Micro Chapter 63 [4-20
advertisement

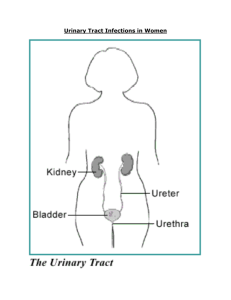
Micro Chapter 63: Urinary Tract Infections UTIs are the most common bacterial infection in humans Can happen in both men and women 1/5 girls will have a UTI by age 30, and over half will have a UTI in their life UTIs can happen at any part of the urinary tract – including the bladder, kidneys, and prostate in men Urethritis – infection of the urethra, and is characteristic fo some STDs, like gonorrhea and chlamydia Acute uncomplicated UTI – a UTI that presents as acute cystitis (bladder or lower-tract infection) in otherwise healthy women Acute nonobstructive pyelonephritis (aka acute uncomplicated pyelonephritis) – kidney infection or upper tract infection in otherwise healthy women Complicated UTI – UTI in people with underlying structural or functional abnormalities of the GU Asymptomatic bacteriuria – bacteria in the urine, but no signs or symptoms of UTI Bacterial prostatis – bacterial infection of the prostate Chronic bacterial prostatis – chronic bacteria in the prostate causing recurrent or persistent pelvic or urinary symptoms in men A person who’s had a UTI is at risk for a future one Reinfection – if a new organism is isolated, or a previously isolated organism is reintroduced - Reinfection in UTIs happens when a previously isolated organism is reintroduced into the urinary tract from the colonizing gut or genital flora Relapse – UTI that resists drugs and stays in the GU tract UTI usually happens when colonizing flora from the periurethral area, or vagina in women, ascend up the urethra into the bladder - Bacteria causing UTI usually originate from the normal gut flora UTI happens more often in women, because of the shorter female urethra, allowing easier access of bacteria to the bladder Most bacteria that ascend to the bladder, will be removed with the next normal urination For infection ot happen, bacteria must be able to persist and reproduce int eh bladder Pyelonephritis happens when organisms go further up to the kidneys o Can happen when the bacteria have adhesins, or from reflux up the ureter in people with incompetent ureteral sphincters - - Bacterial infection of the prostate gland also happens mainly through ascension of organisms form the urethra into the prostate ducts o This is facilitated by turbulent urine flow, which is common in men with prostate hypertrophy Occasionally, UTI can happen from spread of organism through the blood from somewhere else o The characteristic feature of hematogenous dissemination (spread through blood) is renal abscesses in the renal cortex o UTIs from blood are usually S. aurea or candida The most important pathogen in UTI is E. coli, but other bacteria can cause UTI Uncomplicated UTI: - - Uncomplicated UTI will be E. coli 80-85% of the time o An essential E. coli virulence characteristic for acute cystitis is expression of mannosesensitive fimbria (FimH) This protein receptor allows adherence of E. coli to bladder uroepithelial cells, through attachmet to the mannosylated glycoproteins that line the bladder mucosa The adhesion is common though, so other things must also lead to the bladder infection Staph saprophyticus is a gram-positive that is seen in the rest of uncomplicated UTI cases o S. saprophyticus is seen way more often in the fall When it becomes acute nonoubstructive pyelonephritis, it is usually E. coli o Has the adhesion factor P fimbria, which binds Gal disaccharide Causes bacterial persistence and inflammation of the urinary tract o Other virulence factors include aerobactin (scavenges for iron for the bacteria to grow) and hemolysin (may lyse host cells) Complicated UTI: - - E. coli is again the most common pathogen for complicated UTI, but the % isn’t as high as for uncomplicated Urease producing organisms, like proteus mirabilis, morganella morganii, and providencia spp. are common causes as well o These organisms are also pathogenic because as urease metabolizes urea to ammonia, it can lead to struvite formation o The ammonia produced damages the kidney directly, and can cause kidney stones that obstruct and cause further damage Bacteria from people with complicated UTI are also characterized by being resistant o This is because of using antibiotics on them in the last time they flared up People with complicated UTI often have urologic devices in them, like a urethral catheter o o They get coated with biofilm when bacteria contaminate them and grow along them, then ascend to the bladder The conditions caused by the device protect the organisms growing from antibiotics and host defense, making them hard to get rid of Asymptomatic UTI – E. coli is again most common, with low prevalence of virulence factors Acute bacterial prostatitis is an uncommon infection, mainly caused by S. aureus or E. coli Prostate stones form in men with age, providing a way for organisms to persist in the prostate, and a source of bacteria for relapsing cystitis The most important host defense for preventing UTI is complete, normal urination - This removes bacteria in the bladder and along the uroepithelial cells Host factors in uncomplicated UTI: - - - - Shows normal voiding Women with recurrent acute uncomplicated UTI are more likely to have a close relative who also gets recurrent infections o Shows a genetic predisposition o One genetic cause is if you don’t secrete ABH blood antigens They’re normally secreted at mucosal surfaces, and bind to receptors on bacterial cells to prevent attachment to the uroepithelium About 1/5 of people are nonsecretors, so their bacterial cell surface receptors remain exposed, allowing attachment of bacteria to host uroeptihelial cells The most important behavioral risks for acute cystitis in premenopausal women are sexual intercourse and use of spermicides for birth control o Sex mechanically facilitates the ascension of organisms from the periurethral area into the bladder o Bacteria enter the bladder in about 1/3 of episodes of intercourse They get cleared usually the next time the girl urinates, but if they don’t you get either symptomatic or asymptomatic infection o An increased frequency of intercourse is associated with an increased frequency of symptomatic UTIs o The normal flora of the vagina maintains an acidic pH that prevents colonization by potential pathogens like E. coli Spermicide disrupts this normal flora, allowing E. coli to colonize the vagina Other behavioral risk factors that are less important are a new sex partner, diaphragm use, and recent use of antibiotics o New sex partner increases exposure to new strains of E. coli o A diaphragm may block the urethra and prevent complete bladder emptying Condom use without spermicide, or use of birth control pills, won’t increase risk of infection - Things that don’t increase risk for UTI are urination before or after sex, wiping, douches and tampons, types of underwear, or bathing rather than showering Uncomplicated UTI is rare in healthy young men – so rare though that you basically assume a UTI in a guy is comlicated o Risk factors for men include a new sex partner, and anal sex Patients with complicated UTI have structural or functional problems of the GU tract that compromise urination, or promote entry of bacteria into the urinary tract - Includes blocked urine flow, stones, and increased access thanks to catheters or reflux Women with acute cystitis have an inflammatory response in the urinary tract, characterized by local cytokine production (like Il-6, 8, or 10) and recruitment of WBCs - Probably triggered by LPS activating TLR-4 on the bladder epithelium Untreated acute uncomplicated cystitis resolves in about half of episodes by 2-4 weeks The limited local immunity that develops in an episode of acute cystitis, doesn’t protect from future episodes For acute pyelonephritis, the initial host response is also inflammatory - - Manifested by pyuria (WBCs in the urine) and cytokine production Systemic inflammotry response includes fever, WBCs, and increased C-reactive protein o System antibodies develop, mainly IgM for the first infection, and IgG’s in following infections The inflammatory response int e kidney likely adds to tissue damage and renal scarring Diagnosing UTIs: - - Uncomplicated cystitis or pyelonephritis o Acute cystitis in women presents with lower tract irritative symptoms like dysuria (pain urinating), frequency (having to go a lot), urgency (need to urinate immediately once you feel the urge) and suprapubic discomfort Some women also get hematuria if you see vaginal symptoms like discharge or irritation, consider vaginitis or an STD o Women with acute uncomplicated pyelonephritis present with costovertebral angle pain and tenderness due to renal inflammation Usually unilateral, but can be bilateral The systemic inflammatory response accompanying pyelonephritis shows fever, and possibly nausea, vomiting, and sepsis hemodynamic problems Pyelonephritis can also show lower-tract irritative symtpoms Complicated UTI - Show symptoms of uncomplicated or pyelonephritis - - - Acute prostatitis presents with severe local and systemic symptoms, including high fever, pelvic pain, and urinary retention o Prostate will be swollen and tender o Don’t do a rectal exam cause it may make things worse Urine culture o Need bacteria from urine to diagnose a UTI o Have men pee in a cup, and women too but they have an increased chance of contaminating it with vaginal secretions and giving false positive If a woman can’t cooperate with urinating, you can get a urine sample with a catheter o Contaminants show low #’s of colonies, while infecting organisms will have high concentrations o Most people with UTI just have one organism in the urine, but complicated UTI can show more than one, especially when there’s a device like a catheter in place o If you took a sample in a way that included biofilm, the biofilm is measured too and usually has more organisms o Any pathogens found in the urine is diagnostic for UTI For acute pyelonephritis or complicated UTI, they’ll have equal to or more than 105 bacteria Pyuria is measured by microscopic examination of the urine, or a dipstick leukocyte esterase test o Usually you’ll see pyuria in UTI, but you usually see WBCs in the urine any time bacteria is in he urine, so pyuria isn’t diagnostic for UTI o Lack of pyruia though is a good indictor there is no UTI Treating UTI’s – page 647 table for treating UTIs - - Antibiotics that get excreted in the urine should be used for therapy For cystitis, all you need to give them is an antibiotic into the urine For pyelonephritis, you need antibiotics to get into both the tissues and urine Short 3 day therapy is done in acute cystitis, and there’s no need for culture tests cause they’ll take 3 days to get back anyways Trimethoprim/sulfamethoxazole, or just trimethoprim, are the first choice drugs for 3-day therapy o Second line choices include fluoroquiniolone for 3 days or nitrofuantioin for 5 days o These 3 drugs are empiric therapy Acute uncomplicated pyelonephritis o A urine specimen for culture should be taken before starting antibiotics o The infection can be serious, so you have to know what the infecting organism is, to pick the right therapy o Should also take a WBC count, serum creatiine, and blood and urine cultures o How severe it is depends on if there is fever, and the hemodynamic status o - - - You start with empiric therapy, and then reassess once urine culture results come back in 2-3 days Can use, trimethoprim/sulfamethoxazole, just trimethoprim fluoroquinolones, depending on what you think the culture will tell you o Usually 7-14 days of therapy is recommended o If there is no improvement in 2-3 days, check for urinary obstruction, abscess, or other issues Complicated UTI o Need a urine sample before you start antibiotics every time Due to many different possible infecting organisms, and a good chance of resistance being present o If symptoms are mild, delay therapy till the results come back o If symptoms are severe, empiric therapy is used, and then reassessed once the tests come back Asymptomatic bacteiuria – common in many populations, including nursing homes o Should not be screened or treated in most cases Does more harm than good Exception – always screen and treat a pregnant patient Earlier you catch it, the less the chance of pyelonephritis later int eh pregnancy Recurrent UTI- 2 per 6 months, or 3 per year o Prolonged antibiotic therapy may be indicated, to prevent reinfection o Recurrent acute uncomplicated UTIs – antibiotics are very effective Given as long-term low-dose therapy daily or every other day Prophylaxis is indicated after 2 infections Trimethoprim/sulfamethoxazole, just trimethoprim, and fluoroquinolones work, and decrease gram-negative colonizing flora in the gut, vagina,a nd periurethral area, preventing infection Probiotics, like in yogurt, don’t prevent recurrent infections Daily cranberry juice or tablets decrease the frequency of infection by 1/3 The cranberry juice binds E. coli adhesins as it’s excreted o Recurrent complicated UTI – fix the underlying problem that is promoting infections