Journal Club GVHD prophylaxis with ATG-F
advertisement
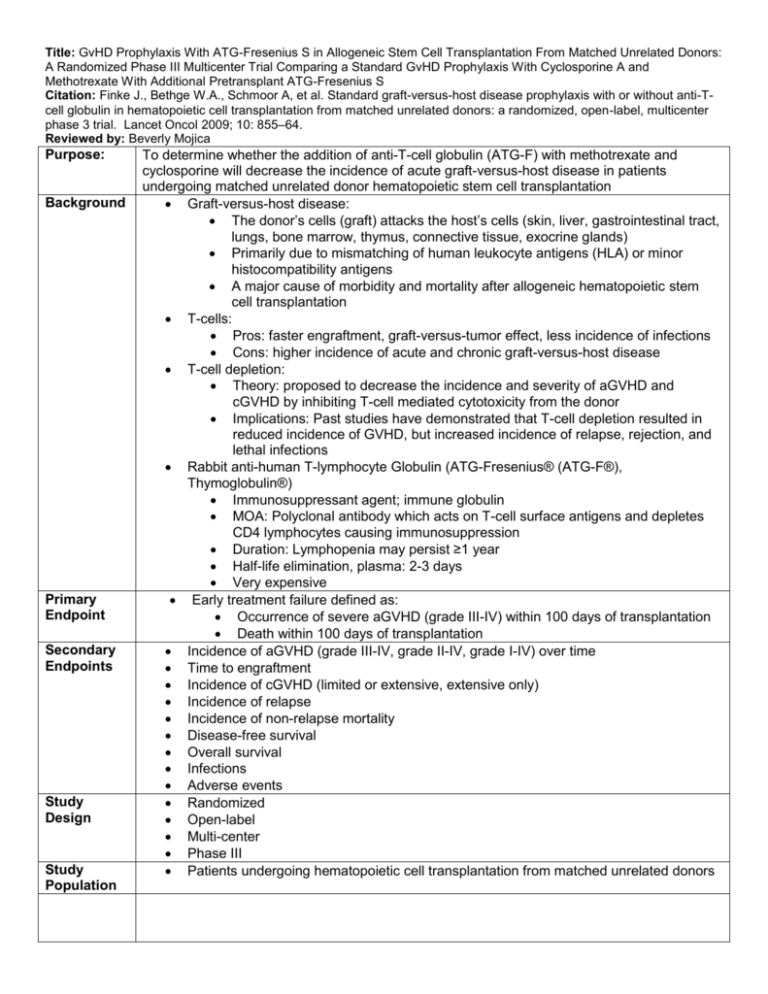
Title: GvHD Prophylaxis With ATG-Fresenius S in Allogeneic Stem Cell Transplantation From Matched Unrelated Donors: A Randomized Phase III Multicenter Trial Comparing a Standard GvHD Prophylaxis With Cyclosporine A and Methotrexate With Additional Pretransplant ATG-Fresenius S Citation: Finke J., Bethge W.A., Schmoor A, et al. Standard graft-versus-host disease prophylaxis with or without anti-Tcell globulin in hematopoietic cell transplantation from matched unrelated donors: a randomized, open-label, multicenter phase 3 trial. Lancet Oncol 2009; 10: 855–64. Reviewed by: Beverly Mojica Purpose: Background Primary Endpoint Secondary Endpoints Study Design Study Population To determine whether the addition of anti-T-cell globulin (ATG-F) with methotrexate and cyclosporine will decrease the incidence of acute graft-versus-host disease in patients undergoing matched unrelated donor hematopoietic stem cell transplantation Graft-versus-host disease: The donor’s cells (graft) attacks the host’s cells (skin, liver, gastrointestinal tract, lungs, bone marrow, thymus, connective tissue, exocrine glands) Primarily due to mismatching of human leukocyte antigens (HLA) or minor histocompatibility antigens A major cause of morbidity and mortality after allogeneic hematopoietic stem cell transplantation T-cells: Pros: faster engraftment, graft-versus-tumor effect, less incidence of infections Cons: higher incidence of acute and chronic graft-versus-host disease T-cell depletion: Theory: proposed to decrease the incidence and severity of aGVHD and cGVHD by inhibiting T-cell mediated cytotoxicity from the donor Implications: Past studies have demonstrated that T-cell depletion resulted in reduced incidence of GVHD, but increased incidence of relapse, rejection, and lethal infections Rabbit anti-human T-lymphocyte Globulin (ATG-Fresenius® (ATG-F®), Thymoglobulin®) Immunosuppressant agent; immune globulin MOA: Polyclonal antibody which acts on T-cell surface antigens and depletes CD4 lymphocytes causing immunosuppression Duration: Lymphopenia may persist ≥1 year Half-life elimination, plasma: 2-3 days Very expensive Early treatment failure defined as: Occurrence of severe aGVHD (grade III-IV) within 100 days of transplantation Death within 100 days of transplantation Incidence of aGVHD (grade III-IV, grade II-IV, grade I-IV) over time Time to engraftment Incidence of cGVHD (limited or extensive, extensive only) Incidence of relapse Incidence of non-relapse mortality Disease-free survival Overall survival Infections Adverse events Randomized Open-label Multi-center Phase III Patients undergoing hematopoietic cell transplantation from matched unrelated donors Inclusion Criteria Exclusion Criteria Intervention (Total n = 202) Statistical Analysis Patient Population Age 18-60 years of age Karnofsky performance score of > 60% Acute Leukemia in first complete remission or beyond first remission, in relapse, or not in remission (primary refractory , induction failure) Chronic myeloid leukemia beyond first chronic phase Myelodysplastic syndrome Myelofibrosis Donors and recipients required to be HLA-compatible (10/10 matches) Patients with a HLA-A, -B (DNA-based, 2 digits), HLA-DRB1, -DQB1 (DNAbased 4 digits) matched (8 out of 8 alleles) unrelated donor Significant disease: Heart failure with ejection fraction (EF) <50% Pulmonary (forced expiratory volume in 1 s <50%) Renal (Scr > 1.5 mg/dL) Metabolic (bilirubin > 2 mg/dL) CNS disease currently uncontrolled by treatment Infections currently uncontrolled with antimicrobials Carriers of hepatitis B surface antigen, hepatitis C antibody, or HIV Additional concurrent or previous malignant disease History of hypersensitivity to rabbit immunoglobulin antibodies Previous transplantation, including autologous transplants Pregnant or lactating women Treatment arm (n=103): ATG-Fresenius S (20 mg/kg body weight at days -3 to -1 (total dose: 60 mg/kg) Cyclosporine A (target trough level > 200ng/ml (day -1 until day +100) Methotrexate: 15mg/m2 at day +1, 10mg/m2 at days +3, +6, and +11 Control arm (n=99): Cyclosporine A (target trough level > 200ng/ml (day -1 until day +100) Methotrexate: 15mg/m2 at day +1, 10mg/m2 at days +3, +6, and +11 Conditioning regimens differed across the study centers: Total body irradiation (8-12 Gy) Busulfan (14-16 mg/kg orally or equivalent for IV administration) plus cyclophosphamide (2 x 60 mg/kg) or etoposide Regimens consisting of Thiopeta (>15 mg/kg) or Carmustine (>300 mg/m2) 80% power to detect significant difference in early treatment failure between the ATG-F group and control group, requiring 176 and 192 participants, respectively Intention-to-Treat Analysis Per-Protocol Analysis Safety Analysis A logistic regression model was used to adjust for differences (disease status, study center stratification, stem-cell source) Used to calculate the odds ratio (OR) with a 95% CI A Cox regression and Fine and Gray models were used to adjust for disease status (e.g. early v. advanced) and stem-cell source (e.g. bone marrow vs. peripheral blood) Used to calculate the hazard ratios (HR) with 95% CI Similarities: Average age: 40 years Sex distribution equivalent Ethnic origin (Caucasian) Performance status Differences: -More advanced disease status in control group -More seropositive CMV in ATG-F group -More HLA-C mismatch in ATG-F group Results Primary Endpoint aGVHD or death within day -100 Treatment (ATG-F) 21.4% (95% CI 13.4-29.3) Odds Ratio 0.59 (95% CI 0.301.17; p= 0.13) 33.7% (95% CI 24.343.0) Comment(s) Reduction in early treatment failure was found in the ATG-F group NNT=8 Adjusted Hazard Ratio (HR) 0.61 (95% CI 0.43-0.88; p=0.007) Comment(s) 2-year cumulative incidence of cGVHD (limited or extensive) 2-year cumulative incidence of nonrelapse mortality 0.34 (95% CI 0.21-0.55; p< 0.0001) Significant reduction in cGVHD with ATG-F NNT= 4 0.68 (95% CI 0.38-1.22; p=0.20) Lower incidence of non-relapse mortality with ATG-F, but not significant NNT= 11 2-year cumulative incidence of relapse 1.18 (95% CI 0.69-2.03; p=0.55) 0.91 (95% CI 0.62-1.36; p=0.65) 0.86 (95% CI 0.57-1.30; p=0.47) Slightly higher incidence of relapse with ATG-F, but not significant NNH= 17 Slightly higher disease-free survival with ATG-F, but not significant NNT= 24 Higher over survival found in ATG-F group, but not significant NNT= 14 Secondary Endpoints Cumulative incidence of grade I-IV aGVHD 2-year disease-free survival 2-year overall survival rate Safety Endpoints Control Infections Bacterial (staph., strep., clostridium) Fungal (Candida spp.) Parasitic Viral (CMV, HSV) CMV infection Epstein-Barr virus post-transplant disorder (EBVPTLD) Significant reduction in aGVHD with ATG-F NNT=6 Treatment 62.3% Control 68.4% 33.0% 2.8% 74.5% 53.8% 37.9% 6.3% 64.2% 29.5% 4.8% 1.0% Comment(s) Similar Similar Similar Higher rate of seropositive CMV in treatment (62.3%) vs. control (40.0%) Adjusted HR for CMV infection: 1.53 (95% CI 0.96-2.44; p=0.08) NNH=4 Regular EBV monitoring should be done Adverse Events Mucosal inflammation Pyrexia Treatment 68.9% 68.9% Control 72.6% 56.8% Hypertension Diarrhea Headache 55.7% 53.8% 41.5% 51.6% 50.5% 30.5% Chills 31.1% 13.7% Renal failure Abdominal pain 21.7% 19.8% 17.9% 25.3% Conclusion Strengths Limitation Clinical Relevance Comment(s) Similar More often in ATG-F group NNH=8 Similar Similar More often in ATG-F group NNH= 9 More often in ATG-F group NNH=5 Similar Similar Study conclusion: The addition of ATG-F to standard GVHD prophylaxis regimen significantly decreased the incidence of aGVHD and cGVHD, without having a negative effect on survival or increasing the relapse or non-relapse mortality. Randomization Concealment ITT analysis Analyzed efficacy and safety data Covariate analysis was used to adjust for differences Considered clinically important outcomes Good follow-up Open-label Multi-center trial Unequal treatment Differences in some baseline characteristics Quality of life not measured Cost of treatment was not considered Study was funded by Fresenius Biotech GmbH Longer-follow up needed for cGVHD Only studied Caucasians The advantages and disadvantages of in-vivo T-cell depletion with ATG-F should be considered in the prophylaxis of GVHD The following factors should be considered: Risk for infection Risk for relapse Degree of mismatch Age of patient Cost of treatment Quality of life The addition of ATG-F to standard GVHD prophylaxis regimen should be reserved for: Those at higher risk for GVHD (e.g. unrelated donor, mismatched allogeneic stem cell transplantation) Those at low-risk for relapse (e.g. patient responded to induction chemotherapy, patient was in remission at the time of transplantation) A study investigating the addition of ATG-F to Tacrolimus and Sirolimus will provide better insight as to the clinical application of ATG-F for patients at City of Hope.