evidence_base_paper final
advertisement
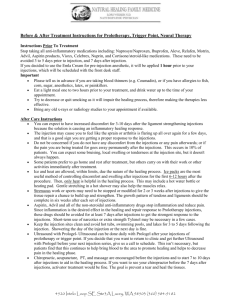
This paper will discuss the extent to which evidence guides the nursing practice. As well as examines and discusses a nursing practice and intervention related to a specific client that was cared for in the hospital setting. Client Scenario M. J, is a 20 year old female admitted to the hospital for surgery on February 20, 2009 at 0700 for a breast augmentation. M.J states she chose to get this elective surgery done for personal reasons because she felt by having this surgery she would improve her appearance which would ultimately improve her self confidence. M.J’s records show she has had a past history of having surgery and being hospitalized in 1997 where she got her appendix removed because of appendicitis, and the surgery was completed without any compilations. She has no other health issues that she is aware of at the time, and considers herself to be a healthy individual. After being admitted to the hospital on February 20, M.J was a little nervous before surgery; however, had her mother by her side to comfort her. At 0730, M.J was taken from 3B to the operating room and returned from surgery at 0940 where she was drowsy, but responsive. There were no concerns during the procedure .... Her vitals were stable during the initial assessment and stayed steady during the remaining vital checks. M.J felt no nausea or vomiting, rated her pain as minimal and the dressing remained dry and intact with no drains in place during her stay in the hospital. She was able to stomach crackers and was drinking water, so within two hours of being on the unit her intravenous of normal saline was discontinued. At 1230 her discharge teaching was completed and at 1300 she left the unit with her mother at her side. There were no concerns during the surgery, as well as when she was brought back to the unit. Nursing Intervention and related health issue Intramuscular injections are quite common, however evidence shows there have been various complications related with them (Floyd & Meyer, 2007). Complications from intramuscular injections were mostly from inadequate knowledge of the procedure and not using the proper techniques to administer injections into the ideal site (Small, 2007). The best site to administer intramuscular injects has been discussed in numerous articles. Evidence shows that the dorsogluteal should be avoided for most medications and Greenway, Merriman, and Statham (2006) recommend using the ventrogluteal site as the top choice for administering intramuscular injections. The ventrogluteal site should be the site of choice for many reasons. It is a large, well-defined muscle, which is surrounded by a consistent layer of subcutaneous fat (Greenway, Merriman & Statham, 2006) and lacks main blood vessels and nerves (Floyd & Meyer, 2007). Not only are the chances of hitting a blood vessel or nerve less than the dorsogluteal, but land marking for the injection is easy to locate, and the positioning of the patient can be individualized depending on their condition and whether they prefer sitting, standing or lying down (Greenway, Merriman & Statham, 2006). Compared to the dorsogluteal, the ventrogluteal provides a thicker muscle and more consistent thinness of adipose tissue, which ultimately reduces the need to figure out the depth of subcutaneous fat because it is usually less than 3.75 cm (Greenway, 2004). By using the ventrogluteal injection site the nurse can be sure that the medication will penetrate the muscle and not enter the subcutaneous fat of the client (Greenway, 2004). “The ventrogluteal site has come to attract significant attention in the nursing literature and is seen by many as being the site of choice for IM injections” (Rodger & King, 2000, pg 577). However, even though it is said to be the best choice, only 12% of nurses used the site (Rodger & King, 2000). The lack of use is said to be because, ventrogluteal intramuscular injections is a fairly new practice, and practitioners are unfamiliar with the procedure of using this site, and have a lack of confidence when it comes to administering the injection. This is because they get the impression that this technique is a difficult and complex, but when they become more familiar with the anatomy of the site, then they will become more confident in land marking and administering medication (Greenway, Merriman & Statham, 2006). Greenway (2004) describes an easy technique for land marking the site, “to identify the ventrogluteal site, position the palm of your right hand on the left greater trochanter so your index finger points towards the anterior superior iliac spine. Now spread your middle finger to form a V. The injections site is in the middle of the V” (pg 40). Even thought land marking is not complicated, health care professionals do not want to change techniques when they feel confident (Greenway, Merriman & Statham, 2006) and familiar with the procedure of using the dorsogluteal (Greenway, 2004). However, even though they feel confident they still need to take in account that there are major blood vessels and nerves in the dorsogluteal area and complications can occur (Small, 2007). One of the most serious complications of intramuscular injections is injury to the sciatic nerve (Floyd & Meyer, 2007). Injury to this nerve due to intramuscular injections has been recognized since it was said to be the main site for injections and since they first began giving injections. However, over the years, because of the possible complications linked with using the dorsogluteal, its use is starting to become more and more discouraged (Small, 2004). Evidence shows that injury to the sciatic nerve is linked with the use of the dorsogluteal site for injections. Along with injuring the sciatic nerve, literature states that it can also cause a lot of “client discomfort, morbidity, and lasting disability” (Small, 2004, pg 288). There is a lot of agreement in different literature that states the ventrogluteal site is more favoured because it causes less pain and the nurse does not need to worry about hitting the sciatic nerve (Small, 2004). However, Floyd & Meyer (2007) stated that the dorsogluteal is the most commonly used for intramuscular injection, even if there are potential dangers. If an injection is done into the dorsogluteal, “the nurse must have a full appreciation of the anatomy of the site and proximate anatomic structures, be able to accurately identify anatomic landmarks and site boundaries, and administer the injection with meticulous technique” (Small, 2004). If the nurse does not use careful technique and does hit the sciatic nerve, it can produce a wide range of effects. The patient could experience minimal sensory and motor abnormalities (Small, 2004) to short or long-term paralysis (Greenway, Merriman & Statham, 2006), and unbearable pain that is unresponsive to any sort of analgesia (Small, 2004). Hitting the sciatic nerve is not the only problem linked with using the dorsogluteal site. When using this site there is also a major risk that when you administer the drug it will be injected into the subcutaneous fat later, instead of the muscle because the fat can layer can fluctuate from 1 cm to 9cm (Greenway, 2004). This results is a slow uptake of the medication, as well as the tissue becomes irritated because it was not administered into the muscle, making this site less preferred over the ventrogluteal (Greenway, 2004). Unlike the ventrogluteal having a wide variety of positions for the patient, whether it be sitting, standing or lying down, the dorsogluteal cannot be individualized for the patient because it is limited on what position it should be given. The health care worker should not give the injection in the dorsogluteal when the patient is standing. Roger and King (2000) state that the patient should be either lying on their side or in prone positions. This helps relax the surrounding muscles, as well as aids in reducing the amount of pain produced from/by the injection (Rodger & King, 2000). Literature states that very few people prefer to use the ventrogluteal site (Floyd & Meyer, 2007). However, an advantage of using the ventrogluteal is that it lacks main blood vessels or nerve structures. As well as there is a lot of muscle tissue which helps reduce the possibility of injury which all suggests that using the ventrogluteal it the best site for intramuscular injections (Floyd & Meyer, 2007). However, literature argues that because the ventrogluteal site is not regularly used that this may account for the lack of problems connected with the site (Floyd & Meyer, 2007). Floyd & Meyer, 2007 Small Roger and King 2000 Greenway, Merriman & Statham, 2006 Greenway 2004