MM Nov 2014 - DNA-TRAP
advertisement

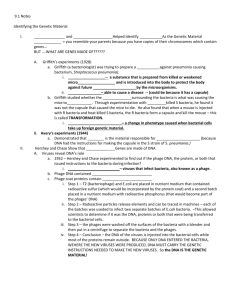
/w EPDw UBMGRk Meet the UK firms at the forefront of drug creation Science 22 October 14 by Stephen Armstrong 8 inShare Sean Freeman This article was taken from the November 2014 issue of WIRED magazine. Be the first to read WIRED's articles in print before they're posted online, and get your hands on loads of additional content by subscribing online. Cinema audiences love an apocalyptic attack: waves of invaders decimating civilisation until a few smart survivors re-establish order. In the real world we've already fought a similar war against a deadly menace, won it -- and then thrown the victory away. The real-life baddies were the micro- organisms causing millions of deaths until, starting in the 40s, scientists cracked their weakness and created thousands of antibiotics. But through over-prescription, the use of antibiotics in farming and patients failing to complete courses of penicillin, the bacteria are fighting back. Chloramphenicol is no longer effective in many parts of the world. Strains of drug-resistant tuberculosis, methicillin-resistant Staphylococcus aureus, multidrugresistant Escherichia coli andKlebsiella pneumoniae are all threats. In May, the Wellcome Trust called for an organisation to catalyse policy across governments. The following month it was announced that antibiotic resistance was the focus of the Longitude Prize (which offers £10m for a cheap, accurate test for bacterial infections). Since then, David Cameron has warned that we risked being "Thrown back into the Dark Ages of medicine." But drug companies have largely given up because of the ROI compared to drugs like Viagra. It was a Brit, Alexander Fleming, who developed penicillin in 1928 to treat bacterial infections -- and today, British researchers are again leading the fight. WIRED meets the people tackling the problem. Procarta Biosystems, Norwich Nanoparticulate delivery of decoy DNA Erik Kriek Bacteria disrupt human cells. Startups disrupt conventional thinking. Procarta twists both together -isrupting the market and micro-organisms with an inventive genetic assault on microbe DNA. Our cells' DNA is the sequencing code for building our body's proteins. When the cell is building, the DNA helix untwists and protein building blocks lock into the correct place. The DNA strand is, effectively, a series of very specific locks -- each protein's key can only slot into one type of lock. For this to work, start and stop signals on the DNA signal how to build the protein. This is known as the promoter region, where a particular molecule called the transcription factor attaches, thus switching on the gene. "We make a decoy -- we fool the transcription factor," Procarta chief scientific officer Michael McArthur explains. "We put that decoy into the cell, the transcription factor binds to the decoy, and then either the bug dies or the disease doesn't happen." Bacteria such as Clostridium difficile resist harsh environments by forming hard outer coats, or spoors, and entering a state of suspended animation. Switching that off makes them vulnerable. Iron regulation is another target -- bacteria need a lot of metal when they enter the human body and have a specific genetic pathway to acquire iron. "If you were a science-savvy investor the first thing you'd say is, 'You're talking about putting in a piece of DNA which is highly negatively charged, prone to biological degradation… how are you going to get that inside the bugs?'" McArthur says. "The clever part of the technology is the nanoparticulate delivery. We have formed a soapy bubble, if you like, around the DNA that carries it safely through the blood. It then finds a bacterium and takes the DNA inside." The Norwich-based company raised seed funding in 2008, with a second round in 2010 led by Morningside Partners. "We intend to stay small for as long as we can," McArthur says. "If you have a technology that's unproven you need to keep it within the family possibly a bit longer to incubate it. When it looks really good is when we start looking for serious business deals." Discuva, Cambridge Using gene manipulation to identify potential new drugs Ryan Inzana "The technology behind sequencing DNA is moving much quicker than Moore's Law," says Discuva CEO David Williams. "In the 90s it would take about a week to derive 100 base pairs of sequence information from DNA. In our lab, we are currently generating one billion 100 base pair sequence reads a day. When you're looking at this many sequences every day, you've got to invent new ways of looking at the data -- so we've had to design new algorithms to look inside it alongside genetic technology that allows us to modify bacteria -- extensively and controllably." This combination of data and genetic mutation so excited pharmaceutical company Roche that, in February 2014, it invested in Discuva -- making an initial commitment of $16 million (£9.4m), plus research fees and payments on other programmes of up to $175 million per product. Discuva has a library of compounds --conventional starting materials that pharma companies use for drug discovery -- which it screens against tens of millions of mutations of target superbugs. Researchers expose each possible mutant to the drug then examine the DNA of those that survive to understand how they've resisted. "That can tell us exactly what component inside the cell the compound is binding to and affecting, and it can tell us what all the potential resistance mechanisms could be for that compound," Williams says. "That's really important because we don't want to develop new antibiotics that are going to develop resistance quickly in the clinic." The Discuva team were all working in pharma when they met at a barbecue in 2009 and decided to found a company. It took two years to achieve funding but the company has grown fast, with its most advanced programme now roughly two years away from obtaining a patent. "There are fewer than 20 chemotypes of antibiotics on the market currently, with not many following behind," according to Williams. "We've got 3,000 completely new chemotypes just waiting to go." Cycle, Cambridge Discovering new treatments using old pharmaceuticals Angie Wang Cycle's approach is to combine existing drugs in order to explore previously discarded aggregations, new combinations or versions of previously toxic doses that can be made safe for humans. "Reviving existing drugs is much less risky than trying to discover new ones, both financially and in terms of patient safety," according to Cycle CEO James Harrison. "The drug discovery pipeline is a lottery -the chances of success are very small. Some of the drugs we're looking at have years of safety data behind them. There are lots of drug files with all the relevant safety and clinical trial data collecting dust. We're effectively recycling them." Harrison came to antibiotics via finance. He studied chemistry at Cambridge but joined Soros Private Equity Partners' mergers and acquisitions team via a postgraduate job at Morgan Stanley. He ended up becoming the CEO of a business he helped acquire for Soros -- drug-component maker Archimica --and moved to Germany and then Switzerland for three years to run the company. He founded Cycle in 2012 with a team of pharmaceutical industry veterans from companies such as Eli Lilly, Novartis and AstraZeneca. They signed an agreement with the UWM Research Foundation to research new uses for nitisinone -- a drug marketed to treat a rare genetic disorder, hereditary tyrosinemia type 1. Nitisinone also inhibits pyomelanin, a pigment used by many species of bacteria -including the Legionnaires' disease infector Legionella pneumophila. The bugs use it to protect against light and free radicals and to absorb metals essential for cell reactions. It's a good example, James explains, of drugs we already know that can be reconsidered. Others include drug combinations tried successfully in developing countries where there isn't access to newer medicines. "We have former US and EU drug regulatory officers on our staff, so we know what regulators require," he says. "Our background is also in drug manufacturing, so we know how to put supply chains in place and manage them. Many pharmaceuticals are not optimised for patients and we're trying to do something about this. There is an ethical component to our work -- we want to do well by doing good." Phico Therapeutics, Cambridge Hijacking viruses that hunt and kill bacteria Ben Oliver Phico is undertaking trials that could establish a hunter-killer virus that's a powerful human ally in the real world. Its drug is based on phage therapy -- a 1920s technique from the Soviet Union that exploits the constant war between bacteria and viruses. Although those with a nasty cold might not appreciate the subtlety, a virus isn't technically a living thing; it's a strand of DNA wrapped in proteins that help it penetrate cell walls and enter the heart of living things. All bacteria have natural viral enemies which specialise so precisely in infecting bacteria that they cannot infect humans. Phico's trick is to hijack a virus and use it to inject a small, acid-soluble protein (SASP) that shuts down DNA replication. After studying SASPs in the US, CEO Heather Fairhead founded Phico in 2000 with seed funding from Cambridge Research and Innovation Ltd and has since raised £14 million from a variety of grants and partners. The 16-person startup is based at the Babraham Research Campus and includes nine post-doctoral scientists. "We're a small company so we're resource-limited," says Fairhead (right). "We focus on higher value, higher medical-need products for serious infections." The Pseudomonas aeruginosa hospital pathogen -- a common cause of pneumonia -- is first. It's difficult to treat and perhaps the most resistant of all bacteria, but SASP works irrespective of that. Fairhead expects the first Phico drug to come on to the market in about four years with variants for E.coli and Klebsiella pneumoniae to follow -- although the UK may emulate the US and afford clinical programmes help in getting drugs to market sooner. Demuris, Newcastle Exploiting "good" bacteria for new treatment Guy Shield If there is such a thing as a serial antibiotic entrepreneur, Jeff Errington, scientific founder of Demuris and director of the Institute for Cell and Molecular Biosciences at Newcastle University, would be it. Errington's first startup, Prolysis, was sold in 2009 following research done at the University of Oxford into bacterial cell biology. By the time Australian drug company Biota Holdings bought it, Errington had already moved on. His new company Demuris is moving forwards by going back -- right back to the roots of the first wave of antibiotics, produced in the battles between micro-organisms in the natural world. "We've been lucky enough to acquire an enormous library of actinomycetes [from Michael Goodfellow at Newcastle University who collected examples of bacteria], which account for two thirds of all known microbial natural products," says Errington (below). "Goodfellow's collection of more than 7,000 strains has been built up by more than 100 graduate, postgraduate and post-doctoral scientists over a 35-year period, from the bottom of the ocean to the top of mountains. It's unparalleled in diversity and quality of its content." Actinomycetes are the "good" bacteria -- with one genus, Streptomyces, producing various natural anti-fungal, anti-parasitic and immunosuppressant drugs. Errington believes only about ten per cent of the total number of natural products that can be synthesised by these organisms have been discovered. His team is working in a combination of its own labs and those at Newcastle University. "It used to be the case that academics and the private sector rarely spoke," Errington says. "The future is all about collaboration." Amura, Madingley, Cambridgeshire Combating bacteria by interfering with enzymes Ethan Rilley Cambridgeshire-based Amura has found itself in a strange position: while working on an antibiotic, it developed a new technology that is financially more productive than the antibiotic itself. The team is currently looking for development partners to help restart the original antibiotic programme, which is languishing under the research name AM-112. The first wave of antibiotics was designed with a common chemical structure -- a four-atom ring known as beta-lactam. One technique bacteria have developed for resisting these drugs is producing a powerful enzyme that cracks this ring open, subsequently breaking the drug down. AM-112 is the first in a new generation of drugs -- called oxapenems -- that block bacteria's ability to make that enzyme, with the upshot that old-school penicillin becomes effective again. Alongside developing the oxapenems, Amura is using its proprietary technology platform AMcore to target cysteine proteases -- nzymes which are produced by parasites such as malaria and are crucial to their survival. Develop a drug that inhibits these enzymes and it would be a powerful anti-malarial. Absynthe Biologics, Sheffield Enabling the immune system to recognise and react to MRSA Alexander Wells Absynth Biologics has become a world leader in new forms of immunisation against the toughest superbug -- Methicillin-resistant Staphylococcus aureus (MRSA). The bacterium's assault of the human immune system is complex and challenging to combat. Typically, infection of any kind weakens the host's immune defence system in two ways: first, foreign invaders such as viruses trigger a wave of protein antibodies and attack white blood cells that shut down then devour the invader; at the same time, dendritic cells carve up the invader and take the pieces to the body's lymph nodes. Here, the body creates killer molecules, while storing the memory of the attacker's protein ID. The adaptive system is slow first time round -- but its attack "memory" means a second infection is dealt with swiftly and mercilessly. Absynth chief executive Fiona Marston (top left) explains that MRSA switches off an aspect of the adaptive system -- meaning that each MRSA infection is, as far as the body is concerned, its first. "It can remain invisible to your defence system," she says. "The pressure on the immune systems of older or sicker patients can prove fatal." Absynth is developing a vaccine that mimics proteins in the virus's cell wall, meaning the immune defence system learns to recognise and react to its presence. The vaccine, in effect, de-cloaks the MRSA. Marston has more than 25 years' experience in healthcare and biotechnology, from cofounding Novacta Biosystems to working as an investor for Rothschild. Founded in 2007 and based on discoveries by Professor Simon Foster (above right) and Dr Jorge Garcia-Lara, Absynth has secured £1m in seed capital from Fusion IP. Marston predicts the company will deliver future vaccines against a range of viruses. Novactal | Cantab, Cambridge Tackling superbugs with species-specific drugs Ricardo Bessa Novacta's major backer -- life-science private-equity firm Celtic Pharma -- invested in 2005. As Novacta's new antibiotics -- known as lantibiotics -- reached trial stage, Celtic encouraged the team to spin out a new company, Cantab, to rejuvenate a drug class abandoned in the 40s, the polymyxins. ¶ Lantibiotics come from the microbes' own weapon systems, according to Novacta's chief scientific officer (and Cantab CEO) Mike Dawson (below). The company's two new drugs -- NVB302 and NVB333 -- are species-specific, attacking the formation of cell walls in Clostridium difficile and Staph aureus respectively. NVB302 is in first-stage clinical trials and could come to market within five years. Since 2012, the team's lab research has been focused on the polymyxins. These target gram-negative bacteria such as E. coli, Salmonella, Legionella, gonorrhoea and acinetobacter. In June 2012, the US passed the Generating Antibiotic Incentives Now -- or GAIN -- act. The US Food and Drug Administration can fast-track new antibiotics and extend drug companies' exclusive licences for five years. Dawson believes Cantab's drugs will benefit, but points out that no equivalent UK legislation is being discussed. Stephen Armstrong wrote about the BBC Natural History Unit in 03.14. Details of the Longitude Prize 2014 are at longitudeprize.org