C3 Semi-Solids 2015 - 1
advertisement
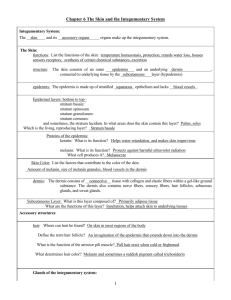
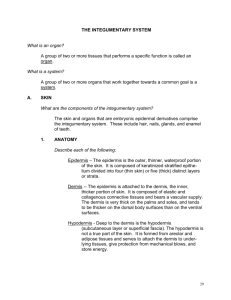
Pharmaceutics 2 - 2015 Semi-Solids Michael Wisch mike@mobile.geenet.co.za ceutics.geenet.co.za PHARMACEUTICS 2 SEMI-SOLID DRUG DELIVERY SYSTEMS - COURSE OUTLINE 1. Introduction 2. Structure of human skin 3. Functions of the skin Containment Barrier functions Reception of external stimuli Regulation of body temperature Synthesis and metabolism Disposal of biochemical wastes Intraspecies identification and/or sexual attraction Blood pressure regulation 4. Rationale for topicals Targets for topical drugs (surface and stratum-corneum effects) 5. Percutaneous absorption Variability in the permeability of healthy and damaged skin Process of percutaneous absorption 6. Classification of semi-solids Hydrocarbon bases Water-soluble bases Gels Emulsion-type semi-solids (emulsified and non-emulsified bases) 7. Emulsions and creams Classification of emulgents Preservatives and antioxidants Multiple emulsions 8. Ointments ; pastes ; gels 9. Methods of preparation of semi-solids 10. Evaluation criteria for topical drug delivery systems Stability of active ingredients and adjuvants Cosmetic criteria (appearance, odour, ease and feel of application) Rheological characteristics (viscosity, extrudability) Phase Distribution (homogeneity, phase separation, bleeding) Particle size distribution of dispersed phases Loss of water and other volatile vehicle preparations Particulate contamination Microbial contamination/sterility (unopened container/under conditions of use) Bioavailability (release, factors affecting percutaneous penetration) STRUCTURE OF THE HUMAN SKIN The skin may be divided into 2 main tissue groups: a) epidermis (avascular, generally nonliving) b) dermis (connective tissue, blood vessels and glands) The anatomically distinguishable regions from the outside of the skin inward: (I) stratum corneum (nonviable epidermis) 10 µm thick (2) viable epidermis 100 µm thick and includes the basal layer (3) dermis 1000 µm thick The skin appendages (hair follicles and associated sebaceous glands, eccrine sweat glands) project through the epidermis down to the dermis. Also penetrating the tissue but not into the epidermis is a complex network of blood vessels. Finally, the skin is interlaced with sensory nerves. Stratum corneum Also called the "cornified or horny" layer of the skin. Formed from approximately 10-15 layers of dead, fully-keratinized, flattened cells. The cells overlap to form a continuous sheet without pores and is a thin, ultra dense epidermal covering. SC is of different thicknesses depending on body site - e.g. much thicker on friction surfaces such as the hands and soles of the feet. SC is under continuous formation, as cells are worn off the surface, they are replaced. A total turnover of cells in this stratum occurs about every 2 weeks in adults. Cells originate through mitosis in the basal layer of the epidermis (germinal/proliferative). As they migrate to the surface, the cells flatten and inwardly synthesize protein and lipid which determine the nature of the SC - the cells undergo specialization as they migrate from the generative layer to the SC. Keratin fibres are progressively deposited. Lipid is also synthesized during the keratinocyte's epidermal transit - lipid seals the layers of dead cells, making the SC a very efficient moisture barrier. The lipid content of the horny layer is estimated to comprise as much as 20% of the SC's dry weight. The SC also contains moisture - about 15-20% of its dry weight. The water content increases 300 to 400% of the dry weight on some areas of the body when the skin becomes waterlogged through soaking. The skin is also hydrated when the natural evaporation of water is impeded by an occlusive dressing. - this results in increased elasticity of the tissue and increased ease with which the molecules diffuse within the tissue. Conversely, as the SC dries out, it becomes brittle, until it begins to split and fissure under stress hence chapped lips, windburn and dishpan hands. The selective permeability of the SC is the main barrier to the absorption of chemicals and protects the body from exogenous chemicals. Viable epidermis This interfaces with both the SC and the dermis. These are metabolically active cells. This layer is much more hydrophilic in nature than the SC, so drug diffuses easily through this region. Keratin molecules are actively synthesized by migrating keratinocytes in this layer. Dermis This is thicker than the epidermis. It consists mainly of a dense network of proteinaceous connective tissue (collagen, elastin) in a semigel matrix of mucopolysaccharide. Of importance is that the microcirculation that serves the entire skin is located in the dermis - the copious blood supply delivers oxygen, nutrients and immunological agents to the skin and removes waste products and chemicals absorbed transdermally. The blood supply also assists in thermoregulation and blood pressure regulation. The dermis is also penetrated by a network of sensory nerves and lymphatics, and by the eccrine glands (salty sweat glands) and hair follicles and associated pilosebaceous glands. Cells called melanocytes lie within and beneath the epidermal-dermal interface. They produce a pigment, melanin, which is then deposited into neighbouring keratinocytes. Pigment is continuously formed in and deposited in dark skins in response to the presence of melanocyte stimulating hormone (MSH). In light-skinned persons, little pigment is formed until the cells are stimulated by ultraviolet radiation whereupon "tanning" is initiated. Skin 's appendages Hair follicles - hairs are formed of keratinized cells compacted together into plates or scales - this takes place at the base of the follicle in the hair bulb. Sebaceous glands - these are associated with hair follicles (pilosebaceous glands) and secrete an oily material called sebum. This plasticizes and seals the SC and maintains an acidic condition on the skin surface (pH of 5). Eccrine glands (salty sweat glands) - found over virtually the entire surface of the body. They are particularly concentrated in the palms and soles. They secrete a highly dilute aqueous solution of salt. Apocrine glands - found only in the armpits, the anogenital regions and around the nipples. They secrete a milky substance containing proteins, lipoproteins, lipids and some saccharides. Bacterial action on apocrine secretions deposited on the surface of the skin is responsible for body odour. FUNCTIONS OF THE SKIN (Modern Pharmaceutics, 2nd Edition, GS Banker and CT Rhodes, pgs 263-273) The skin serves several protection and regulatory functions vital to the homeostasis of the body. GENERAL FUNCTIONS OF THE SKIN Containment of body fluids and tissues Barrier functions (protection from harmful external stimuli) Microbial barrier Chemical barrier Radiation barrier Thermal barrier Electrical barrier Reception of external stimuli Tactile (pressure) Pain Thermal Regulation of body temperature Synthesis and metabolism Disposal of biochemical wastes (in glandular secretions) Intraspecies identification and/or sexual attraction (apocrine secretions) Blood pressure regulation Containment This relates to the ability of the skin to contain the underlying tissues and restrain their movement from place to place. The strength to perform this mechanical role is mostly derived from the collagen and elastin fibrous matrix found in the dermis. The elastic character allows the skin to return to its normal contours and condition when stretching ceases. As one ages, the skin loses its elasticity, is stretched beyond the ability to restore itself and folds itself over in wrinkles. This process is accelerated through prolonged exposure to UV sunlight. The elasticity of the SC is dependant on a proper balance of lipids, hydroscopic water-soluble substances and water in conjunction with the keratin proteins. Water is the main softening agent and it takes about 15% moisture to maintain adequate pliability. The skin's "natural moisturizing factor' consists in part of amino acids, hydroxy acids, urea and inorganic ions as well as the skin lipids which hold water in the SC to plasticize it. Microbial Barrier The SC is an absolute barrier to microbes. Diverse microorganisms are found in the superficial cracks and fissures of the SC due to the continual sloughing - surgeons know to scrub their hands vigorously to remove microbes from these inner recesses. MO residing in the skin can initiate infection if seeded into living tissues as a result of damage to the SC caused by disease or mechanical trauma. The acidic pH makes the skin bacteriostatic. The dryness of the skin's surface also makes it unfavourable for microbial growth. Chemical Barrier The diffusional resistance of the SC is much greater than that of most body membranes. The ability of a chemical to breach the skin and the particular route which is taken is dependent on the physicochemical properties of the chemical. The intact skin is an extremely good chemical barrier. Radiation Barrier When the skin is stimulated by ultraviolet rays, melanocytes just beneath the epidermis produce a dark pigment, melanin, which is deposited in adjacent epidermal cells - tanning. Tanning is time-dependent and protection is developed over a period of time. Dark-skinned people are already heavily pigment protected and are thus less susceptible to burning. The epidermis thickens in response to UV radiation and this takes several days. The increased thickness itself contributes to the protection of the tissues underlying the epidermis.