Prenatal & Perinatal Care
advertisement
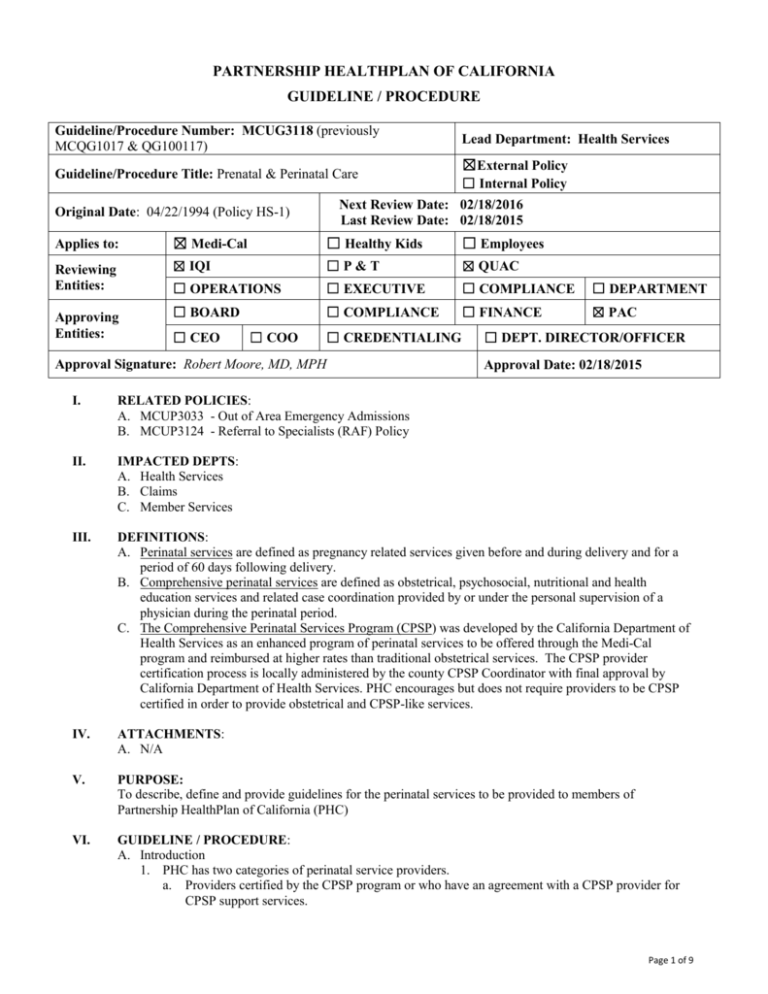
PARTNERSHIP HEALTHPLAN OF CALIFORNIA GUIDELINE / PROCEDURE Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Guideline/Procedure Title: Prenatal & Perinatal Care Lead Department: Health Services ☒External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Last Review Date: 02/18/2015 Original Date: 04/22/1994 (Policy HS-1) Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☐P&T ☒ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Approving Entities: ☐ CEO ☐ COO ☐ CREDENTIALING Approval Signature: Robert Moore, MD, MPH ☐ DEPT. DIRECTOR/OFFICER Approval Date: 02/18/2015 I. RELATED POLICIES: A. MCUP3033 - Out of Area Emergency Admissions B. MCUP3124 - Referral to Specialists (RAF) Policy II. IMPACTED DEPTS: A. Health Services B. Claims C. Member Services III. DEFINITIONS: A. Perinatal services are defined as pregnancy related services given before and during delivery and for a period of 60 days following delivery. B. Comprehensive perinatal services are defined as obstetrical, psychosocial, nutritional and health education services and related case coordination provided by or under the personal supervision of a physician during the perinatal period. C. The Comprehensive Perinatal Services Program (CPSP) was developed by the California Department of Health Services as an enhanced program of perinatal services to be offered through the Medi-Cal program and reimbursed at higher rates than traditional obstetrical services. The CPSP provider certification process is locally administered by the county CPSP Coordinator with final approval by California Department of Health Services. PHC encourages but does not require providers to be CPSP certified in order to provide obstetrical and CPSP-like services. IV. ATTACHMENTS: A. N/A V. PURPOSE: To describe, define and provide guidelines for the perinatal services to be provided to members of Partnership HealthPlan of California (PHC) VI. GUIDELINE / PROCEDURE: A. Introduction 1. PHC has two categories of perinatal service providers. a. Providers certified by the CPSP program or who have an agreement with a CPSP provider for CPSP support services. Page 1 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care b. Those who are contracted with PHC to provide comprehensive perinatal services, but who are not CPSP certified providers, but do provide CPSP like services. 2. PHC’s contract with the California Department of Health Care Services (DHCS) requires contracted providers to follow current American College of Obstetrics & Gynecology (ACOG) standards as the minimum standards for services to PHC’s pregnant women. In addition, all obstetrical practitioners are required to provide a comprehensive initial risk assessment that includes medical nutrition, health education and psychosocial risks, on all pregnant women at the initiation of pregnancy related services. Formal re-assessments must be offered in each subsequent trimester and in the postpartum period. All identified risk conditions must be followed up by interventions designed to eliminate or remedy the condition or problem in a prioritized manner. Individualized care plans must be developed to include obstetrical, nutritional, health education and psychosocial interventions when indicated by identified risk factors. All services/resources provided must be clearly documented on the Care Plan in the member’s medical record each trimester. Non-CPSP Obstetrical providers must have an agreement with a certified CPSP provider to provide comprehensive support services. A non-CPSP provider may choose to use a trained staff person to administer the comprehensive risk assessments and to make referrals to the CPSP program for interventions and completion of care plans. A specific billing code is available to bill for administration of assessments by non-CPSP providers. B. Program Goals 1. To make comprehensive perinatal services accessible to all pregnant PHC members. 2. To assure all members initiate prenatal care within the first twelve (12) weeks of pregnancy and pregnant members who are new to the HealthPlan obtain prenatal care within forty-two (42) days after enrollment in the Plan. 3. To support and expand the range of comprehensive perinatal services provided to PHC members. 4. To strongly encourage obstetrical providers to become CPSP certified providers or to have an agreement with a CPSP provider to provide support services. 5. To inform all PHC members about the availability of comprehensive perinatal services and the added benefits of these programs. 6. To assist members with enrollment into comprehensive perinatal services programs. 7. To increase provider awareness of comprehensive perinatal services and the potential benefits for pregnant members. C. Perinatal Service Providers 1. In general, perinatal service including antenatal care, labor and delivery services should be provided by perinatal providers who deliver at the hospital associated with the member’s primary care physician’s capitated agreement. Exceptions to this include emergency deliveries and hospital admissions authorized according to the Out of Area Admissions policy, members determined to be high risk who require the services of a perinatologist, and pregnant women who are not assigned to a primary care physician because they are in a special member category. 2. OB/GYN providers are expected to refer pregnant women to PHC’s Growing Together Perinatal Program (GTPP) for voluntary enrollment. Those members determined to be high risk will be assigned a PHC Care Manager who will provide care management support throughout the pregnancy. 3. All providers of perinatal services must deliver services in conformance with the following: a. Current ACOG Standards for Obstetric-Gynecologic Services, (available from the American College of Obstetricians and Gynecologists, 600 Maryland Avenue, Southwest, Suite 300 East, Washington, DC 20024). Page 2 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care b. Newborn Screening Regulations as set forth in Title 17, California Code of Regulations, Section 6500 et seq. c. Hemolytic disease of the Newborn Requirements as set forth in Title 17, California Code of Regulations, Section 6510 et seq. d. Title 22 regulations; Title 17 regulations and all applicable sections of the Health and Safety Code. e. The California Prenatal Screening Program. 4. Perinatal service providers include all of the following practitioners for the purpose of providing perinatal services: a. Physicians who are general practitioners, family practice physicians, pediatricians, or obstetrician-gynecologists b. Certified Nurse Midwives c. Nurse Practitioners d. Physician Assistants e. Registered Nurses, Social Workers, Health Educators, Childbirth Educators, Registered Dietitians, Perinatal Health Workers, or LVNs D. Referral Procedures 1. Obstetrical services do not require a Referral Authorization Form (RAF) by the PCP. Members assigned to a multi-specialty group (Kaiser, or Woodland Health Care) must obtain perinatal services through that entity. Members assigned to PCPs must obtain obstetrical care from a perinatal provider associated with the same hospital affiliation as the member’s PCP. Members not assigned to a PCP may obtain OB services from any provider within their county of residence Members not assigned to Woodland or Kaiser may obtain OB services from any Medi-Cal contracted provider, but are strongly encouraged to obtain services from a PHC contracted perinatal provider. 2. It is the responsibility of the perinatal provider to confirm the member's eligibility and PCP information from the Plan at each visit. Page 3 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care E. Perinatal Care Guidelines Requirement Preconception Care: physical exam and medical history, family planning and pregnancy resources, folic acid prescription, cessation of smoking, alcohol and drug use, and domestic violence/abuse. Pregnancy Test as soon as period is missed or if woman had unprotected intercourse. Initial history and physical exam As soon as pregnancy is detected. A prenatal visit should be available within one week upon request. First Trimester (0-12 weeks) Second Trimester (13-23 weeks) Third Trimester (24 – 40 weeks) Postpartum Period (delivery to 8 weeks) Complete medical history. Complete physical exam including pelvic and breast exam. Prescribe prenatal vitamin with folic acid. Establish estimated date of delivery. Page 4 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care Requirement First Trimester (0-12 weeks) Comprehensive assessment and reassessments with referral for support services as indicated. Initial comprehensive assessment: psycho-social, health education and nutrition. Provide and document referral to WIC Program. (Title 42) Mandatory referrals: - Dental Care - Genetic Screening - Family Planning - WIC - CHDP The frequency and regularity of scheduled prenatal visits should be sufficient to enable providers to accomplish the following activities: 1. Monitor the progression of the pregnancy 2. Provide education and recommended screening and interventions 3. Reassure the mother 4. Assess the well-being of the fetus and mother Prenatal exam Schedule for low risk pregnancy. Women with medical problems and younger teens may require more frequent visits Second Trimester (13-23 weeks) Reassessment: psycho-social, health education and nutrition Third Trimester (24 – 40 weeks) Reassessment: psycho-social, health education and nutrition See first trimester See first trimester Generally, ACOG recommends every four weeks: same as in first trimester with the addition of questions about fetal movement contractions, leakage of fluid or vaginal bleeding. Generally, ACOG recommends after 28 weeks, every two weeks. After 36 weeks, every week. Postpartum Period (delivery to 8 weeks) Postpartum Reassessment: psycho-social, health education and nutrition Approximately 4 to 6 weeks after delivery: pelvic exam, breast and abdomen exam, weight, blood pressure. If cesarean delivery or complicated gestation, an additional visit may be needed within 7-14 days. Page 5 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care Requirement First Trimester (0-12 weeks) Prenatal exam Schedule for low risk pregnancy. Women with medical problems and younger teens may require more frequent visits. 5. Detect medical and psychosocial complications and institute indicated interventions. Generally, ACOG recommends every four weeks, exam includes blood pressure, weight, urine protein and glucose, measurement of uterus, fetal heart rate. Second Trimester (13-23 weeks) Third Trimester (24 – 40 weeks) Postpartum Period (delivery to 8 weeks) Page 6 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care Requirement Screening tests recommended First Trimester (0-12 weeks) Pap smear, gonorrhea, Chlamydia (required for pregnant women ages 16-26 yrs) syphilis, hepatitis B, Hematocrit or hemoglobin levels, MCV and, Platelets, blood type, antibody screen, rubella test, urinalysis, Mantoux TB test, quantitative gamma interferon test (IGRA), HIV test must be discussed and offered. Early diabetes screen if family history, history of large baby or gestational diabetes, hypertension, or if mother is 30 years of age or older. Second Trimester (13-23 weeks) AFP test 15-18 weeks, other genetic tests as indicated. An ultrasound may be indicated to determine the due date or if the baby is not growing at the normal rate. Third Trimester (24 – 40 weeks) Diabetes screen, anemia tests 24-28 weeks, HIV test may be repeated at 24-28 weeks, tests for sexually transmitted diseases may be repeated at 32-36 weeks if indicated. Antibody test should be repeated at 28 weeks if RH negative. Immune globulin should be given at this time if indicated. Consider screening for Group B Beta Strep at 35-37 weeks. Sometimes a non-stress test or contraction stress test may be needed to assess fetal well-being. Postpartum Period (delivery to 8 weeks) Pap smear, anemia check, birth control prescription Page 7 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care Requirement Education topics recommended First Trimester (0-12 weeks) Danger signs, how to reach your doctor. Schedule of visits, use of safety belts, Nutrition and weight gain, exercise guidelines, smoking cessation, HIV counseling, alcohol and substance abuse education, domestic violence. Second Trimester (13-23 weeks) Pre-term labor signs, danger signs, when to call. Third Trimester (24 – 40 weeks) Kick counts, signs of labor, labor and delivery preparation, planning for discharge and child care, breastfeeding education and resources, postpartum self care, family planning, resources for home health after discharge. Newborn care, cord care, jaundice and circumcision. Identification of pediatric provider. Postpartum Period (delivery to 8 weeks) Family planning, evaluation of family planning, newborn care, sleep position. Confirm participation in WIC Program from initial referral. Postpartum depression. Reevaluate breast feeding concerns. F. CPSP Case Management Responsibilities 1. The CPSP case manager is expected to plan and ensure the provision of comprehensive perinatal services, including nutrition, health education, and psychosocial assessments and reassessments, individualized care plan development, coordination of services, and referrals. 2. The CPSP case manager must assure that the following has been provided to the member and documented in the medical record: 3. An orientation per CPSP guidelines about the services which have been offered, who will provide the services, the locations for service delivery, warning signs and symptoms, office procedures, and purpose of the program. a. Information about the available adjunctive referral services available to the member. b. Advice about the member’s rights and responsibilities in accepting or refusing the services offered. c. Notification regarding CPSP provider and PHC appeal and grievance policies. d. An offering of the initial nutrition, health education and psychosocial assessments, and individualized care plan development, as well as re-assessments in each trimester and postpartum assessments including both individual and group interventions for each service as recommended in the individualized care plans. e. Documentation of referrals to services which are not specifically included in the definition of comprehensive perinatal services, but which are appropriate for the medical and/or psychosocial health of the member, should be noted in the record by the CPSP case manager. Page 8 of 9 Guideline/Procedure Number: MCUG3118 (previously MCQG1017 & QG100117) Lead Department: Health Services ☒ External Policy ☐ Internal Policy Next Review Date: 02/18/2016 Original Date: 04/22/1994 (Policy HS-1) Last Review Date: 02/18/2015 Applies to: ☒ Medi-Cal ☐ Healthy Kids ☐ Employees Guideline/Procedure Title: Prenatal & Perinatal Care 4. The CPSP case manager must use orientation, assessments, re-assessments, individual and group process interventions and family support participation as methods for the provision of comprehensive perinatal services. 5. The perinatal provider must document his/her assessment of the member's obstetrical status at each visit. 6. Each component of the individualized care plan should identify risk conditions; prioritize the member's needs, referrals, and proposed interventions including methods, time frames and outcome objectives for psychosocial, health education, and nutrition services. The member's needs are to be reassessed and the individualized care plan revised as necessary at least each trimester and at the post-partum visit. 7. A member has the right to decline to participate in any part of the Comprehensive Perinatal Services Program. This should be documented clearly in the medical record. 8. CPSP providers must submit a TAR to PHC for the provision of services in excess of the PHC maximum frequency allowance for nutrition, psychosocial and health education services, as established in Title 22, CCR, Section 51504. 9. CPSP providers must submit a list of any staff changes within one month of the change to the county CPSP Coordinator. VII. REFERENCES: A. Guidelines for Perinatal Care –7th Edition. American College Obstetricians & Gynecologists VIII. DISTRIBUTION: A. Provider Manual B. OB/Gyn practice sites C. PHC Department Directors IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Senior Director, Health Services X. REVISION DATES: (HS-1 - 12/10/96; 10/10/97 [name change only]; 02/17/99; 06/21/00, 10/17/01; 06/19/02; 10/20/04; 04/20/05; 05/18/05; 05/17/06; 08/15/07; 08/20/08; 06/17/09; 01/16/13; 03/19/14; 09/17/14; 02/18/2015 PREVIOUSLY APPLIED TO: ********************************* In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: Consistent with sound clinical principles and processes Evaluated and updated at least annually If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC. Page 9 of 9