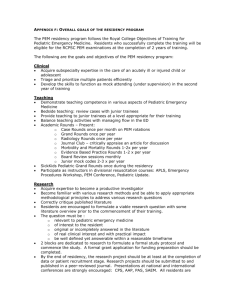
PICU Ch Ho NY - St. Barnabas Hospital
advertisement

PEDIATRICE INTENSIVE CARE – PL 3 Block Director: Dr. Katherine Biagas phone: x52315 page: 86742 ATTENDING INTRODUCTION During this rotation, third year residents will develop competency in Pediatric Critical Care. Residents will focus on the care and special needs of critically ill children, including disease processes, assessment, management and coordination of care. They will gain proficiency in the use of critical care technology and modalities. They will gain an in-depth understanding of physiology and pathophysiology. Patients will include infants, children and adolescents with serious medical conditions, traumatic injuries and complex surgical conditions including cardiac surgery, orthopedic surgery, neurosurgery and general surgery. Residents will coordinate care across the multiple disciplines involved in the patient care. They will provide ongoing education to families regarding their child’s condition. Lastly, residents will gain knowledge about the complex ethical and social issues that occur in caring for seriously or terminally-ill children. PATIENT CARE: PL 3 residents will act as primary physicians for patients admitted to the PICU, under the supervision of the pediatric critical care fellow and attending. Objective 1: Assess, resuscitate and stabilize a critically ill, unstable child. Indicators: Demonstrate ability to recognize respiratory failure and/or shock. Formulate a differential diagnosis and identify most likely diagnosis quickly, especially with respect to conditions that need immediate stabilization. Formulate and implement a plan to stabilize a patient, including respiratory and cardiovascular support. Demonstrate competency in skills necessary for age-appropriate cardiopulmonary resuscitation, including: o Airway management o Bag-valve-mask ventilation o Insertion of nasal and oral airways o Identification op priorities for vascular access o Establishment of appropriate vascular access o Administer fluid resuscitation MEDICAL KNOWLEDGE Objective 1: Understand core concepts of resuscitation and stabilization of critically ill child. Indicators: Describe physiology of respiratory and/or cardiovascular decompensation. Identify appropriate interventions including first line pharmacologic agents and understand their effects. Objective 2: Demonstrate an in-depth understanding of pediatric diseases and conditions or symptoms requiring intensive care unit management. Indicators: Describe the clinical presentation (and variations by age), pathophysiology, diagnostic and laboratory findings, age-management and prognosis of the following: General Ill appearing child Shock Single or Multi-system organ failure Severe dehydration Severe child abuse Allergy Angioneurotic edema Cardiorespiratory Congenital heart disease Respiratory failure or severe distress Severe asthma Apnea Cysnosis Tachyarrythmias and bradyarythmias Hypertension and hypotension Otolaryngology Congenital and acquired life-threatening upper airway obstruction/disease Tracheostomy management Endocrinology Diabetic ketoacidosis Adrenal crisis Other endocrinologic emergencies Gastroenterology Acute abdomen GI bleeding GI obstruction Infectious Disease Sepsis Toxicology/Pharmacology Accidental poisoning Overdoses of recreational drugs Overdoses of prescription medications Hematology/Oncology Acute illness or fever in patient with neutropenia/cancer Abnormal bleeding Oncologic emergencies (spinal cord or airway compression; electrolyte abnormalities, tumor lysis syndrome) Musculoskeletal Trauma to neck, back Severe trauma to extremities Neurology Acute brain injury Acute ataxia Coma, lethargy Seizures New onset weakness or paralysis Bulging fontanelle, stiff neck Psychiatry ICU psychosis Objective 3: Demonstrate an in-depth understanding of post operative management for surgical patients requiring PICU management. Indicators: Describe the clinical presentation, pathophysiology, surgical intervention, post-op management and prognosis for the following: Cardiac surgery o Congenital heart disease repair/palliation o Valve replacement o Cardiac transplantation Neurosurgery o V-P shunt placement o EVD placement o Removal of intracranial masses o Repair of intracranial vascular anomalies (AVM, aneurysm, etc) Orthopedics o Scoliosis spinal fusion o Other prolonged orthopedic surgeries ENT o Tacheostomy placement o Surgery on critical airway o Airway reconstructions o Repairs of congenital cranio-facial abnormalities Lung o Lung transplantation o VATS Trauma Other Surgery o Liver transplantation o Small bowel transplantation o Other complex surgery requiring intensive post-op care o Surgery on children with underlying complex medical problems Objective 4: Understand the indications for various diagnostic procedures, and interpret results to solve clinical problems and construct appropriate management plans. Indicators: For the following diagnostic studies discuss when the tests should be done and interpret the results during rounds. Blood test o CBC with differential o Blood chemistries: electrolytes, glucose, calcium, magnesium, phosphate, BUN, creatinine o Tests of hepatic function and damage o Serologic tests for infection o C-reactive protein, erythrocyte sedimentation rate o Drug levels o Coagulations studies o Blood gases o Urinalysis Cerebrospinal fluid analysis Imaging Modalities o Plain x-ray o CT scan o Magnetic resonance imaging o Ultrasonography o Nuclear studies o Fluoroscopy Cardiac tests o Electrocardiogram o Echocardiogram PRACTICE-BASED LEARNING & IMPROVEMENT Objective 1: Identify gaps in knowledge or expertise and demonstrate the ability to find relevant sources of information. Indicators: Identify a relevant article from a recent journal that addresses a clinical question that arose during a patient encounter, and report back to the team about the clinically relevant findings. Demonstrate proficiency in using the internet to find medically accurate information in a timely fashion. Objective 2: Participate in the education of patients and families. Indicators: Counsel patient and/or family about the current medical condition in terms that are appropriate to family’s a priori level of knowledge and confirm their level of understanding. Provide quality written material to the family regarding the child’s medical condition or treatment, if available. Objective 3: Identify gaps in procedural expertise and seek out opportunities to gain experience. Indicators: With appropriate supervision, participate in procedures with which the resident is not familiar or proficient at performing. Document procedures of the E-value website (Endotracheal intubation and Lumbar punctures need to be recorded on an on-going basis) INTERPERSONAL & COMMUNICATION SKILLS Objective 1: Communicate effectively with patients and families. Indicators: Demonstrate the ability to communicate effectively with patients and families using nonmedical language and avoiding jargon, so that they have a good understanding of the medical condition and management plan. Demonstrate the ability to communicate in a manner that is respectful of the diverse backgrounds of patients and families, including sensitivity to race, religion, culture and ethnicity. Demonstrate empathy in communicating bad news to patients and families. Objective 2: Communicate effectively with health care team, including other residents, fellows, attending, consultants, nurses, and allied health professionals. Indicators: Present on daily rounds in a clear, concise and organized manner such that the patient’s condition and management plan are transmitted and easily understood by the health care team. Communicate timely and accurate information to consulting services with a clear request for the specific input sought. Relay consulting services’ recommendations back to the team in a timely, accurate and thoughtful manner. Objective 3: Maintain accurate, timely and comprehensive medical records. Indicators: Write daily notes which are organized and coherent, contain all relevant information and clearly reflect the resident and team’s thought process and assessment/plan. Write event notes that are completed in a timely fashion, and include all information pertinent to the event (antecedent factors, the event itself, interventions, outcome, and changes in management plan). PROFESSIONALISM OBJECTIVE 1: Demonstrate a commitment to carrying out all professional responsibilities in a compassionate and ethical manner. Indicators: Approach the patient and family with open-mindedness, concern for their perspective and beliefs and sensitivity to their gender, age, culture, race, religion, disabilities and/or sexual orientation. In interactions with staff and other members of the health care team, consistently demonstrate respect through verbal and on-verbal behavior. Demonstrate a commitment to the patients’ best interest. Maintain patient confidentiality by limiting discussion about a patient and/or his/her medical condition to the bedside or to appropriately private settings. Demonstrate appropriate sensitivity and respect for a patient who is terminally ill or dying, and his/her family and other health care providers. Objective 2: Become familiar with the ethical and medical legal considerations in the care of critically ill children. Indicators: Discuss concepts of futility, withdrawal, and withholding of care. Define brain death and describe criteria for organ donation. As appropriate, participate in discussion with the family and attending regarding “Do Not Resuscitate” orders. SYSTEMS-BASED PRACTICE Objective 1: Understand cost considerations and incorporate risk-benefit analysis into decision-making and management planning. Indicators: Discuss the risks and benefits of utilizing expensive tests and consider whether a less costly modality would provide adequate information. Objective 2: Promote patient safety. Indicators: Consistently adhere to standard had hygiene practice and isolation procedures by donning appropriate persona protective equipment. Consistently adhere to standard hand hygiene practice and isolation procedures by donning appropriate personal protective equipment. Adhere to Hospital policy regarding patient identification confirmation. Ensure that home medications are reconciled in the electronic medical record on every admission. Objective 3: Understand resources and health care options for patients outside of the acute hospital setting (e.g. inpatient rehabilitation services versus home therapy) in order to facilitate discharge planning. Indicators: Under the supervision and with assistance from the social worker and patient care coordinator, discuss with a patient and/or family appropriate health care resources that are available to them. METHODOLOGY & EVALUATION As is true for much of residency, patient care and case-based reading will be the cornerstones of resident education in the PICU. Third year residents spend four weeks in the PICU; two of those weeks focus on cardiac pediatric critical care and the other two on general pediatric critical care. Third year residents take overnight call seven times in the four weeks. 2 of which will be weekend calls. Third year residents are on call overnight with at least one other pediatric resident covering all the PICU units, and sometimes more. In addition, a pediatric critical care fellow is on call at all times and oversees patient care in conjunction with a pediatric critical care attending. On post-call days, residents sign out to the other residents prior to morning rounds so that they can leave in a timely manner. Residents participate in daily patient rounds for all patients in the unit. They write daily notes, are responsible for ordering and following up on diagnostic evaluations, laboratory tests, and imaging studies, and for communicating ongoing changes in the management plan with nurses. They communicate directly with consulting services, and organize and relay recommendations from them to the health care team. They attend daily radiology rounds to review all diagnostic imaging on all the patients in the unit; this is an excellent opportunity to ask questions and learn about the radiologic findings and diagnostic modalities. They write comprehensive, organized transfer summaries for patients being transferred out of the unit to different services or facilities in order to ensure continuity of care. MANDATORY CONFERENCES: Chief of Service Rounds (Wednesday 8-9 am) and Grand Rounds (Fridays 8-9am) Attending Rounds on Thursdays from 7:30 to 8:15 am; these rounds will cover core topics in Pediatric Critical Care. Division Chief’s Rounds on Thursdays at 1:00 pm, led by Dr. Charlie Schleien Interdisciplinary Rounds on Tuesdays at 2:00 pm, includes multidisciplinary team and is focused on care coordination and discharge planning. Journal Club on the last Thursday of the month at 4:00 pm. RESOURCES: Peds CCM WEBsite at http//pedsccm.org with access to an electronic Pediatric Critical Care textbook, case report registry and evidence based medicine reviews. Textbook of Pediatric Intensive Care. Rogers MC, editor, Baltimore; Williams and Wilkins. Smith’s Anesthesia for Infants and Children. Motoyama EK, Davis PJ, editors, St. Louis; Moby, Inc. Evaluation: Link to the evaluation form which your attending will use to evaluate your performance.