APPENDIX Appendix 1. (TTE ICL DATA REVIEW FORM AND
advertisement
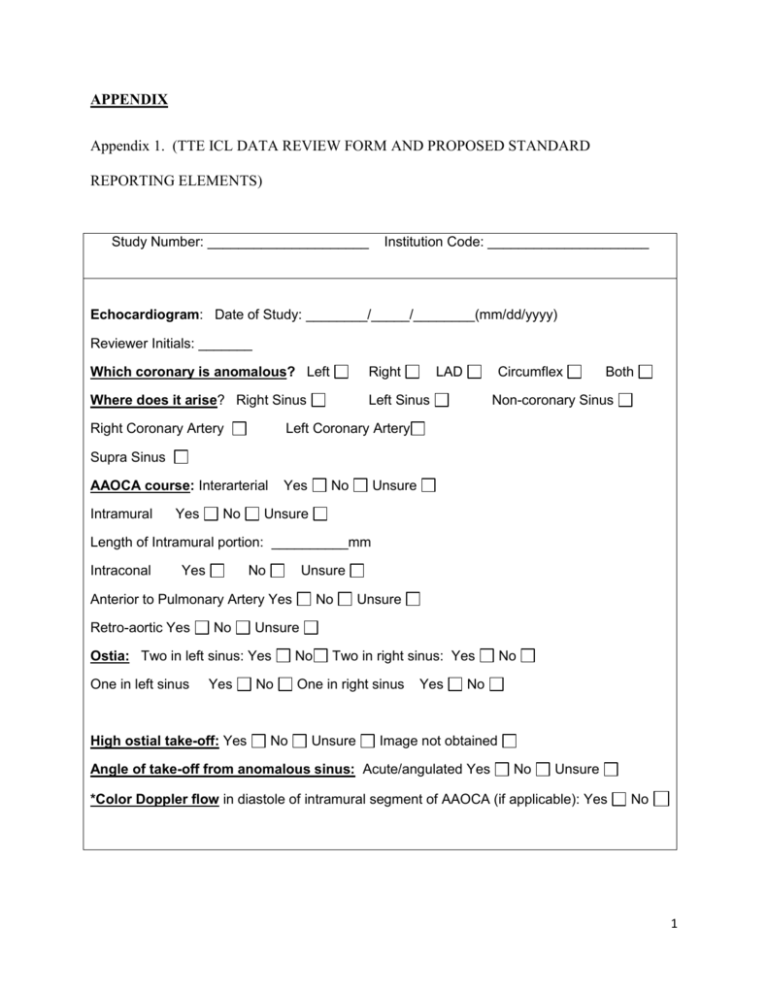
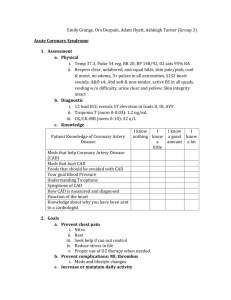
APPENDIX Appendix 1. (TTE ICL DATA REVIEW FORM AND PROPOSED STANDARD REPORTING ELEMENTS) Study Number: _____________________ Institution Code: _____________________ Echocardiogram: Date of Study: ________/_____/________(mm/dd/yyyy) Reviewer Initials: _______ Which coronary is anomalous? Left Right Where does it arise? Right Sinus Left Sinus Right Coronary Artery LAD Circumflex Both Non-coronary Sinus Left Coronary Artery Supra Sinus AAOCA course: Interarterial Intramural Yes No Yes No Unsure Unsure Length of Intramural portion: __________mm Intraconal Yes No Unsure Anterior to Pulmonary Artery Yes Retro-aortic Yes No No Unsure Unsure Ostia: Two in left sinus: Yes No One in left sinus One in right sinus Yes High ostial take-off: Yes No No Two in right sinus: Yes Unsure Yes No No Image not obtained Angle of take-off from anomalous sinus: Acute/angulated Yes No Unsure *Color Doppler flow in diastole of intramural segment of AAOCA (if applicable): Yes No 1 Appendix 2. BEST PRACTICE ECHOCARDIOGRAPHY PROTOCOL FOR PERFORMING TTE AND TEE The goal of this echocardiography protocol is to allow for diagnosis of all of the following 1. Diagnosis of AAOCA 2. Intramural course 3. Interarterial course 4. Intraconal course 5. Position of the ostial origin relative to STJ of the aorta Principles for image optimization In order to best visualize and detail coronary anatomy, high spatial and temporal resolution; use of high-frequency probes and small sector scanning is key. It is recommended to optimize use of grey scale range with dynamic range near 50 decibels, edge enhancement, placement of transmit focus at the region of interest and depth adjustments, adjusting color flow map settings using high color Doppler frequency and optimization of Nyquist limit (near 20-40 cm/s). This allows for visualization of flow in the coronary throughout the cardiac cycle while performing sweeps rather than three beat clips and avoidance of still frame capture. Optimal positioning of the color flow sector also allows for accurate diagnosis by demonstrating antegrade flow from the aortic sinus into the proximal coronary. Additionally positioning the color sector over the interarterial space allows for detection of anomalous coronaries if not noted from standard planes. AAOCA may be difficult to diagnose in real time and obtaining a loop of several seconds and playing them back slowly can help identify the ostia and the proximal course of the coronary arteries. Imaging Views 2 Parasternal short axis imaging (PS SAX) Normal coronary ostia and the proximal course can be demonstrated at the level of the aortic sinuses with the left main coronary artery (LMCA) arising approximately at 4 o’clock (Video1), and the right coronary artery (RCA) arising at approximately 10- 12 o’clock. (Figure 1). For evaluating the interarterial course, subtle clockwise rotation of the transducer from the standard parasternal short-axis and / or angling leftward towards the left shoulder is generally needed (Figure 1, PSSAX-2). The course of the coronary artery in the interarterial space is not necessarily from a standard short axis- plane (Video2, Video3, Video 6, and Video 7). In patients with AAOCA, the ostia may arise more superiorly at or even above the STJ. Multiple beat sweeps in an inferior to superior plane, through the aortic root; need to be performed to demonstrate a high take off. With intramural coronaries, the proximal coronary artery course is acute and makes a <30° angle with the aortic wall and courses parallel to the wall. This can be well demonstrated by color Doppler focusing on the interarterial space. In AAOCA, the anomalous coronary artery may falsely appear to have a normal origin from the appropriate aortic sinus. This area of “takeoff” may be falsely misinterpreted as a normal origin by still frames (Figure 1, (i), (ii), (iii)). The length of intramural segment of AAOCA can be variable. PS SAX imaging will allow imaging the ostia of the AAOCA in relation to the intercoronary commissure (Figure 1 (ii), (iii), (iv) and Video 2, Video 3). Color Doppler evaluation of the ostium and the proximal course should be obtained. The linear diastolic flow parallel or “with in” the aortic wall is an important indicator for an intramural course. (Figure 1 (iv), (v)). Color Doppler can also be helpful in identifying which coronary artery is anomalous. With AAOLCA a blue color Doppler signal will be seen in the anomalous coronary as flow moves away from the right sinus towards the more posterior positioned left 3 sinus of Valsalva (Video 3). This is in contrast to AAORCA, where a red color Doppler signal will be seen in the anomalous coronary as flow moves anteriorly towards the right sinus from its origin in the left sinus (Video 2). An intraconal left main coronary artery (LMCA) or left anterior descending (LAD) can generally be well demonstrated from a parasternal short-axis with the appearance of “muscle” surrounding the proximal coronary artery (Figure 1 (vi), Video 7). Left parasternal long axis imaging (PS LAX) From the PS LAX view, the anomalous coronary coursing between the great arteries can be seen as a discrete circle anterior to the aortic root (Figure 2 (i)). This view also allows demonstration of the coronary origin of an AAOCA in relation to the sinutubular junction via a sweep (Fig 2 (ii), Video 4a, Video 4b, Video 4c, Video 6). Color Doppler flow into the high ostial takeoff should be performed (Video 4b, Video 4c). For intraconal course of the left main coronary (LMCA) or left anterior descending (LAD) a PS LAX sweep angling to the left shoulder demonstrates the intraconal course of the coronary inferior to the pulmonary valve (Video 7). This PS LAX imaging plane may be one or two interspaces lower than usual. Modified Apical From a typical apical four-chamber view, moving the transducer medially and superiorly and tilting it anteriorly (imaging window between a typical parasternal and apical window) will demonstrate the course and length of the anomalous coronary between the two great arteries. (Video 12). This view also will show an intraconal coronary artery inferior to the pulmonary valve annulus (Video 5). The “hammock sign” of the LMCA from the right sinus of Valsalva (as seen on RAO projection by coronary angiography or CTA) can also be obtained from modified apical imaging. Intraconal LMCA coronary artery course can be associated with stenosis, and 4 this should be evaluated with Color Doppler (Figure3 (ii)). Intraconal LAD can be associated with a posterior course of the circumflex coronary artery (Video 10). Imaging the branching pattern and origin in single coronary can also be demonstrated from this view (Figure 3(i)). Sub-xiphoid imaging Children who have good subcostal windows, a sweep from the aortic root more anteriorly to the pulmonary root can help to identify a length of the anomalous coronary running between the great arteries (Video 11). The transesophageal imaging of AAOCA This modality can be particularly useful in adolescents and adults when TTE cannot adequately define the coronary origins. The above principles of imaging equally apply to TEE imaging. The objective is to demonstrate the origin of the AAOCA from the aortic sinus and its proximal course. Optimization of 2D and color Doppler as mentioned above apply. The imaging planes in TEE should be similar to those in TTE in AAOCA. These planes are often modifications of typical TEE imaging planes. Short axis imaging planes to visualize the ostium and its relation to the commissure may be obtained between 25° to 50° (figure 11a, 11b). Long axis imaging of the aorta and STJ at 100°-135° will demonstrate the origin of the anomalous coronary artery in relation to the STJ and its interarterial course (Video 8c, Video 9b). Color Doppler interrogation of the aortic root and interarterial space should be performed as in TTEs. Since the probe is posterior to the heart in TEE compared to anterior in TTE the correspondence between flow and color will be reversed in the anomalous coronary artery. With AAOLCA red color Doppler signal (Video 9a, Video 9b) will be seen in contrast to AAORCA where a blue color Doppler signal will be seen in the anomalous coronary as flow 5 moves away from the TEE transducer towards the right sinus from its origin in the left sinus. (Video 8a, Video 8b, Video 8c). 6