BMW23: PDGFRA rearrangement leading to hyper
advertisement
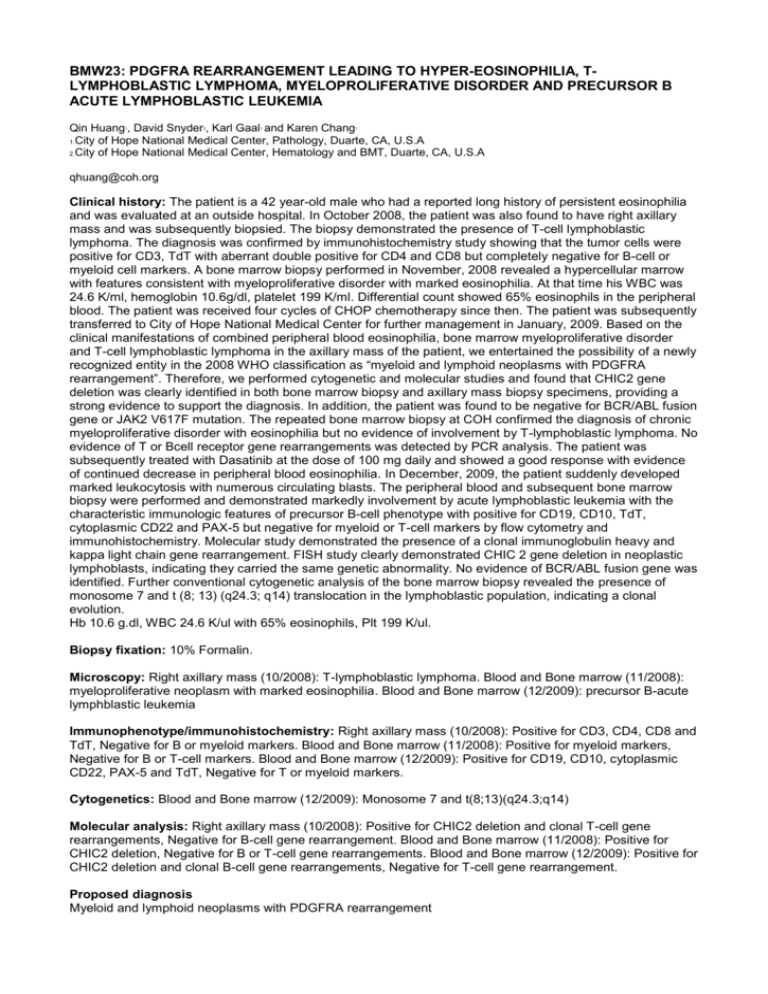
BMW23: PDGFRA REARRANGEMENT LEADING TO HYPER-EOSINOPHILIA, TLYMPHOBLASTIC LYMPHOMA, MYELOPROLIFERATIVE DISORDER AND PRECURSOR B ACUTE LYMPHOBLASTIC LEUKEMIA Qin Huang , David Snyder , Karl Gaal and Karen Chang 1.City of Hope National Medical Center, Pathology, Duarte, CA, U.S.A 2.City of Hope National Medical Center, Hematology and BMT, Duarte, CA, U.S.A 1 2 1 1 qhuang@coh.org Clinical history: The patient is a 42 year-old male who had a reported long history of persistent eosinophilia and was evaluated at an outside hospital. In October 2008, the patient was also found to have right axillary mass and was subsequently biopsied. The biopsy demonstrated the presence of T-cell lymphoblastic lymphoma. The diagnosis was confirmed by immunohistochemistry study showing that the tumor cells were positive for CD3, TdT with aberrant double positive for CD4 and CD8 but completely negative for B-cell or myeloid cell markers. A bone marrow biopsy performed in November, 2008 revealed a hypercellular marrow with features consistent with myeloproliferative disorder with marked eosinophilia. At that time his WBC was 24.6 K/ml, hemoglobin 10.6g/dl, platelet 199 K/ml. Differential count showed 65% eosinophils in the peripheral blood. The patient was received four cycles of CHOP chemotherapy since then. The patient was subsequently transferred to City of Hope National Medical Center for further management in January, 2009. Based on the clinical manifestations of combined peripheral blood eosinophilia, bone marrow myeloproliferative disorder and T-cell lymphoblastic lymphoma in the axillary mass of the patient, we entertained the possibility of a newly recognized entity in the 2008 WHO classification as “myeloid and lymphoid neoplasms with PDGFRA rearrangement”. Therefore, we performed cytogenetic and molecular studies and found that CHIC2 gene deletion was clearly identified in both bone marrow biopsy and axillary mass biopsy specimens, providing a strong evidence to support the diagnosis. In addition, the patient was found to be negative for BCR/ABL fusion gene or JAK2 V617F mutation. The repeated bone marrow biopsy at COH confirmed the diagnosis of chronic myeloproliferative disorder with eosinophilia but no evidence of involvement by T-lymphoblastic lymphoma. No evidence of T or Bcell receptor gene rearrangements was detected by PCR analysis. The patient was subsequently treated with Dasatinib at the dose of 100 mg daily and showed a good response with evidence of continued decrease in peripheral blood eosinophilia. In December, 2009, the patient suddenly developed marked leukocytosis with numerous circulating blasts. The peripheral blood and subsequent bone marrow biopsy were performed and demonstrated markedly involvement by acute lymphoblastic leukemia with the characteristic immunologic features of precursor B-cell phenotype with positive for CD19, CD10, TdT, cytoplasmic CD22 and PAX-5 but negative for myeloid or T-cell markers by flow cytometry and immunohistochemistry. Molecular study demonstrated the presence of a clonal immunoglobulin heavy and kappa light chain gene rearrangement. FISH study clearly demonstrated CHIC 2 gene deletion in neoplastic lymphoblasts, indicating they carried the same genetic abnormality. No evidence of BCR/ABL fusion gene was identified. Further conventional cytogenetic analysis of the bone marrow biopsy revealed the presence of monosome 7 and t (8; 13) (q24.3; q14) translocation in the lymphoblastic population, indicating a clonal evolution. Hb 10.6 g.dl, WBC 24.6 K/ul with 65% eosinophils, Plt 199 K/ul. Biopsy fixation: 10% Formalin. Microscopy: Right axillary mass (10/2008): T-lymphoblastic lymphoma. Blood and Bone marrow (11/2008): myeloproliferative neoplasm with marked eosinophilia. Blood and Bone marrow (12/2009): precursor B-acute lymphblastic leukemia Immunophenotype/immunohistochemistry: Right axillary mass (10/2008): Positive for CD3, CD4, CD8 and TdT, Negative for B or myeloid markers. Blood and Bone marrow (11/2008): Positive for myeloid markers, Negative for B or T-cell markers. Blood and Bone marrow (12/2009): Positive for CD19, CD10, cytoplasmic CD22, PAX-5 and TdT, Negative for T or myeloid markers. Cytogenetics: Blood and Bone marrow (12/2009): Monosome 7 and t(8;13)(q24.3;q14) Molecular analysis: Right axillary mass (10/2008): Positive for CHIC2 deletion and clonal T-cell gene rearrangements, Negative for B-cell gene rearrangement. Blood and Bone marrow (11/2008): Positive for CHIC2 deletion, Negative for B or T-cell gene rearrangements. Blood and Bone marrow (12/2009): Positive for CHIC2 deletion and clonal B-cell gene rearrangements, Negative for T-cell gene rearrangement. Proposed diagnosis Myeloid and lymphoid neoplasms with PDGFRA rearrangement Interesting feature(s) of the submitted case This is a very unique and extremely interesting case. A single genetic abnormality (PDGFRA rearrangement) leads to multiple distinctive diseases involving all three major hematopoietic lineages etc. myeloid, T-cell and B-cells, truly representing a “hematopoietic stem cell disorder” and clearly proving the concept of hematopoietic plasticity and lineage infidelity of the neoplasm. To best of our knowledge, PDGFRA rearrangement cases with evolution to precursor B-cell acute lymphoblastic leukemia have not been recognized by the new 2008 WHO classification and have not been described in the literature.