Case Management Re-admission Strategy
advertisement
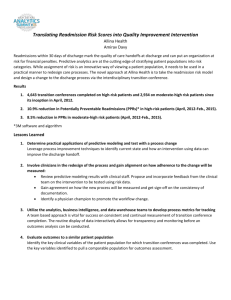
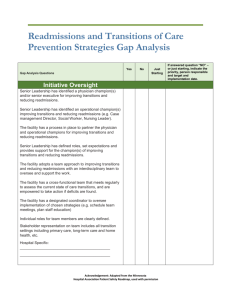
Best Practice Submission Case Management re-Admission Strategy Point of Contact: Sam Spencer, (210)297-1044, SJSPENCER@baptisthealthsystem.com Group Involved with the Project. The Baptist Health System VP CM, CMO, Nursing, Pharmacy, Allied Health, Quality Director Executive Sponsor: David Siegel, Dave Williamson Team members: Sam Spencer, CM directors Submitted by Major Moises Soto 11 May 2012 Executive Summary: The process of readmission due to continued complications for the same illness will become punishable under the new healthcare law starting October 2013. Under this new initiative, funding will be reduced for hospitals that do not show improvement to readmission rates, while facilities that achieve standards will benefit. The Baptist Health System has set a goal to develop a comprehensive continuity of care program that includes thirty days post discharge to improve patient care and reduce avoidable hospital readmissions. Patients identified as moderate to high risk for readmission in Acute Myocardial Infarction, Congestive Heart Failure, and Pneumonia have experienced a reduction in readmissions through one year post discharge as evidence by readmission rate reduction on a combined composite of 1.91% over four years. Objective of the Best Practice: This practice focused on several major factors that were identified through the re-admission process, which created a protocol that provided guidelines for staff to follow. Through this best practice, the staff was educated on the specifics of their individual responsibilities as well as the most comprehensive possible approach to implement them. Background: After the discharge process, patients tend to experience fragmented health care. This fragmentation leads to inadequate care, which results in elevated readmission rates. Having multiple nurses, and physicians involved in patient care allows for miscommunication during the transition to post-acute care. There is also a lack of outpatient follow-up post discharge, timely Primary care Provider (PCP) follow-up post hospital, and discharge instructions from hospital. The first factor the Baptist Health System used was to identify medication reconciliation to classify drug-to-drug interactions to avoid re-admission due to the mixing of medications. Incomplete discharge summaries were also addressed through staff education to ensure everyone addresses them the same way. Assigning dedicated roles focused on a specific cohort population suffering from Acute Myocardial Infarction, Congestive Heart Failure, and Pneumonia. Early identification included a comprehensive assessment completed within 24 hours of admission, and daily huddles for progression of care planning with case manager. The discharge planning also included an appropriate discharge plan within 24-48 hours of admission, home health or other post-acute interventions for moderate to high-risk patients. Scheduled primary care appointment 4-7 days after discharge identified patients appropriate for palliative or hospice care, and daily documentation in discharge notes by the Transition Care Manager. Coordinating the continuum of care began during inpatient care and includes Patient Health Record, regular communication and updates from post-acute care providers, awareness and escalation of “red flags”, missing physician appointments, and abnormal or declining patient health metrics. 1 Literature Review: The Baptist Health System approach to case management and re-admission strategy is based on Dr. Eric A. Coleman’s model. Dr. Coleman is a professor of Medicine and Head of the Division of Health Care Policy and Research at the University of Colorado, and Director of the Care Transitions Program, who has being at the fore front of an initiative aimed at improving quality and safety during times of care “hand-offs”. (Sullivan 2003) The baby boomer generation (1946-1964) has being setting trends since their inception. As this large part of our population grows older, they continue to dictate how products and services must evolve to ensure their proper care. Dr. Coleman’s approach is able to marry innovation and practice through: (1) enhancing the role of patients and caregivers in improving the quality of their care transitions across acute and post-acute settings; (2) measuring quality of care transitions from the perspective of patients and caregivers; (3) implementing system-level practice improvement interventions and (4) using health information technology to promote safe and effective care transitions. (Coleman 2008) Implementation Methods: Bridging a full continuity of care pathway started with daily patient contacts & telephonic management. In order to accomplish this, several high quality post-acute care partners were hired. These included but were not limited to: Interim Healthcare, Texas Home Health, Restorative Health Care, Gentiva Home Health, and Home care Dimensions. These institutions focused disease-specific programs and remote in-home monitoring. They also conducted physician follow-up appointment coordination with specialty-trained clinicians. These partners used Safe Life at Home Disease State Management Programs. These programs promote high quality decision-making by patients, which is believed to be critical to effective care management. According to Health Dialog (a leading provider of care management, healthcare analytics, and decision support). Individuals that participate in Shared Decision 2 making programs tend to choose less invasive care, and report being happier with both their care and with their health plan. (Health Dialog 2012) Results: Data collected for CHF, AMI, and PN since 2008 shows evidence of a downtrend in the amount of readmissions over the last four years. As a result BHS has dedicated staff models, and increased the amount of patient and family member interaction and education. Conclusion: The impact of implementing this BHS initiative has shown progress over the last four years demonstrating an improvement in the transition to post-treatment care. The initiative is working and the trend reflects an assimilation of new ideas and directives in the part of the staff. The system as a whole is becoming more efficient in the treatment of these three conditions on the 64 year an older population, as shown on table 1. Table 1 3 References Eric Coleman, MD, MPH | Department of Medicine | University of Colorado Denver. (n.d.). University of Colorado Denver. Retrieved April 26, 2012, from http://www.ucdenver.edu/academics/colleges/medicalschool/departments/medicine/hcpr/ Faculty/Pages/EricColeman.aspx Coleman, E. A. (n.d.). Care Transitions Intervention (sm) - Innovative Care Delivery Models. Innovative Care Models. Retrieved April 27, 2012, from http://www.innovativecaremodels.com/care_models/12/leaders Coleman, E. A., & Smith, J. D. (2002). Development and Testing of a Measure Designed to Assess the Quality of Care Transitions. International Journal of Care Integration, 2(April-June), 1-9. Retrieved April 18, 2012, from http://www.caretransitions.org/documents/Dev%20and%20Testing%20-%20IJIC.pdf Sullivan, H. P. (2003). mproving the Quality of Transitional Care for Persons with Complex Care Needs. Journal of the American Geriatrics Society, 51(4), 30-32. Retrieved April 19, 2012, from http://www.caretransitions.org/documents/Improving%20the%20quality%20%20JAGS.pdf The best medical decisions are those made together between doctor and patient.. (2012, February 7). http://www.Health Dialog.org. Retrieved April 24, 2012, from www.healthdialog.com/Main/Solutions/PopulationHealthSolutions/DECISIONDialog?g clid=CKSpo7HM8K8CFalgTAodsXmdYQ 4