Inf_Dis_Case_studies_Van_Etta_4-7
advertisement

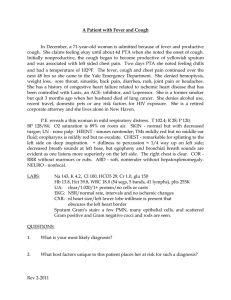
Case studies.Van Etta. 4-7-10-Heather Grothe 7 y.o. Girl Chief Complaint o Dysuria and urinary frequency x 2 days o No fever, flank pain, trauma, hematuria (gross), or emesis Physical Exam o Mild suprapubic tenderness o T-37.0, P-71 Dx? UTI Tests? UA, gram stain, culture UA o 100-200 WBC/hpf o 5-10 RBC/hpf Urine Gram Stain o 15-25 gram negative rods/hpf Specimen sent for culture RX: ___1. TMP/Sulf, _or trimethoprim_ Culture Grew o >100,000 ml E. coli sensitive to amoxicillin, sulfa, cefazolin, ciprofloxacin Recommended- concern is an anatomic malformation in recurrent UTI in kids. (collect system), abuse also in mind. o IVP o Voiding cystogram o Cystoscopy 27 y.o. Male Pediatric Resident Chief Complaint o Cough, chest pain, fever x 2 days, headache History of Present Illness o “URI” symptoms for several days o Developed nonproductive cough and fever o Day before admission noted right-sided pleuritic pain and cough productive of blood-tinged sputum Physical Exam o Moderately ill o VSS, Temp - 103ºF o Chest - fine, moist rales RLL posteriorly Dx? Pneumonia, Tests? Sputum and CXR Right side abnormal, infiltrate WBC-8,700/ul Legionella urinary antigen-neg- very specific and good to do, quick way to rule these out. Pneumococal urinary antigen-neg C-reactive protein-4.5 mg/dL Gram Stain (sputum) o Many PMNs o Few (+) cocci o Occasional (-) rod RX: ceftriaxone + azythromycin (atypicals) or just flouroquinilone Sputum culture - grew normal flora (probably mycoplasma b/c test are poor for this organism) 54 y.o. Female Chief Complaint o Pain in right leg, chills and fever History of Present Illness o Hx of phlebitis, now has chronic edema, especially right leg o 18 hours prior to admission noted pain in leg that became progressively worse o Few hours later noted redness, swelling & blisters; then chills and fever developed Physical Exam o VSS, Temp 102.6ºF o Right leg indurated, erythematous, swollen, large bullae from ankle to knee Dx? Cellulits :Staph (doesn’t move as fast) or streplooks like beta hemolytic strep, b/c she has recurrent edema (moves faster) Tests? Blood culture WBC-14,600 CRP-18.2 Blood cultures x 2-results pending Wound culture-moderate WBC, moderate Gram + cocci Rx: nafcilln, cephlasporin, clindamycin (to prevent toxin, works at level of ribosome) Blood culture and culture of skin lesions grew Group A beta hemolytic streptococci Patient improved with parenteral clindamycin and warm packs 69 y.o. Male Chief Complaint o Fever, cough, pain in left leg History of Present Illness o 10 days PTA fever and cough productive of purulent sputum o 8 days PTA severe pain left knee o 7 days PTA knee swollen, very hot and tender Physical Exam o Acutely ill, dyspneic o VSS, Temp – 103.6ºF o Chest - rales left mid lung field, posteriorly o Left knee - swollen, tender, erythematous, hot Dx? 1. Sepsis, 2. Pneumonia, 3. septic arthritis of knee Tests? Blood culture, sputum culture, tap the knee, cxr Left lower lobe pneumonia WBC-17.600 CRP-25.6 Blood cultures x 2 –results pending Creatinine-1.1 Other tests? Arthrocentesis o Turbid fluid o 70,000 WBC, 95% PMNs o Sugar - 15 mg%- low bugs eating o Protein - 6 grams %- too high Gram Stain o (+) cocci, in pairs RX: Gram + diplococci Blood cultures and synovial fluid grew Streptococcus pneumoniae Patient was treated with ceftriaxone (3rd gen ceph) 2 gms IV q 24 hrs for 4 weeks- also add vanco due to severe sickness and possible resistnace 56 yr old male Chief complaint : abdominal pain and fever HPI: 3 days of increasing abdominal pain, mild diarrhea, and fever to 100.4 P.E: T-38, BP-130/72, P-96, R-19 Lungs-clear, CV- RR, no murmur Abdomen- tender with rebound diffusely, absent bowel sounds Dx? Peritonitis (diffuse rebound and absent bowel sounds). Perforation usually causes peritonitis. (perferated ulcer or diverticulits) Tests? CT of abdomen, cbc WBC-18,600 with 92% neutrophils Creatinine-1.8, BUN-34 AST-24 Other tests? o CT abdomen/pelvis-diverticula of sigmoid colon with inflammatory changes, paracolonic inflammatory mass, and peritoneal fluid. Rx: antiobiotics (metronidazole (anaerobes) ceftriaxone, extended penicillin, carbipeneum, zosin, surgery Blood cultures were negative Peritoneal cultures grew-E coli, Bacteroides species, Fusobacterium species, Enterococcus faecalis, and Enterobacter cloacae Patient recovered after surgical resection of the sigmoid colon with formation of a colostomy and peritoneal irrigation combined with Antibiotic therapy- metronidazole combined with ciprofloxacin (enterobacter coverage) and piperacillin/tazobactam for 10 days 28 yr old female Chief complaint: confusion HPI: lives alone, found by her friend in bed at home this morning-confused, weak, unsteady on feet, speaking in nonsensical sentences Physical exam: T-37, BP 122/63. P-73, R-16 Lungs-clear, CV-RR, no murmur, Abd-soft, nontender Neuro-neck supple, expressive aphasia, DTRs-equal and reactive, toes down-going bilaterally Dx? Encephilitis, brain abscess Tests? CSF- WBC 34 with 72% mononuclear, RBC 75, glucose-64, protein-45 CSF- gram stain – few WBC, no bacteria seen CT brain- normal ( CT sensitive for abscess) Additional tests?- MRI of brain to better show herpes encephilits- won’t show up on CT MRI brain- enhancement of the temporal region on the left Rx: CSF PCR was positive for herpes simplex Patient recovered with intravenous acyclovir-10 mg/kg IV q 8 hrs for 21 days