My Skin Disorder Outline

Ch 45 Skin Disorders
Inflammatory Disorders o Eczema
Most common skin condition. When you hear eczema think dermatitis. Includes seborrheic and atopic o Allergic Contact Dermatitis o Irritant Contact Dermatitis o Atopic Dermatitis o Stasis Dermatitis o Seborrheic Dermatisis
Allergic and Hypersensitivity Dermatoses o Type I (Allergies) sometimes called anaphylactic response
Atopic Eczema
Urticaria (hives)
Characterized by vasodilation, increased capillary permeability, smooth muscle contraction, etc.
Type II is a cytotoxic reaction
Type III is immune complex reaction
Type IV is a delayed or cellular reaction
Urticaria o Lesions are raised areas of cutaneoud edema
Drugs, foods, systemic diseases
Histamine, vascular constriction, and edema
Hives, wheals, welts
Mild allergic response
Cutaneous Vasculitis o Immune complexes deposited in small vessels after exposure to an antigen
Drugs, allergens, bacteria, viruses
Complement, chemotactic for WBC’s
Type III response, inflammation of the small blood vessels in the skin after exposure to an antigen
Purple discoloration, ischemia and something else result from something
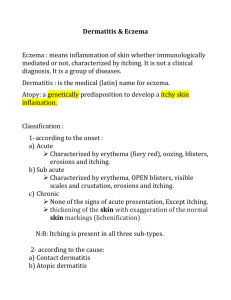
Eczema o Most common inflammatory disorder
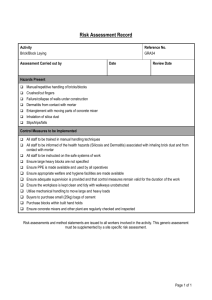
An inflammatory response of the skin caused by internal or external sources.
Kind of a general term for dermatitis. o Erythema, versicles, scales, and pruritis (itching)
Characterized by these things
Can also see edema, swelling, serous discharge, and when the drainage ruptures and dries, crusting.
Chronic E makes leathery skin. It’s think and hyperpigmented (darker than all your other skin). Location is important when you are talking about the cause of dermatitis. IF you have a new laundry detergent and you have an allergic response to it, where you’re clothes are tight are where you would see that reaction! It’s where it’s touching you the most!
Atopic Dermatitis o Affects approimately 10% of population o More common in infants, children o Associated with Inflammation,Allergies, Immune response. Sometimes hay fever or food allergies. Also an increased sensitivity to histamine.
Mast cell activation
Histamine, lymphokines
T lymphocytes, Langerhans cells (immune cells of the skin),
Monocytes, IgE production
Chronic inflammation
Incidence has increased over the last 30 years or so. Some people outgrow it, sometimes it hangs around for life.
Common on the hands, feet, and flexor surfaces (the spots that bend, like the back of your knees and inside of your elbows)
Lichenification= term for leathery, hyperpigmenation of the skin
Treatment is low dose steroids or anti-histamines.
Effected individuals should avoid herpes simplex exposure and vaccination with live virus (the effect could be hypersomething or other, super bad response)
Allergic Contact Dermatitis o Erythema & edema, pruritis, vesicles (the same as atopic) o Allergy to Metal, chemicals, poison ivy o Cell mediated immune response o Delayed hypersensitivity response o Urticaria (wheals) can be present
Irritant Contact Dermatitis o Prolonged exposure to acids or bases
Wal-Mart sandles? Damn, her feet were messed up… o Nonimmunologically mediated inflammation o Lesions similar to Allergic Contact o Erythema & edema, pruritus, vesicles (same as allergic contact)
Stasis Dermatitis o Venous Insufficiency venous stasis ulcers, incompetent valves cause it o Venous stasis and edema
o Erythema, pruritis, scaling, petechiae, hyperpigmentation, Brawny (woody) edema (skin is tough and thick like green wood) o Ulcerated lesions may form - irregular borders, “weepy faucet”, champagne bottle appearance o Treatment: elevation, not standing for long periods, wearing lose clothing. Sometimes antibiotics are used when they get a secondary infection from their skin being all messed up.
Cutaneous Infections o Bacterial o Viral o Fungal (tinneas vs. candidiasis/yeast) o Pretty common, generally localized and superficial. Occasionally sepsis can occur, which can be life threatening. We have all kinds of natural flora on our skin but kicks our ass when it gets in our body.
Bacterial Infections o Folliculitis furuncle carbuncle o Cellulitis
Skin and sometimes SubQ tissue as well o Difference is degree of tissue involved o Impetigo
May lead to poststreptococcal hypersensitivity reactions
These can cause glomerulonephritis o Boils are most commonly caused by Staph aureus.
Acne o Disorder of sebaceous glands o Related to:
Hormonal stimulation of sebaceous glands
Increased number of sebaceous cells
Increased sebum production
Inflammatory response to bacteria in sebum
Viral o Herpes Simplex
Cold Sores o Herpes Zoster
Varicella (shingles)
Herpes invades dorsal root ganglia
Caused when chickenpox herpes virus is reactivated
Travels out nerve to skin and causes a new inflammation o Papillomavirus
Warts
Condyloma
Venereal Warts
Increased risk of Cervical cancer o Verrucae (warts)
Benign Neoplasms (papillomas)
Skin Infections of the fungal variety o Superficial fungal infections
Ringworm, athlete’s foot
Attack the keratinized (dead) cells
Inflammatory reaction to toxins causes most signs and symptoms o Deep fungal infections
Candidiasis, sporotrichosis
Attack living tissue
May attack other organs
Fungi o Tineas o Candidiasis o Onychomycosis
Vesiculobullous Disorders o Pemphigus Vulgaris
Autoimmune
IgG autoantibodies
React with intracellular cement leading to loss of adhesion between epidermal and dermal cells
Directed against the cell surface adhesion molecule desmoglein at the cell junction in suprabasal layer in epidermis.
IgG and complement bind to desmoglein adhesion molecules (causing) destruction of cell to cell adhesion o Acantholysis o Blister formation
2 drugs are associated with it: PCN and Captapril administration o Bullous Pemphigoid
Milder form
More often seen in people over the age of 60 o Erythmea Multiforme
Acute inflammation with target-like lesions
Rings of edema and inflammation
Allergic reaction to drugs, herpes simplex
Stevens-Johnson syndrome - mucus membrane involvement
Drug-Induced Skin Eruptions o Erythema multiforme
Occurs after herpes simplex; self-limiting
o Stevens-Johnson syndrome
Skin detaches from body surface; <10% of body affected o Toxic epidermal necrolysis
>30% of epidermis detaches
30%–35% mortality rate
Immune mediated
Papulosquamous Dermatoses o Psoriasis
You get papules, scales, plaques, and erythema. There are well demarcated, thick, silvery, scale, erythematous plaque on normal skin
Patho:
Chronic, noninfectious, T cell mediated inflammatory condition
T cell cytokine release (TNF-a), inflammatory response hyperproliferation of keratinocytes thick inflamed plaques
Red raised plaques c silvery scales o Pityriasis rosea- self limiting inflammatory disorder. Occurs in young adults in the winter. Probably herpes in origin. Begins with a single lesion (The Herald Patch) which is
3-4 cm, salmon pink, and clearly demarkated (you can tell where it is) o Lichen planus- benign auto immune inflammatory disorder of the skin and mucous membranes. It can occur after exposure to drugs or film processing chemicals. Causes non-scaling, violet colored puritic 2-4 mm papules on the wrist, ankles, lower legs, and genitalia. Patho might be the epithelial cells are considered foreign by the T cells, so the
T cells try and eat them.
Pressure Ulcers o Risk Factors
Immobilization
Failure to move or turn
Debilitation
Incontinence
Friction or Shear
Use the Braden Scale to assess the risk factors, duh.
Risks associated with certain chronic conditions
Neurologic disorders
Anemia
Edema
Renal Failure
Malnutrition
Sepsis o Patho
Immobility
Continuous Pressure
Capillaries occlude with platelets
Microthrombi form
Occlusion of blood flow
Anoxic necrosis
Sun Exposure o Sun exposure increases the risk of skin cancer o Cumulative sun exposure increases risk of:
Basal cell carcinoma
Squamous cell carcinoma o Severe sun exposure with blistering increases risk of:
Malignant melanoma
Cancers arising from melanocytes
Asymmetry
Border irregularity
Color variegation
Diameter > 0.6 cm
Evolving change over time
Types of Melanomas o 70% are superficial spreading
Raised edges; grow horizontally and vertically
Ulcerate and bleed o 15%–30% are nodular
Dome-shaped, blue-black o 4%–10% are lentigo maligna
Slow growing, flat o 2%–4% acral lentiginous
On palms, soles, nail beds, mucous membranes
Skin Disorders of the Elderly o Actinic (solar) damage
Keratoses: premalignant lesions
Lentigines: liver spots o Vascular lesions
Angiomas
Telangiectases
Venous lakes
Benign Tumors o Suborheic Keratosis o Keratocanthoma o Actinic keratosis o Nevi
Malignancies of the Skin
o Basal cell - most common, recurs often
Originate from cells around hair follicles or glands o Squamous cells can become invasive
Actinic (solar) keratosis is premalignant lesion o Melanoma can metastasize via lymph
Arise from basalar epidermal cells or Nevi o Kaposi sarcoma - vascular malignancy
Seen in immunodeficiency
Herpes simplex-8
Damage due to ? DNA sythesis, repair, replication; protooncogene activiation or inactivation of tumor suppression
Sunburn Patho o Ultraviolet radiation hits the melanocytes. The melanin becomes oxidized which causes a tan. More melanin is produces which creates a delayed tanning effect. o Some of the UV reaches lower skin layers which damages your DNA and your immune cells. Inflammatory mediators are released. This causes the sunburn!
Burns o 1 st Degree
Partial thickness
Outer layers of the epidermis o 2 nd Degree
Superficial partial thickness, blistering, pain
Deep partial thickness, dermis, no appendages
Epidermis and Dermis
Partial thickness is only part of the dermis
Full thickness is the entire dermis o 3 rd Degree
Full-thickness, entire epidermis, dermis, hypodermis, painless (because you burned away all your pain receptors)
Extends into the subq tissue
May damage muscle, bone, and blood vessels