Immunology Chapter 5 [4-20
advertisement

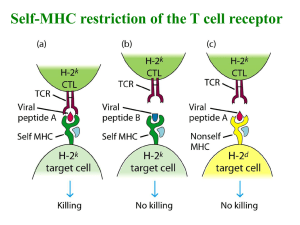
Immunology Chapter 5: Cell-Mediated Immune Responses Cell-mediated immunity uses T cells to fight intracellular microbes 2 ways a microbe can infect and hang out in infected cells: - - It resists phagocytes, and then uses the phagocyte to live in o Only part of a phagocyte that kills the pathogen is the vesicle, so if they escape the vesicle, they’re safe in the phagocyte Binding to, and then infecting, host cells Page 90 Naïve T cells constantly circulate through the lymph organs, searching for foreign protein antigens - Have antigen receptors to recognize the foreign stuff, but can’t do anything about it until the T cell is activated The job of naïve T cells is to recognize foreign antigens Antigen recognition actives the T cell, causing it to differentiate into effector cells - Microbe protein antigens are taken to the lymph organs by antigen presenting cells (APCs), and are expressed on the phagocyte MHC, to show to the T cells When a T cell recognizes an antigen, the T cell stops and activates o So T cells first encounter antigens in the peripheral lymph organs At the same time as the T cells are recognizing the antigen, the APC and other innate mechanisms provide signals to the T cell Once activated, the T cell releases cytokines - - The cytokines can trigger proliferation of antigen-specific T cells, which is called clonal expansion Some of the cells that proliferate will then differentiate into effector T cells, whose job is to get rid of the microbe Some of the effector T cells will work with B cells in the lymph organ to get rid of the microbe there, while other T cells will go into circulation to the site of infection to get rid of the microbe there Some of the cells that proliferate will instead differentiate into memory T cells, which are inactive on this exposure, but stick around ready to quickly respond to the next exposure Once the infection is eradicated, the stimuli for the T cells to proliferate ends, and T cell levels go back to normal T cell antigen recognition: - Types of T cell receptors: o TCR – recognizes MHC associated peptide antigens o CD4/CD8 coreceptors- recognize MHC molecules - - - - o Adhesion molecules- bind T cells to APCs o Receptors for costimulators from APCs o Accessory molecules- complementary molecules that work in signaling and adhesion Page 93 The TCR and the CD4/CD8 coreceptors all work together to recognize MHC complex with its peptide antigens o Binding to these receptors is the first signal that initiates T cell activation o MHC I’s display antigens from the cytoplasm o MHC II’s display antigens that were taken from the ECF into their vesicles o The TCR is made of an α chain and a β chain, and both work in antigen recognition o The TCR can recognize both the displayed antigen peptide, and parts of the MHC molecule o The CD4 and CD8 coreceptors help the TCR while it’s binding the peptide-MHC complex, by binding whatever MHC it is (1 or 2) at a different site CD4+ T cells (TH cells) recognize MHC 2 molecules CD8+ T cells (TC cells) recognize MHC 1 molecules o It takes binding of multiple TCRs and CD4/8 coreceptors to activate the T cell o Binding also must last for a little while to generate enough of a signal for a response from the T cell o Once all of this happens, the T cell begins its activation program In lymphocytes, some molecules are used for antigen recognition, and others are used for signaling o Ex: TCR can bind antigens, but can’t signal to the interior of the cell The signaling is done by a CD3, and a ῐ chain, which both connect to the TCR to form the TCR complex The TCR α and β chains do the recognizing, and the CD3 and ῐ chain do the signaling Adhesion molecules on T cells recognize their ligands on APCs, and stabilize binding of the T cell to the APC o Most TCRs bind the peptide-MHC complex with low affinity o So the adhesion molecules are what are used to keep the T cell bound long enough to the APC for activation o The major integrin used is LFA-1, which binds to ICAM-1 on the APC o In a naïve T cell, the LFA-1 is in a low affinity state Cytokines from innate immunity convert the T cell’s LFA-1’s to a high affinity state, and the LFA-1’s cluster together Antigen recognition also increases the affinity of the T cell’s LFA-1’s The full activation of T cells is dependent on the recognition of costimulators on the APC’s o This stimuli works with the stimulation from the antigen o 2 costimulators of APCs used for T cells are B7-1 (CD80) and B7-2 (CD86) Expression of these is greatly increased when the APC sees a microbe The receptor on T cells for B7-1 and -2 is CD28 - - - Without CD28-B7 binding, binding of the TCR alone can’t active the T cell Things that block this binding are used to treat rheumatoid arthritis o Costimulation guarantees that only a microbe, and not a harmless foreign substance, will activate the T cell o CD40 on the APC is another costimulator that binds the CD40 ligand on the T cell For this one, T cells express the CD40 ligand to bind the APC CD40, in order to make the APC express more B7 costimulator, and secrete cytokines like Il-12, which enhances T cell differentiation Substances that activate the APCs are necessary for a vaccine to work, they’re called adjuvants o Adjuvants work by causing expression of costimulators on APCs, and stimulating APCs to secrete cytokines like Il-12 that activate T cells o Adjuvants are usually products of dead microbes, that will mimic the microbe Other receptors in the CD28 family can inhibit T cells o CTLA-4 – recognizes B7 on APCs o PD-1 – recognizes ligands of many cells o Both are induced in T cell activation, and lack of these may cause autoimmunity The activation of CD8+ T cells is stimulated by MHC I’s, costimulators, and TH cells o CD8+ T cells have a few differences in their responses One difference is that the cytoplasmic antigen of the virus-infected cell has to be cross presented by dendritic cells Another difference is that CD8+ T cell differentiation into TC cells may need TH cells The same APC will also present MHC 2 for activating the TH cells The TH cell can release cytokines to activate CD8+ cells o HIV targets TH cells, preventing activation of TC cells Activation of T cells - Once recognition has finished, T cells express proteins involved in the proliferation, differentiation, and effector function of the cell Gene transcription and protein synthesis increase quickly after recognition TCR’s and co-receptors cluster and cross-link when they bind MHC-antigen complexes After binding, the TCR, CD4/8 co-receptors, and CD28 cluster at the center of the T cell membrane, and the integrins form a ring around the cluster o Creates an optimal arrangement for inducing activating signals in the T cell o The T cell – APC cell connection is called an immunologic synapse o The clustering of CD4 and CD8 activate a tyrosine kinase called Lck at their tails Lck then phosphorylates tyrosine ITAMs on the CD3 and ῐ chain of the TCR Once phosphorylated, ITAMS bind another tyrosine kinase called ZAP-70 ZAP-70 then also gets phosphorylated by Lck, activating the ZAP-70, which then goes and phosphorylates other proteins and enzymes in several pathways Calcium-NFAT pathway o o o o o Ras-MAP kinase pathway PKC-NF-kB pathway PI-3 pathway Calcium-NFAT pathway Initiated when ZAP-70 phosphorylates and activates phospholipase Cγ (PLCγ) PLCγ the converts phosphatidylinositol-4,5-bisphosphate into IP3 and DAG Inositol 1,4,5-triphosphate (IP3) stimulates release of calcium from the ER, raising the cytoplasmic calcium concentration This triggers calcium channels to open and calcium influx occurs The calcium binds calmodulin, and the two activate a phosphatase called calcineurin Calcineurin removes phosphates from the transcription factor NFAT in the cytoplasm Once dephosphorylated, NFAT goes to the nucleus to promote genes for the T cell growth factor called Il-2 Cyclosporine is an immunosuppressant that works by binding and inhibiting calcineurin Ras/Rac-MAP kinase pathway ZAP-70 and clustering both recruit Ras and Rac, and activates them by trading bound GDP for GTP Ras or Rac bound GTP activate MAP kinases The MAP kinases in this pathway are ERK and JNK ERK and JNK promote proteins c-Fos and c-Jun, which combine to form activating protein 1 (AP-1), which enhances transcription of T cell genes PKCθ-NF-kB pathway PLCγ makes diacylglycerol (DAG), which activates the θ isoform of protein kinase C (PKC) Protein kinase C then activates NF-kB NF-kB is initially bound by inhibitor IkB in the cytoplasm of the T cell TCR signals lead to activating of a kinase to target IkB for destruction, releasing NF-kB to go to the nucleus and promote transcription of genes Phosphatidylinositol-3 (PI-3) pathway PI-3 phosphorylates phosphatidylinositol-4,5-bisphosphate (PIP2) into PIP3 PIP3 activates the serine-threonine kinase Akt, which prevents apoptosis and keeps the T cell alive This pathway is triggered by TCR, as well as CD28 and Il-2 All of these pathways lead to transcription factors that cause the making of cytokines, cytokine receptors, and effector molecules Response of T cells to antigens - - Recognition and signaling lead to a response by T cells involving proliferation and differentiation into effectors Cytokines are proteins that function as mediators of immunity and inflammation o In adaptive immunity, cytokines are released by T cells o Interleukin means a protein that’s made by leukocytes, and acts on leukocytes o The first cytokine made by a CD4+ T cell within 1-2 hours of activation, is Il-2 Activation also increases the ability of the T cell to respond to Il-2 Normally, the T cell only has 2 of the 3 chains of its receptor for Il-2 Once activated, the T cell makes the 3rd chain in order to bind Il-2 Il-2 stimulates survival and proliferation of T cells, so it’s aka T cell growth factor Il-2 stimulates T cells to enter the cell cycle and divide, increasing the number of antigen specific T cells o Page 102 Within 1-2 days of activation, T cells start to proliferate Proliferation allows the immune response to keep up with the proliferation of the microbe The progeny of the proliferating T cells then differentiate into effector cells and memory cells o Effector cells appear within 3-4 days after exposure The effectors then leave the lymph organ and go to the site of infection to kill the microbe + o CD4 TH cells can differentiate into effector cells that respond to the antigen by making surface molecules and cytokines that will activate phagocytes and B cells The most important surface protein in a CD4+ effector function is CD40 ligand, which binds to the CD40 of phagocytes and B cells, activating them CD40 binding causes the expression of costimulators on the APCs, and also causes them to make T cell activating cytokines, causing positive feedback for T cell activation + CD4 TH cells can also differentiate into effector cells that make cytokines 3 types: type 1 TH (TH1), type 2 TH (TH2), and TH17 Page 106 TH1 cells stimulate phagocytes to eat and kill microbes o TH1 cells make interferon-γ (IFN-γ), which activates macrophage to kill microbes, called classical pathway of macrophage ‘s activation o IFN-γ also stimulates making of antibodies that promote phagocytosis of microbes by binding to both the phagocyte and complement o IFN-γ can also stimulate expression of MHC-2’s, and B-7’s TH2 cells recruit eosinophils to come get parasites o TH2 cells make Il-4, 5, and 13 Il-4 stimulates making of IgE antibodies o o IgE activates mast cells, and binds to eosinophils Il-5 activates eosinophils Il-4 and Il-13 stimulate expulsion of parasites from mucosal organs, and inhibit microbe entry by stimulating mucus secretion Called “barrier” immunity These cytokines also stimulate macrophage to repair, called the alternative pathway of macrophage activation These cytokines can also inhibit the TH1 cytokines TH17 cells make Il-17 and Il-22 to mediate inflammation Differentiation into the specific kinds of TH depends on the stimuli the cell receives when it meets microbial antigens o When T cells are exposed to Il-12 from phagocytes, and IFN-γ from NK cells, it differentiates into a TH1 cell Example of innate immunity influencing adaptive o Il-4 tells T cells to form TH2 cells, but we don’t know where the Il-4 comes from o Inflammatory cytokines from phagocytes like Il-1, 6, 23, and TGF-β, tell T cells to form TH17 cells + CD8 T cells activated by antigens and costimulators differentiate into TC cells that kill infected cells Make stuff that drill holes in the cell, and then make other stuff that go in and cause apoptosis Other T cells differentiate into memory T cells Need signals from cytokines like Il-17 to stay alive When the infection is gone, all these signals that were keeping the extra T cells alive are gone, so the T cells die by apoptosis