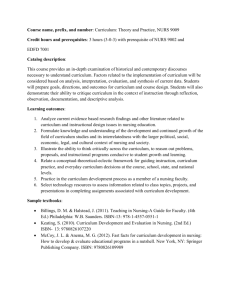
Orvis Handbook - University of Nevada, Reno
advertisement

1 Orvis School of Nursing Bachelor of Science in Nursing Program Undergraduate Student Handbook Approved: Revision: Updated: 12/22/2010 2 General Note This handbook is a document for OSN nursing students to find answers to policy/procedure guidelines and questions. It is important for undergraduate nursing students to be aware of the University’s policies and procedures for undergraduate programs and to understand the policies relevant to their program contained in the General Catalog. For more information about UNR’s Orvis School of Nursing (OSN) from the university catalog, visit their website at: http://www.unr.edu/ecatalog/Default.aspx. The following are the key points from the Undergraduate program materials, plus additional guidelines relevant to the BSN program. It is the student’s responsibility to be aware of and meet all requirements, general university requirements and OSN requirements and policies. Table of Contents Mission, etc. ................................................………………………………………..…page 3 University Student Judicial Code ……………………………………………. (http://www.cis.unr.edu/ecatalog/_(S(m3pnc545lxeef545f20f1kie))/Default.aspx?article _list_id=16029 BSN Curriculum …………........................................................................................... pages 3-6 BSN Pre-requisite Summary............................................................................. pages 3-5 Admission Requirements ................................................................................. pages 5-6 BSN Policies .............................................................................................. ................. pages 7-45 PEAP (Professional Ethics & Academic Policy) ……………………………. pages 7-16 Blood Borne Pathogen ………………………………………………………. pages 17-20 Blood Borne Pathogen Occurrence form …………………………………….pages 21-24 Undergraduate Clinical Absence Policy …………………………………….. page 25 OSN Grading Grid …………………………………………………………... page 26 Health Policy: Impaired Student ……………………………………………. pages 27-30 Tuberculosis Evaluation & Screening………………………………………...pages 30-31 Home Visitation ……………………………………………………………... pages 32-34 In Class Examination Procedures ………………………………………….....pages 35-36 Independent Study Guidelines & Worksheet ………………………………... pages 37-41 Progression Policy ……………………………………………………………pages 42-44 Safe Unsafe …………………………………………………………………..page 45 Student Uniform Policy……………………………………………………… page 46 Student Information...................................................................................................... pages 47-70 APA Format………. ……………………………..………………………….. pages 47-52 Communications of Concerns……………………..…………………………. page 53 Evaluation of Faculty………………………………………………………… page 53 NSNA Code of Conduct …………………………………………………….. page 54 NSNA Code of Academic & Clinical Conduct……………………………… page 55 UNR Student Conduct ………………………………………………………. (http://www.unr.edu/stsv/acdispol.html) Approved: Revision: Updated: 12/22/2010 3 Mission The mission of the Orvis School of Nursing at the University of Nevada, Reno is to prepare individuals for both entry level and advanced nursing roles by providing excellent academic programs integrating recognized educational standards. The curriculum emphasizes nursing care of individuals, families & populations throughout the lifespan; among diverse cultures & beliefs; and across all socioeconomic groups in the context of their environments by providing a strong foundation for evidence-based practice, critical thinking, and leadership. As an essential part of its mission as a land grant institution, Orvis School of Nursing provides service to the state of Nevada and to the professional community at large. Vision The vision of the Orvis School of Nursing at the University of Nevada, Reno is to be a leader in quality nursing education, research and service in partnership with our community of interest, locally, statewide and worldwide. BSN Pre-requisite Summary UNIVERSITY OF NEVADA RENO ORVIS SCHOOL OF NURSING BACHELOR OF SCIENCE in NURSING (BSN) CHECKLIST PRE-NURSING & MAJOR 2010-2011 Catalog Pre-Nursing Major (PM-NU) students apply to the nursing major a semester prior to completion of the prerequisites. Applicants may have up to 13 credits** remaining of which no more than 4** may be science credits to complete before entering the nursing major effective Fall 2011**. Students must have a 3.0 or better on selected* courses to apply (see below*). See additional guidelines on website before applying. **New parameter Name: _____________________ Advisor:______________________ University Requirements (CORE Curriculum) ENGL 101 ENGL 102 *CORE MATH (1) 3 cr 3 cr 3-5 cr CH 201 (2) CH 202 CH 203 3 cr 3 cr 3 cr *CHEM 121 (3) 4 cr PSY/ANTH/SOC or WMST 101 3 cr Approved: Revision: Updated: 12/22/2010 Major Requirements (Nursing Prerequisites) *CHEM 220A *CHEM 220L *BIOL 223 (5) *BIOL 224 (5) *BIOL 251 (5) 3 cr 1 cr 4 cr 4 cr 4 cr *HDFS 201 *Communication(6) *NUTR 223 (7) 3 cr 3 cr 3 cr *NURS 300 2 cr 4 *BSE (8) Fine Art 3 cr Diversity 3 cr Statistics (9) General Capstone(4) (300-400) 3 cr 3 cr 33 cr *Selected courses for nursing admission GPA 3 cr 34-36 cr Numbers in brackets ( ) correspond to page 2 comments. (http://www.unr.edu/catalog/ for course descriptions) NURSING MAJOR COURSE SEQUENCE Level I NURS 301 NURS 301LR NURS 317 NURS 318 NURS 331 Level II 3 cr 1 cr 3 cr 5 cr 3 cr 15 cr NURS 332 NURS 343R NURS 346 NURS 353 NURS 418R Level III 3 cr 2 cr 5 cr 4 cr 3 cr 17 cr NURS 433 NURS 434 NURS 439 NURS 441R Level IV 4 cr 5 cr 2 cr 2 cr 13 cr NURS 453 (10) NURS 454 NURS 485 4 cr 5 cr 3 cr 12 cr Credit & other Requirements (See additional guidelines on website before applying.) 128 Total Credits Required to graduate 64 credits from 4-year School required to graduate 64 Upper-Division credits required to graduate 59 credits from NURS major courses (11) To apply for the nursing major, one must be a current UNR student with a major of pre-nursing (PM-NU) for the semester prior to entering the major, obtain an accurate DARS report reflecting all pre-requisites with nursing admission GPA and complete the application process. Students for whom English is not their Native language must score > 55 on the TSE or SPEAK. Scores must be submitted with the application for consideration. Comment details (1) Nursing requires at least MATH 120. Please refer to CORE MATH in UNR catalog for any details. http://www.unr.edu/catalog/ (2) English requirement must be completed before taking Core Humanities. Students who place into English 102 are not required to complete English 101. (3) Math 120 is a prerequisite to CHEM 121. (4) General Capstone is not a prerequisite; it must be completed prior to graduation. Must be 300-400 level. Second capstone is in the nursing major (10). UNR requires junior standing (>60 credits) to take a Approved: Revision: Updated: 12/22/2010 5 capstone course. (5) BIOL 190, not required by Nursing, has a prerequisite of CHEM 121. BIOL 223 has a prerequisite of BIOL 190 & CHEM 121. BIOL 224 has a prerequisite of BIOL 223. BIOL 251 has a pre-requisite of BIOL 190. NO online courses accepted for science requirement or equivalent. (6) Approved courses: CHS 310: COM 202, 302, 312, 315, 400, 434. NO online courses accepted for communication requirement or equivalent. (7) NUTR 223 has a prerequisite of CHEM 121. (8) Behavioral Science Elective (BSE). See nursing advisor for suggestions; this is an elective that deals with human behavior. Suggest 300 or 400 level class. (9) Approved courses: PSY 210, or APST 207 or 270, STATS 152. Must take STATS 152 or APST 270 if CORE MATH is MATH126. (10) Major Capstone course. (11) May need 0-7 upper division credits outside of the nursing courses. BSN Admission Requirements Nursing Major Admission Guidelines OSN PROCESS AND PROCEDURE FOR STUDENT APPLICATION & SELECTION TO THE NURSING MAJOR The following guidelines are presented to help you submit a viable application to the nursing major. All applicants must adhere to the following criteria: 1) Be officially admitted to the University of Nevada, Reno as a pre-nursing major for the current semester. 2) Have a current, accurate, PM-NU DARS report with a catalog year of 2010. Applicants should meet with their advisor to ensure their DARS report is correct prior to submitting the application. NO APPLICATIONS WILL BE ACCEPTED WITHOUT AN ADVISOR’S SIGNATURE. 3) Have submitted and finalized all transfer credits which appear on the DARS report in the appropriate section. All pre-requisite courses and in progress courses must appear on the DARS report. If you have taken or are taking courses from another school(s) you must have official transcripts sent to UNR admissions. This will provide documentation and list the course as is in progress on the DARS. Once the course is completed a current official transcript must be submitted to UNR admissions showing that the course has been completed. Approved: Revision: Updated: 12/22/2010 6 4) Have no more than 13 pre-requisite credits outstanding or in progress with a grade no lower than “C” during the current semester before entering the nursing major. Of the 13 credits in progress no more than 4 credits may be science credits. 5) Selection to the nursing major is accomplished by a rank order list of qualified applicants based on the pre-nursing major GPA section from the submitted DARS report. 6) To be considered, applicants must have at least a 3.0 GPA or better on the selected pre-nursing coursework. 7) If English is not your Native language, you will need to take the TSE or SPEAK test. A score > 55 must be obtained for admission to the major. Scores must be submitted with your application for consideration. Please contact the Intensive English Language Center at UNR to schedule your speak test. 8) Submit the application form with your current permanent address (notification of acceptance and other correspondence will be sent to this address). 9) After completion of selection to the nursing major, the first 48 students will be sent a letter of acceptance. All selected students must reply to this letter to secure their official enrollment in the nursing major. 10) Letters of non-acceptance will also be sent to those who will remain on the waiting list until after the beginning of classes. No waiting list is maintained semester to semester. 11) Students may reapply during the next application period. If you have questions regarding the application or the information requested please make an appointment to see your advisor or contact Janita Ethridge (janita@unr.edu) at the UNR Orvis School of Nursing. Approved: Revision: Updated: 12/22/2010 7 University of Nevada, Reno Division of Health Sciences Orvis School of Nursing Professional Ethics and Academic Policy (PEAP) Introduction to the Professional Ethics and Academic Policy The Orvis School of Nursing, at the University of Nevada, Reno is dedicated to educating nursing professionals. Essential components of this education are truthfulness, insight and respect. Each member of the School of Nursing community, whether student, faculty or staff holds himself or herself and others to the highest standards based on the values of excellence, respect, diversity, integrity and accountability. Students enrolled in the Orvis School of Nursing are expected to conduct themselves in a manner that upholds the values of this institution of higher education. Each student is obligated to refrain from violating academic and professional nursing ethics principles and non-academic standards of standard outlined in the succeeding pages. Honor Pledge: The following honor pledge will be included and signed (on each examination), (with the receipt of every syllabus), (with each assignment): “On my honor, I pledge that I have neither given nor received any unauthorized assistance on this (exam) (syllabus) (assignment) (care plan) (paper) (project)” The pledge will be completed in several ways such as: • Student will write and sign the pledge • Faculty will preprint the pledge on tests and student will initial it • Faculty will include the pledge on an online quiz/test and ask students to indicate their online verification Professional Ethics and Academic policy violations: Plagiarism Cheating on exams Improper use of the internet Unauthorized use of electronic device for or during examinations (cell phone, PDA, calculator) Unauthorized collaboration Alteration of graded assignment Fabrication and falsification of data (patient or otherwise) or university documents (e.g., letters and transcripts), etc. Lying Facilitating academic dishonesty Infringement of the rights of others Violation of any rules and regulations of the University of Nevada and the School of Nursing (e.g., as outlined in the course syllabi, catalog, academic program manuals, website) Approved: Revision: Updated: 12/22/2010 8 Definitions Plagiarism Submission of the same or substantially similar work of another person, such as an author or classmate Improper documentation of quotations, words, ideas, or paraphrased passages taken from published or unpublished sources Use of the results of another student’s work (e.g., exam, papers, lab data, nursing care plan or other patient evaluation documentation) while representing it as one’s own Unauthorized submission of a paper as original work in one course when the paper has received credit in another course Cheating on Examinations Use of unauthorized materials (e.g., devices, notes, books) during an in-class, WEB-CT or take-home examination. Consultation of unauthorized materials while being excused (e.g., on a bathroom break) from an examination room Copying answers from another student or allowing another student to copy your answers Unauthorized discussion of an exam’s content during its administration Obtaining an examination or answers to an examination prior to its administration Studying from an old exam whose circulation was prohibited by the instructor Failing to comply with designated time limits for an academic evaluation without authorization Acting as a substitute for another or utilizing another as a substitute during an academic evaluation of any type Improper use of Internet Plagiarism from a published or unpublished Internet source Improper or lack of documentation of an Internet source Use of paper writing services or paper databases on the Internet Posting of patient/client data or photographs Unauthorized Use of Electronic Devices Consultation of unauthorized electronic devices (e.g., calculators, cellular phones, PDAs, computers) during examinations Approved: Revision: Updated: 12/22/2010 9 Use of electronic devices to communicate within or outside an examination room (e.g., use of cellular phones is not permitted during an exam) Storage of test answers, class notes and other references in electronic devices for use during examination Improper use during examination of email, text paging, beaming, and instant messaging Transmittal of patient/client data or photographs Unauthorized Collaboration Collaboration on homework assignments, papers, reports unless explicitly assigned or approved by faculty Alteration of Graded Assignments Submission of an examination or assignment for regarding after making changes to the original answers on test Forgery and Falsification Falsification or invention of data in such things as laboratory experiments, data analysis, patient evaluation Citation of nonexistent sources or creation of false information in an assignment Attributing to a source ideas or information not included in the source Forgery of university documents, such as academic transcripts and letters of reference Lying Request for special consideration from faculty or university officials based upon false information or deception Fabrication of a medical or emergency excuse as a reason for needing an extension on an assignment or for missing an examination or clinical Claiming falsely to have completed and/or turned in an assignment Falsely reporting an ethics violation by another student Facilitating Academic Dishonesty Intentionally or knowingly aiding another student to commit a violation of academic conduct Allowing another student to copy from one’s examination paper during administration of the exam, or another student’s work of any kind. Providing copies of course material whose circulation was prohibited (e.g., exams or assignments) to students enrolled in or planning to take that course Taking an examination or completing an assignment for another, or permitting one to do so Unfair Competition Willfully damaging the academic efforts of other students Stealing another student’s academic materials (e.g., book, notes, assignment, computer disks, etc.) Approved: Revision: Updated: 12/22/2010 10 Denying another student needed resources such as hiding library materials or stealing lab equipment Infringement on the Rights of Others Using behavior that jeopardizes the rights or safety of members of the OSN community, or jeopardizes the orderly functioning of University related activities Violation of any of the rules and regulations of the University of Nevada Reno and the Orvis School of Nursing include but are not limited to illegal use of drugs, firearms and sexual harassment Professional Code of Ethics Each student enrolled in the University of Nevada, Orvis School of Nursing is expected to uphold the professional code of ethics established for and by the nursing profession and as defined by the School. Ethics is foundational to the nursing profession. The nursing profession expresses its moral obligations and professional values through the Code of Ethics for Nurses (ANA, 2001). Each student should read the American Nurses Association Code of Ethics and be accountable for its contents. Professional Ethics In its Code of Ethics for Nurses, the American Nurses Association has stated that: “ethics is an essential part of the foundation of nursing. Nursing has a distinguished history of concern for the welfare of the sick, injured, vulnerable and for social justice. This concern is embodied in the provision of care to individuals and the community. Nursing encompasses the prevention of illness, the alleviation of suffering, and the protection, promotion, and restoration of health in the care of individuals, families, groups, and communities”. (American Nurses Association Code of Ethics for Nurses with Interpretive Statements, ANA website). Nursing students are expected not only to adhere to the morals and norms of the profession, but also to embrace them as part of what it means to be a nurse. The nurse recognizes that his/her first obligation is to the patient’s welfare and that all other needs and duties are secondary; the nursing student adheres to this same value. An ethics code makes the professional goals, values, and obligation of a nursing student more explicit, assisting the student in the development of his/her professional ethics. A nursing student at the School of Nursing will University of Nevada Orvis School of Nursing will strive to act in a professional, ethical manner in accordance with the Code of Ethics for nurses, and the Professional Academic and Ethics Policy. He/she will incorporate the following into his/her clinical practice: 1. Read the School of Nursing’s Professional Academic and Ethics policy and be accountable for its contents. 2. Be responsible for his/her own learning and clinical practice and honor other students’ right to learn and be successful in academic and clinical environments. (Example: develop own knowledge base through study and inquiry, recognize other’s right to do well on their written work, have access to reserved materials, and have access to their own preparation materials and supplies used in clinical areas). Approved: Revision: Updated: 12/22/2010 11 3. Demonstrate respect in verbal and non-verbal behaviors to all others in clinical and academic settings. (Example: Interact with others without using threats of, or commission of, physical harm, verbal abuse, unwanted sexual advances or contact, or other unwarranted physical contact. Arrive to class and clinicals on time; turn off beepers and cell phones in class, etc.). 4. Assess patient status carefully upon assuming responsibility for his/her care. 5. Provide safe, competent care, seeking assistance when personal knowledge and/or skill are not adequate. Avoid use of any substances that would impair clinical ability or judgment. (Example: prepare for clinical assignment to develop required knowledge and skill; review patient’s medical record; seek assistance according to course and curricular objectives) 6. Provide the same standard of care to all patients and families regardless of race, ethnicity, age, sexual preference, disability, religion, economic status, employment status, or the nature of their health problem. Accept that others have the right to their own cultural beliefs and values and respect their choices. (Example: demonstrate compassion and respect for every individual; provide the best quality of care possible to all patients; be non-judgmental of cultural differences). 7. Provide patient care without expectation of, or acceptance of, any remuneration. (Example: do not accept gratuities or personal gifts of monetary value). 8. Document in a thorough, accurate, truthful, and timely manner data that reflects findings from one’s own personal assessment, care, interventions, teaching, or the patient’s and/or family’s response to those activities. (Example: documentation errors are corrected in an acceptable manner, documentation is unaltered, vital signs are recorded at the time they are measured, and late entries are duly noted). 9. Act in a manner that contributes to the development and maintenance of an ethical educational and practice environment. Recognize that the primary commitment in clinical practice is to the patient and that respectful interactions are expected. (Example: act as a role model for other students and colleagues; speak up if another student is speaking disrespectfully to classmates or faculty; work through appropriate organizational channels to share concerns about situations that jeopardize patient care or affect the educational environment; advocate patient safety). 10. Complete legally required HIPAA training and University or clinical site requirements regarding confidentiality as required during the academic year. Use patient data in all school work, papers, presentations, research findings and in the clinical setting in a manner that is accurate, truthful, and confidential. Patient data must have a justifiable reason for its presence. Acknowledge real data gaps that may exist in written work. Identify patient in paper by initials, not full name. 11. Refrain from unauthorized use or possession of school or clinical setting’s equipment, patient’s belongings, or items dispersed or intended for patient use. (Example: Do not download University software onto a personal PC or palm pilot; do not use a hospital computer terminal for personal use such as playing online games; do not take a patient’s prescribed medication for personal use). Reporting Ethical or Academic Misconduct: The faculty and students at the Orvis School of Nursing expect that every student will maintain a high standard of individual honor and academic honesty while studying at the University. Any student who commits an act of academic dishonesty is subject to discipline. Approved: Revision: Updated: 12/22/2010 12 Allegations of academic ethics and behavioral misconduct are investigated and resolved using a standardized procedure. Generally faculty members initiate investigations, either by detecting violations themselves or by receiving reports from teaching assistants, clinical site staff, students and other university staff members. Students or staff who witness violations should report these to the appropriate course faculty, or the Chair of the PEAP committee. The faculty and/or chair of the PEAP committee will follow up on the reports by scheduling a meeting of the appropriate PEAP committee members. Both students and faculty should follow these procedures: 1. Overt violations of the Ethics Code that are well substantiated should be referred directly to the PEAP committee. 2. In the case of suspected academic ethics violations, the faculty member should meet with the student or students involved in the incident and the Chair of the PEAP committee to discuss the accusation. If the PEAP Chair and the faculty member believe the accusation has no merit, the issue can be dismissed, but the conversation must be documented and sent forward to the Director of the School of Nursing. 3. If after meeting with the student(s) involved, the PEAP Chair and faculty member believe the incident has merit, the PEAP committee members will be contacted and a meeting scheduled within the next 5 days. The PEAP committee will notify the Director of the School of Nursing of their Decision within 24 hours. Within 72 hours of the decision, the student will be notified of the PEAP committee’s decision by certified mail (this will allow for delivery of the letter via certified mail). PEAP Hearings: A Professional Ethics and Academic Panel will be constituted each year, and will meet annually in the Fall semester (after elections are held) and as needed thereafter. Five faculty members will be elected: two teaching predominantly in the baccalaureate program, two teaching in the graduate program, and one outside faculty will be selected from the full-time faculty of the University by the Director of the Nursing Program. The chair of the committee will be chosen by the members. One committee member must be a tenured faculty. The term of office is one year and can be renewed; a rotating election process will be used so that each year ½ of the committee is comprised of newly elected members. In addition to faculty, one student from each of the programs will be elected from the student body to serve on the committee. The composition of each PEAP hearing committee will be comprised of one ½ of the committee membership (1 faculty from the baccalaureate program, one from the graduate program and one student from the same program as the student involved in the hearing, along with the outside committee member). The committee chair will make the hearing member selection, after a discussion with all committee members. The PEAP committee chair will schedule a meeting within 5 days upon determining that any student incident has merit. At each hearing, the Director of the School of Nursing will appoint a recording secretary. Students and faculty will submit evidence directly to the chair of the PEAP committee 48 hours prior to the meeting. The PEAP hearing is an orderly discussion, not a legal proceeding. Legal representation is not permitted. The proceedings will be kept confidential by all parties. The hearing proceeds in this manner: Approved: Revision: Updated: 12/22/2010 13 • The party initiating the complaint will present an account of the events of the charge of academic or behavioral misconduct • Witnesses will be called to testify if appropriate • The alleged violator may refute the charges • The faculty and violator will be allowed to make closing arguments • At the conclusion of the meeting, all parties will withdraw, and the deliberations of the PEAP panel will be held in private • The alleged honor code violator and the initiating party will be informed in writing by the Chair of the PEAP panel within 5 working days of the panel’s decision • Depending on the severity and type of infraction, the student may be removed from the clinical or classroom immediately after a decision has been achieved. Such decisions will be communicated verbally to the student by the Chair of PEAP. Written confirmation will follow. Coordinators for the students program options (DNP, FNP, MSN, RN-BSN, BSN) will be notified by the Chair of the PEAP committee immediately following the decision of the committee verbally and by e-mail. Any student found not guilty will be exonerated of all charges Students found guilty face the following potential sanctions, based on the Panel’s determination of the severity of the infraction: • Failure on an assignment • Lowering of a grade or failure in a course (depending on the faculty syllabi) • Notation on a student’s transcript of an academic misconduct • Suspension or expulsion from the University In the case of students with prior offenses, the minimum sanction the PEAP panel may impose is failure in a course with a notation on the student’s transcript, which states that the grade resulted from academic misconduct. The Director of the School of Nursing maintains a file or meeting proceedings in a confidential file. The PEAP chair submits a report for the monthly faculty meetings. Students are not identified by name. Appeals Process: Students may appeal decisions of the PEAP panel in writing to the Director of the School of Nursing within 10 business days of the PEAP’s decision. The student’s statement will set forth the grounds for the appeal. The Director will have access to all documents reviewed during the PEAP panel’s hearing. The Director may meet with the accused and when necessary, with the accuser before reaching the final decision. The Director will present a written response to the student. Copies of all appeals correspondence will be sent to the chair of the PEAP committee, and Sally Morgan, Director of Office of Student Conduct. PEAP members will be notified of the Directors response by the chair of the PEAP committee. Records: Confidential records of the PEAP panel will be kept in the Director’s office. Student Experience: Being accused of an ethics violation is a stressful process for students. Students are encouraged to be completely honest in all discussions associated with this process and take advantage of University resources: Approved: Revision: Updated: 12/22/2010 14 The PEAP Chairperson will provide an overview of the process and procedures associated with evaluations, Ethics Code violations, and advice about preparing for the Professional Ethics and Academic Policy hearing. The counseling center can be of assistance with any personal difficulties during this process. In advance of the Professional Ethics and Academic Policy hearing, a student will receive written notification of the hearing date, time and location from the Chair of the panel. Students are required to attend the hearing as scheduled. Faculty Experience: Faculty members should enforce violations of academic ethics equally and consistently. All suspicions of academic misconduct, no matter how minor, must be investigated. As discussed earlier, faculty must contact the Chair of the PEAP committee to discuss accusations of academic misconduct. Coordinators for the program of study must also be notified. This is necessary to determine if an accused student has previous violations of ethics. Faculty members must submit documentation of all direct settlements and hearing requests to the Chair of the PEAP committee. If a PEAP committee meeting is necessary, it will be scheduled to fit the faculty member’s schedule Approved: Revision: Updated: 12/22/2010 15 Faculty are expected to compile evidence and to present their account of a case during a PEAP hearing. A faculty member on the PEAP committee will be chosen to assist the faculty with this preparation and process. Faculty members are encouraged to contact the PEAP chair to discuss concerns and questions about the meeting. (Adapted from the Johns Hopkins University School of Nursing) Approved by the Orvis School of Nursing Faculty: January 25, 2010 Approved by the Director of the Orvis School of Nursing: Patsy L. Ruchala, DNSc, RN Approved: Revision: Updated: 12/22/2010 January 25, 2010 16 Orvis School of Nursing Acknowledgement of Reading the Orvis School of Nursing Professional Ethics and Academic Policy By signing this document, I verify that I have thoroughly read the UNR-Orvis School of Nursing Professional Ethics and Academic Policy. Printed Name: Signature: Date: Approved: Revision: Updated: 12/22/2010 17 University of Nevada Reno Orvis School of Nursing Blood Borne Pathogen Exposure Guidelines I. Purpose and Policy The purpose of these guidelines is to reduce the risk of student exposure to blood borne pathogens such as, but not limited to, Hepatitis B Virus (HBV), Hepatitis C Virus (HCV), and the Human Immunodeficiency Virus (HIV). Standard Precautions is an approach to infection control that requires the application of blood and body fluid precautions for all patients and patient specimens regardless of diagnosis. Standard precautions will be the minimum standard of practice through out Orvis School of Nursing. Whenever possible Body Substance Isolation will be used. Body Substance Isolation takes Universal Precautions one step further and requires the same barrier precautions for all moist body substances and surfaces, not just those associated with the transmission of HIV and HBV. All human blood and body fluids will be handled as if they are infectious. II. Prevention of Blood Borne Pathogen Exposure Education and Training in Standard Precautions and Body Substance Isolation Procedures: Students will be required to participate yearly in Blood Borne Pathogen Exposure Prevention and Control Class during the first week of level one and level four clinical. The student must also have satisfactorily demonstrated skill in using personal protective equipment and procedures before receiving a patient care assignment. The OSN office will maintain documentation of yearly attendance. Hepatitis B Vaccine: Students will be required to have completed the hepatitis B vaccine series, have documentation of titer immunity, or to have signed a declination prior to going to clinical sites. Students may receive the series through Student Health Services, Washoe County Health Department, Orvis Nursing Clinic, or their own private health care provider. III. Methods of Compliance Students will become familiar and comply with the Blood Borne Pathogen Exposure Policy of the clinical sites to which they are assigned. IV. General Screening The Orvis School of Nursing will not undertake any program of screening faculty or students for antibody to HIV. Any student or faculty wishing to be tested will be referred to his/her private physician, the UNR Student Health Center, or the county health department. Approved: Revision: Updated: 12/22/2010 18 V. Accidental Exposure Incidents A student in the School of Nursing who has blood or body fluid exposure while in a clinical agency is treated in a similar manner to any type of accident occurring within the agency. The student should immediately notify the clinical faculty who will then immediately notify the supervisor within the health care facility where the accident occurred. As much information as possible about the source patient should be collected (i.e. HBV antigen, HCV and HIV antibody status). The clinical agency will require the completion of an incident/occurrence report and will usually ask for permission from the client to test for blood borne pathogens. The student should report to a health care provider within two hours to discuss post-exposure prophylaxis treatment. The student should be aware that post-exposure testing and post-exposure prophylaxis treatment is not a covered service at the UNR student health center. While testing and treatment may be initiated at student health services, the student will be required to pay for these services at the time of treatment. In the event of a blood borne pathogen exposure, it is imperative that the student know where and how to seek evaluation and care, as post exposure prophylaxis must be initiated with in two hours. Should the student have a private insurance policy (yourself, your employment, or through your parents); it is still necessary for students to determine if exposure to a blood borne pathogen is a “covered service” of their policy. The University of Nevada Reno is not liable for treatment or medication costs. Each student enrolled in the School of Nursing must carry health insurance and must provide validation of this coverage each semester to the program coordinator or designated staff. The insurance must provide coverage for exposure to infectious/communicable diseases. The cost of personal health care, including care required as the result of blood borne pathogen exposure in clinical practicum experiences, is not covered by the University, the School of Nursing, or the clinical agencies workman’s compensation policy. The University of Nevada Reno does have a Student Accident Insurance policy that would cover students for a blood borne pathogen exposure. The policy is limited to $10,000 and only covers the student in off campus locations (i.e. hospitals or non-university clinics). The coverage is only in effect while you are a student. The exposed student will be encouraged to have testing for HIV at baseline, 6 weeks, 12 weeks and 6 months. The decision to have testing or not, however, is the choice of the individual exposed. The clinical instructor and student will complete the OSN incident report to document the exposure. The faculty will forward the information to the Director of Orvis School of Nursing for follow up. The school of nursing will keep this documentation on file for a period of not less than ten years following the date of the exposure. Approved: Revision: Updated: 12/22/2010 19 The clinical instructor must notify the Director of the School of Nursing when a student has been accidentally exposed. Notification of the Administration is necessary to assist in the protection of the faculty and College in the event of subsequent liability issues or actions occurring following the incident. VI. Guidelines for Exempting Students from Clinical Assignment to Clients with Blood Borne Diseases: Confirmed Pregnancy: The risk of transmission of communicable diseases to pregnant health care workers is not known to be greater than the risk to those not pregnant. However, a pregnant student may not be eligible to receive triple therapy post-exposure prophylaxis in the event of a high-risk exposure due to the teratogenic effects of protease inhibiting medications. Based on the above information, there is no epidemiological reason to exempt pregnant students from caring for patients with blood borne diseases. Incompetent Immunological Systems: Students with diagnosed immunological deficiencies are at an increased risk for developing opportunistic infections that may be present in clients with blood borne diseases as well as other noninfected clients. The Centers for Disease Control (CDC) and the American Nurses Association do not recommend barring HIV-infected health care workers from practicing their profession, though in some cases, disclosure of the student’s status may be indicated and mandated by law. Students with HIV infection need not be restricted from clinical experience unless they have some other illness for which any health care worker would be restricted. Symptoms of HIV (i.e. fatigue, paresthesia, vision problems, or dementia) may limit a health care worker's ability to safely practice. Infections: Any student with an infectious process could further compromise the client with an incompetent immunological system. All students with exudative or weeping skin lesions should be restricted from direct client care contact. The decision to exempt a student from clinical experience will be made on a case-by-case basis by the faculty responsible for the clinical course. Decisions about longer exemptions (more than one clinical session) will be made in consultation with the student's physician and appropriate university faculty/administrators. Approved: Revision: Updated: 12/22/2010 20 VII. Student Acceptance of Clinical Assignment Students who have received formal classroom instruction in blood borne pathogen exposure control and can satisfactorily demonstrate knowledge and skills requisite to such care are expected to accept clinical assignments in order to meet the course objectives. The decision to exempt a student from clinical experience will be made on a case-by-case basis by the faculty responsible for the clinical course. VIII. Confidentiality Within the Code of Federal Regulations are statements designed to protect medical information and the privacy of the individual, providing there is no overriding need for the public to know. To mandate that a person infected with HIV be required or requested to notify College authorities is difficult, if not impossible to enforce and legally challengeable. Individuals involved with health care-giving services that know they are infected with a blood borne disease are ethically and legally obligated to conduct themselves responsibly in accordance with the following protective behaviors. 1. Seek medical advice. 2. Follow College and/or agency guidelines when involved in direct client care. 3. Be knowledgeable about and practice measures to prevent transmission of blood borne diseases. No specific or detailed information concerning complaints or diagnosis will be provided to faculty, administrators, or even parents, without the express written permission of the individual in each case except as required by law. This position with respect to health records is supported by amendment to the Family Education Rights and Privacy Act of 1974. Health officials and other institutional officers must remember that all confidential medical/health care information is protected by statutes and that any unauthorized disclosures may create legal liability. Revised April 2006 Approved by Director & OSN Faculty April 24, 2006 Approved: Revision: Updated: 12/22/2010 21 ORVIS SCHOOL OF NURSING BLOOD BORNE PATHOGEN & COMMUNICABLE DISEASE STUDENT EXPOSURE REPORTING FORM This form must be completed by the student in collaboration with clinical faculty for any exposure or potential exposure to a communicable disease that occurs during the course of a clinical rotation. An exposure or potential exposure is defined as a percutaneous injury or direct skin and/or mucous membrane contact with blood or body fluids or a reasonable belief that an exposure may have occurred. Please complete this form as thoroughly as possible. This form is required in addition to any form required by your clinical agency. While your first priority is to obtain appropriate exposure management and post-exposure prophylaxis therapy if indicated, this form must be completed prior to leaving clinical on the day that the injury or exposure occurred. This information will remain confidential and will be maintained in a locked cabinet at the Orvis School of Nursing for a period of not less than ten years following the exposure. Information in this form will remain confidential and will only be utilized by public health agencies in the mandated reporting of diseases, or as required by law. 1. Name of exposed individual: ___________________________________________________ Address: ____________________________________________________________________ Phone: _________________________ 2. Date of exposure: _________________ Date of Birth: _______________________ Time of exposure: ____________________ Exact location where exposure occurred (i.e patient room #, hallway, utility room): ___________________________________________________________________________ 3. Witnesses to exposure incident: Name: ___________________________ Name: ______________________________ Address: _________________________ Address: ____________________________ Phone #: _________________________ Phone #: ____________________________ 4. Describe the circumstances of the exposure: ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Approved: Revision: Updated: 12/22/2010 22 THE FOLLOWING SECTION IS APPLICABLE ONLY TO SHARP OBJECT INJURIES. IF THIS EXPOSURE WAS NOT THE RESULT OF A SHARP OBJECT INJURY, PLEASE CONTINUE TO PAGE 3. 5. Was the injured worker the original user of the sharp item? Yes No Unknown Not applicable 6. The sharp item was: Contaminated Uncontaminated Not applicable Unknown 7. For what purpose was the sharp item originally used: Unknown Injection into muscle, vein, or artery Heparin or saline flush Injection into (or aspiration from) IV injection site or IV port To connect IV line To gain intravenous access To draw a venous blood sample To draw an arterial blood sample 8. Did the injury occur: Before use of item During use of item After use of item Between steps of a multi-step procedure While recapping a used needle While withdrawing needle from a rubber port Device left on floor, table, or bed In transit to disposal While disposing of item After disposal/protruding from sharps container Other: ______________________ 9. What type of device cased the injury? Hollow Bore Needle Surgical Needle Lancet Glass 10. Brand/Manufacturer of product (i.e. ABC Medical Company): ________________________________________ Unknown 11. If the item causing the injury was a needle or a sharp medical device, was it a “safety design” with a shielded, recessed, retractable, or blunted needle or blade? Yes No Unknown Please mark the location of the injury a. Was the protective mechanism activated? Yes, fully No Yes, partially Unknown b. Did exposure incident happen Before activation During activation After activation N/A Approved: Revision: Updated: 12/22/2010 23 THE FOLLOWING SECTION IS APPLICABLE ONLY TO BLOOD AND/OR BODY FLUID EXPOSURES TO SKIN OR MUCOUS MEMBRANES. IF THIS EXPOSURE WAS THE RESULT OF A SHARP OBJECT INJURY, PLEASE CONTINUE TO PAGE 4 12. Which body fluids were involved in the exposure? Blood or blood products Saliva Vomit Sputum Amniotic fluid CSF Other: ________________________ Peritoneal fluid Pleural fluid Urine 13. Was the body fluid visibly contaminated with blood? Yes No Unknown 14. Was the exposed part: Intact skin Non-intact skin Eyes (conjunctiva) Mouth (mucosa) Not applicable Nose (mucosa) Other: __________________________ 15. Did the blood or body fluid: Touch unprotected skin Soak through protective barrier garment Touch skin between gap in PPE Soak through clothing 16. Which barrier garments, if any, were worn at the time of exposure: Latex/vinyl gloves Face shield Protective gown Goggles Surgical mask Lab coat Eyeglasses Other: ______________________ 17. If the exposure was the result of an equipment failure, please specify: Equipment type: _________________ Manufacturer: __________________ 18. For how long was the blood or body fluid in contact with your skin or mucous membranes: < 5 minutes 5 – 15 minutes 15 minutes – 1 hour > 1 hour 19. How much blood/body fluid came in contact with your skin or mucous membranes? Small amount (< 5 cc) Moderate amount (up to 50 cc) Large amount (> 50 cc) Please mark the location(s) of the exposure Approved: Revision: Updated: 12/22/2010 24 SOURCE PATIENT DATA & POST-EXPOSURE FOLLOW UP 1. Name of student: ________________________ 2. Date of injury: ________________________ 3. Was the source patient identifiable Source known and tested Source known, but not tested Source not known 4. Was the source patient known to be positive for any of the following pathogens (check all that apply): Hepatitis B Respiratory tuberculosis Hepatitis C Bacterial meningitis HIV Other: ______________________________ 5. If the source patient was believed to be in a high risk group for a blood-borne pathogen, please check all that apply: Blood product recipient Hemophilia Injection drug use Sexual history Elevated liver enzymes Dialysis Other: _______________________________ 6. If the source patient was known to be HIV+, has s/he been treated with any of the following: Zidovudine Not applicable 3TC Unknown ddC Other anti-retroviral: ____________________ IDV 7. Student seen and exposure evaluated by (check all that aply): UNR Student Health Clinical agency employee health Private health care provider No follow-up care received Emergency room Other: __________________________ 8. Was the student vaccinated against HBV before exposure? No 1 Dose 2 Doses 3 Doses 9. Was the student pregnant at the time of the exposure? Yes, 1st trimesterYes, 2nd trimester Yes, 3rd trimester No Not applicable 10. What follow up care was received after evaluation of this exposure: None Other prophylaxis: ________________________ Baseline testing only HAART post-exposure prophylaxis Other: __________________________________ April 12, 2006 Approved: Revision: Updated: 12/22/2010 25 Clinical Requirements And Expectations For Undergraduate Students Absence From Class or Clinical / Reporting Illnesses There shall be no official absences in any university class. It is the personal responsibility of the student to consult with the faculty regarding absence from class or clinical. Absence from clinical classes at Orvis School of Nursing for long term illness requires immediate notification of the Undergraduate or Graduate Coordinator and the OSN Director for administrative direction with input from the involved faculty. Orvis School of Nursing Clinical Absence Policy In the event of illness or emergency, when a student cannot meet clinical obligations, the student must do the following: a. Notify the clinical faculty b. Notify the clinical agency c. Follow up with the faculty regarding his/her absence Clinical absence due to a personal or family illness or some other emergent event of more than two days (15 hours) in any one semester will reduce the student’s final grade for that semester by 2% for each day of clinical missed. Documentation of illness or emergent event may be requested by the faculty. There will be no make-up of clinical time missed for this reason. Other clinical absences, in any one semester, for a voluntary reason, will automatically decrease the student’s grade by 2% for every absence in that semester. Make up time, as negotiated with faculty, will be required for one voluntary absence. More than four days of missed clinical time from any one student, for any reason, will fail the student in that semester and not allow the student to progress in the nursing major and/or to graduate. (Approved by the OSN Faculty and Director: May 15, 2006) Approved: Revision: Updated: 12/22/2010 26 ORVIS SCHOOL OF NURSING UNDERGRADUATE GRADING GRID POLICY UNIVERSITY OF NEVADA, RENO DIVISION OF HEALTH SCIENCES Purpose: To provide consistency in grading across the Orvis School of Nursing undergraduate curriculum. The following grading scale is to be used by the Orvis School of Nursing faculty for all undergraduate courses: A AB+ B BC+ C CD+ D DF 93 or > 90-92.9 87-89.9 84-86.9 81-83.9 78-80.9 75-77.9 72-74.9 69-71.9 66-68.9 63-65.9 <63 Approved by the OSN Faculty: November 1, 2004 _______________________________ Patsy L. Ruchala, DNSc, RN Director Approved: Revision: Updated: 12/22/2010 __________________ Date 27 Health Policies: Impaired Nursing Student The faculty recognize that all persons of our society, including nursing students, are susceptible to illnesses that may impair their ability to function at an optimal level. When a student develops an illness that impairs the ability to learn and to provide safe nursing care it is of special concern. In the case of chemical dependence, disease development may be facilitated or accelerated by occupational risk factors such as easy drug access and pharmacological model of dealing with high stress, emotional distress and pain. Given the occupational components of nursing that require safe, effective care, the following policy and procedure for identification, intervention and treatment in situations of actual or potential student impairment has been developed. Impairment is defined as being under the influence of psychoactive substances and/or evidencing psychological or physical symptoms. This can be episodic or chronic and affects cognitive, interpersonal and psychomotor learning and performance. Faculty beliefs that underlie this policy are: That the use of psychoactive substances while performing or learning to perform nursing care is not acceptable. That when a student's performance is impaired, safe, effective care is at risk whether it occurs in the classroom, learning skills laboratory or in the clinical setting. That alcohol and drug abuse and addiction are primary illnesses as are psychiatric and physical illnesses and each can be successfully treated with rehabilitation and return to optimal function. That students who are willing to cooperate with a program of assistance to them and accept treatment, rehabilitations and monitoring should be allowed to continue their nursing education, provided they cooperate fully and comply with requirements for treatment and monitoring of their continued well being. This applies for any illness causing impairment. That habitual impairment is cause for disciplinary procedure, as are those students identified as impaired or potentially impaired who are unwilling to be rehabilitated. Legal transgressions such as theft, falsification of records, diversion of drugs for sales or to supply another, or the substitution, alteration or denial of prescribed medications to patients involves the disciplinary process as well as the assistance process. The purpose of this policy is to: Encourage students who self identify themselves as having physical, cognitive or emotional conditions affecting their performance to seek and receive evaluation, treatment and/or professional licensure. Approved: Revision: Updated: 12/22/2010 28 Identify and assist students who have not yet recognized signs of potential impairment in themselves or identified themselves as having medical or emotional conditions leading to future impairment. Procedure Actual or potential impairment is identified through the recognition of signs of deteriorating performance including but not limited to: Problems with lateness, missing clinical time Increasing numbers of incidents and errors with nursing care Observed or reported incidence of interpersonal conflict Complaints of poor quality nursing care Decreased productivity Awkward, ineffective, inaccurate psychomotor skills Peers and others attempt to compensate for the imbalance of care and learning by overlooking impaired performance, lateness and absenteeism. Self identification and report Student will be referred for professional evaluation and treatment if this is not in process. Conference will be arranged with Director of OSN to decide the following (with input from counselor or therapist); Continued attendance at OSN and any restrictions Schedule of reports on progress and rehabilitation Plan for relapse prevention (student responsibility) One time incident Faculty observe, assess and document performance and objective data. Student faculty conference at which time student is informed of the reasons she/he must leave clinical (symptoms of illness, impairment and lack of required safe, professional behaviors). Arrange for someone to drive home and give student assignment for make-up work. Set appointment for next conference. Be sure student leaves. Inform undergraduate curriculum coordinator and Director of OSN. At preset second student-faculty conference provide follow-up guidance: discuss behavior and/or signs of illness; establish expectations and limits for future behavior of student (designate time period); encourage student to give his/her perception of situation and plans to prevent further unprofessional behaviors. Record relevant information. Send copy to student and OSN director. Ongoing pattern Consult with OSN Director. Review all documentation of related incidents. (In custody of director). If pattern of observable, objectified quantified behaviors identified, arrange for conference with student. Prepare for intervention through collaboration with counseling service. Approved: Revision: Updated: 12/22/2010 29 At intervention conference, inform student of concern, observed pattern of impairment and need for professional evaluation as a condition of continued professional education. Refer for evaluation with prearranged appointment. Student will be initially evaluated by Director of UNR Counseling Center or Director of Student Health. If student refuses referral, disciplinary procedures may be indicated. May need involuntary withdrawal. After evaluation, Director of OSN will request conference with student and their advisor. o If illness is not identified, a contract will be established outlining unacceptable behavior and a time frame for improvement including clear consequences if change does not occur. o If student identified as chemically dependent or to have any other illness or condition that impairs judgment and/or performance, she/he will be asked to enter treatment and/or withdraw and enter treatment and rehabilitation (depends on the severity of the condition and prognosis). Documentation will be maintained in separate, confidential files in the Director's office, and will include conditions for continuing in the program, copies of professional evaluation, diagnosis and treatment recommendation. The student will be informed of implications for licensure and given a referral list of NSBON Requirements for maintaining documentation and reports of treatment and rehabilitation will be including possibility of restricted clinical expectations. Approved by OSN Faculty, Spring 1997 Signs And Symptoms Of Intoxication Data indicating need for removal from clinical, evaluation and documentation. Odor of alcohol Unsteady gait Rapid or slurred speech Blood shot eyes Fine motor tremors Dilated or pinpoint pupils Difficulty with calculations Inability to follow directions N/V or sweating without known cause Some of the above may be due to/explained by another cause. If this is found to be true, above should still be documented in clinical notes and observed over time. The following all indicate possible intoxication and should be addressed if not related to a known cause and a pattern of these exist. Look for a pattern and document clearly and accurately. Sleepiness, dozes off Shuns interaction, long lunches alone Avoids eye contact Errors in judgment in patient care Approved: Revision: Updated: 12/22/2010 30 Frequent disappearance from clinical site without explanation Tardiness, leaves early, short term absences Odor of mouth wash or breath mints Lapses in memory, incongruent responses, difficulty in recalling instructions. Improbable, elaborate excuses and apologies for behavior Prefers to work alone, seeks less supervision or avoids, with draws from other students Inconsistent performance, sudden changes in usual behavior Direct blame onto others Defensive and irritable Inconsistent stories and explanations Difficulty meeting deadlines and schedules Frequent reports of illness accidents or emergencies Unusual interest in giving medications or pain medications (i.e., deprives peers of opportunities) Frequent behavior of impaired student nurses Tuberculosis Evaluation And Screening Policy Orvis Nursing students who routinely work in health care facilities treating individuals are at high risk for infection that all persons present in their agency are disease free and/or protected from infection. Purpose 1. Identify people with TB infection and possible TB disease. 2. Treat persons with identified infection. 3. Evaluate persons infected and treated on continuing basis. Procedure: TB Screening and Evaluation All students are skin tested yearly prior to entering any clinical facility. A baseline two-step Mantoux will be done on all students who have not had a documented two-step Mantoux test and documented yearly negative Mantoux tests within each 12 month period after the baseline (This includes persons who have had BCG vaccination and women who are pregnant). The test to be done is the Mantoux test with 0.1 ml of PPD tuberculin injected intradermally. It will be read 48-72 hours after injection. If the test is negative a second test is given 1-3 weeks later. If this test is positive it is considered a 'boosted' reaction (due to TB infection that occurred a long time ago). If the reaction to the second test is negative the person is considered uninfected. Annual testing within 12 months of the original test and prior to this anniversary date thereafter can be done with a single Mantoux test. If an individual has had a negative Mantoux test within the last 12 months, a second Approved: Revision: Updated: 12/22/2010 31 Mantoux will be done and this is considered the same as a two step/baseline test. Single annual testing is done thereafter. Students who are exposed to suspected TB patients in the course of their clinical experience will follow the guidelines of that facility or seek advice and testing from student health services. A person with a documented history of a positive Mantoux tuberculin skin test is exempt from future skin test or chest x-rays. A person with a current positive skin test will have a chest x-ray once prior to entry in to the nursing major and medical evaluation for active tuberculosis on required physical exam. A person with a history of TB or a positive TB test will have documented yearly medical evaluations for the presence or absence of symptoms of TB. A person with active TB will undergo medical treatment for the disease according to the American Thoracic Society. References: Nevada Administrative Code 441A.375, 441A380, CDC March 1995. Approved by APSA 10/23/95 Approved by OSN Faculty 12/4/95 Revised for student exposure 12/20 MAL Approved: Revision: Updated: 12/22/2010 32 UNIVERSITY OF NEVADA, RENO ORVIS SCHOOL OF NURSING NURS 434 – COMMUNITY HEALTH NURSING PRACTICUM CLIENT VISITATION POLICY Policy Statement Community health faculty have supervisory as well as faculty roles in the course. Students in the Community Health Practicum are under direct Orvis School of Nursing (OSN) faculty supervision for all client care provided. The clinical faculty member is the registered nurse of record, unless there is a situation where the student is under the supervision of agency staff when direct care is provided. Indirect faculty supervision responsibilities include communication and direction among and between students, agency personnel, clients, families, and any interdisciplinary team members. Purpose To ensure the safety of the OSN students, faculty, community clients, and families while providing optimal learning experiences. Policy A. Safety considerations are the highest priority. Faculty will work in collaboration with the student to maintain safety for students, faculty, and clients. 1. If, at any time during a visit, conditions or individuals appear threatening or unsafe for ANY reason, leave the site immediately. Always respect “gut feelings”. Always be aware of your exit route. 2. Students MUST work in pairs when visiting clients. If a student is working with an agency, the agency representative will be considered as their “pair” for the day. 3. All home visits will be completed during assigned clinical times. If an appointment is needed at a time other than assigned clinical time, the student must receive permission from the clinical faculty. Such requests must be typed, provide rationale for making the visit at the requested time, and be submitted in advance of the scheduled visit. 4. Students making client visits without an agency representative will provide the clinical faculty with a daily schedule of visits. Students will complete the “Student Daily Itinerary Data Sheet” prior to beginning their visit(s) and assure that the faculty is aware of their itinerary. If any changes to the itinerary are necessary, faculty must be notified prior to altering the schedule. 5. The student(s) must notify their faculty member upon completion of the visit(s). If the faculty member is not contacted, the OSN Director may be notified and appropriate action taken. 6. Student name badges will use with first name and first initial of their last name only. Name badges are to be worn at all times. Approved: Revision: Updated: 12/22/2010 33 7. Students will not give out their personal contact information (phone number, address, etc.) to clients. Any contact should occur through their faculty member. 8. Students traveling in their own vehicle will maintain the vehicle in good repair and assure that their gas tank is at least one-half full. 9. At no time will students use their own vehicle to transport clients or client family members/friends. Similarly, students will not ride in a client’s vehicle. 10. Vehicles will be parked in plain sight near the site of the client visit. Do not park in areas of questionable safety (alley ways, deserted streets) or with poor lighting. 11. All valuables, including laptop or hand held computers, purses, backpacks, etc., should be secured out of sight in the vehicle. B. Client Visit Considerations and Guidelines 1. The OSN document “Client Consent Form” must be completed prior to initiating care for any community-based client visited without agency personnel present. 2. All health promotion activities and nursing interventions in the home will occur within the framework of the client’s current medical plan of treatment and the Nevada Nurse Practice Act. 3. If practical, clients will be called to confirm appointment prior to the visit occurring. 4. Professional, therapeutic relationships are of the utmost importance. Please use appropriate titles (i.e. Mr. Jones or Mrs. Cannon) and refrain from using terms of endearment such as “honey” or “sweetie” when speaking with clients. 5. Students will give written or oral report on client visits to their faculty member within 24 hours of the visit, earlier if conditions warrant. 6. Written documentation of student-client interactions will be maintained throughout the semester. All documentation will be kept with the faculty member when not being directly utilized by the student nurse. 7. Patient confidentiality will be maintained by using a unique identifier on all documentation created by OSN student nurses with the exception of the “OSN CLIENT CONSENT FORM”. The identifier will include the initials of the client as well as their date of birth in the following format: ABmmddyy. Example DS120799. 8. The following forms will be used as appropriate: OSN CLIENT CONSENT FORM OSN OBSERVATION NOTE OSN CLIENT GOALS Approved: Revision: Updated: 12/22/2010 34 OSN STUDENT NURSE TO STUDENT NURSE UPDATE REPORT OSN REQUEST FOR RELEASE OF INFORMATION OSN FINAL SUMMARY OSN STUDENT NURSE TO AGENCY REFERRAL OSN STUDENT DAILY ITINERARY OTHER FORMS OR DOCUMENTS AS APPROPRIATE Approved: Revision: Updated: 12/22/2010 35 In Class Examination Procedure Each course faculty, at the beginning of course, will provide students with the following information orally and in writing: Criteria utilized for evaluating student performance. Specific weight given to examinations. Examination format (essay, multiple choice, etc.). How the final grade is derived. Faculty will also announce the duration of any examination and time the question and answer sheets and/or essays must be retrieved, immediately prior to the beginning of any examination. At the end of each written examination, all examination questions must be turned in with the answer sheets. Faculty will keep examination materials for one year. The following procedures have been established to insure that, in the specific area of course examinations, the standards of professional behavior of Orvis are maintained: Proctoring A uniform method of proctoring examinations has been established with proctors clearly instructed as to their responsibilities and duties. Written examinations will be given in areas that provide easy visibility, for example, large lecture halls. The proctors must ascertain that each student has cleared his/her desk area of all material prior to the examination. Seats in the lecture halls may be numbered. When examinations are given in these areas, students will be asked to record the seat number on the answer form. Examination booklets and scantron sheets may be numbered. A sufficient number of faculty proctors will be present to insure the honesty of the examination procedure. At least one of the proctors will be a faculty member whose function is not only that of a proctor but who is also able to answer any questions during the examination. Faculty responses will be uniform and available to all students taking this examination. The faculty and undergraduate coordinator will establish the need for and numbers of proctors. Student Behavior During Examinations Students are expected to behave professionally during examinations. Academic Dishonesty of any kind is incompatible with behavior considered inherent in becoming a nurse. The existence of firm guidelines during the examination period emphasizes the commitment of administration and faculty to neither foster nor tolerate such behavior. Guidelines include: Approved: Revision: Updated: 12/22/2010 36 Students may not communicate with one another during examinations. Students will be seated in a wide distribution to diminish the opportunity of academic dishonesty. Books, note pads, calculators, and hand-held electronic information systems may not accompany students to their seats and will be left in the front of the room. Open-book exams are the exception to this procedure. Students who leave the room during an examination must leave their examination material with the proctor and may be asked to sign in and out of the room. Students taking examinations are expected not to communicate the contents of the examination to those students who have not yet taken this examination. Identification of Students Suspected of Academic Dishonesty The following procedures will be actuated, in the event that the proctor observes students exchange written communication with one another, a student copying from another student's examination paper, or a student to be in possession of and/or utilizing written material improperly brought into an examination: Any illicit material will be confiscated. The point to which the examination has proceeded, as well as the students ID number, will be recorded. However, the student will not be permitted to complete the examination. Corroboration with another proctor is encouraged where possible. See UNR catalog, Academic Standards and OSN PEAP Policy for disciplinary process guidelines. The OSN Administration in conjunction with the involved faculty and student will handle all administrative actions. Approved: Revision: Updated: 12/22/2010 37 Independent Study Guidelines: Undergraduate Purpose: An Independent Study is designed to further develop concepts and/or theory learned and acquired in previous academic arenas that encompass an area of nursing interest for the student. The student must be able to pursue the learning activities and research with autonomous, intellectual ability, and display appropriate independent study behaviors. Learning objectives must be established at the outset to guide the student toward the ultimate outcome used to establish ground rules for the learning experience as it progresses toward the outcome. Pre-registration activities for the student: (to be completed toward the end of the prior semester or one month before semester begins). The student must determine an area of desired interest for learning with a written purpose for the study. Establish a relationship with a faculty member for supervision throughout the independent study (this is a must prior to registration). The student must write preliminary objectives that are to be discussed with the supervising faculty member of record. These objectives may be revised and finalized in number of content based on the mutual interaction of the student and the faculty member (see section on objectives for more information). Complete worksheet for preparation only and does not constitute a learning contact. Activities for the faculty of record: The faculty member of record will be responsible for the following inclusions in the independent study. Preparations (resulting either from preparation by the student or mutual agreement with the student): A student statement of the purpose for the study that is appropriate for the level of his/her study and preparation. Learning objectives that are adequate to achieve the intended outcome of the learning experience. The number of credit hours registered for are commensurate with the academic endeavors of the established independent study contract. Select a method of measuring the achievement of the objectives for the assignment of a grade (Usually by discussion with the student). Establishing a regular, repeating conference schedule for the student to discuss progress and objective achievement with the faculty of record. Approved: Revision: Updated: 12/22/2010 38 The faculty of record in conjunction with the student will be responsible for establishing and maintaining a time line for the independent study. The student must complete all stated objectives and desired activities within this time frame. If the independent study involves a practice component, the faculty of record has the responsibility of monitoring by observations or/on site interaction with the student and preceptor a minimum of three (3) times over the course of the time line. The faculty of record will then assign a grade at the conclusion based on the outcome of the study. The faculty role will be to guide the student toward the desired outcome by discussion during conference time, responding in the journals kept by the student, and by maintaining the time line for the study. Description of study types: There are basically three types of study - theory research, clinical practice, or a combination of these two prior types involving theory research and application practice. The university catalog provides the following course descriptions on the subject of those available through the Orvis School of Nursing. Opportunity for students to master areas of knowledge through independent organization and assimilation of materials under the guidance of faculty advisors. Variable 1-6 credit (s) choice. The number of credits registered for may never exceed the maximum of 6. The course number can be used a multiple of times until the maximum is reached. These are not read on the student's record as repeated courses. Nurs 490 - Special problems and practices in nursing. Individual or group study in areas relevant to nursing theory and/or practice. Variable 1-10 credit (s) choice. The number of credits registered for may never exceed maximum of 10. The course number can be used a multiple of times until the maximum is reached. These are not read on the student's record as repeated courses. Credit hour recommendation based on type and time: The faculty of record will exercise judgment to determine with the student what would be appropriate credit hours to register for based on the type of study to be pursed and the time commitment required for the student to meet the objectives. It is recommended that the same hours of actual classroom time be translated into independent study opportunities. For example: A theory only oriented study would involve a three hour per week commitment for the student, to include the conference time and research in the library. The recommended credit hours for registration would be three (3) credit hours. A theory/practice combination study may require five (5) credit hours to be divided into 1 hour of conference, 1 hour of research and three hours of practice per week. The division of the time into the areas of conference vs. Research vs. Practice needs to be determined as part of the learning contract for the student. The arrangement of how and when these hours for credit will be achieved is part of judgment to be exercised by the faculty member. Approved: Revision: Updated: 12/22/2010 39 Written learning objectives: The number of credit hours for independent study should serve as a guide for the number of learning objectives written, as well as, the specificity of information provided in the objective. The minimum number of objectives recommended is five (5) and it is suggested that central concepts (or paradigm) of nursing be considered and addressed in the study objectives. The central concepts specifically are person, environment, health and nursing. Other objectives will be determined through discussion between the student and faculty member. They should be considered in relation to the topic (s) of interest for the student. The number of objectives should expand to meet the number of credit hours sufficiently and reasonably. The language of the objectives may also have bearing on the number of objectives written. These are also left to the judgment of the faculty member as long as the intended idea is clear and measurable. These suggestions are not meant to considerations to be made prior to the registration for independent study. Method of measuring achievement: The student and faculty member will jointly decide the desired method of measuring his/her success on a predetermined basis that will be commensurate with the type of study and number of credits for which he/she will register. Options for the methods of measurement are papers, written critical thinking exercises, class presentations as a guest speaker, article preparation for publishing, journals, or any other creative means mutually decide upon by both parties. Combinations of the aforementioned may also be a consideration to meet the level of academic time commitment for the student. Specific requirements may be asked by the faculty of record prior to the implementation of the learning contract and should be written in the summary of the independent study arrangements. The method of measurement may be inclusive of the scheduled conference times that are the student's responsibility to meet by agreement with the faculty member (see the section on independent study conferences). Establishment of grading criteria: Criteria for grading should be included in the summary for the independent study. A standard by which to establish these criteria is provided here, but is not intended to be the absolute upon which to base performance in achieving the objectives. These suggestions are: Grade Level A. A high performance level is demonstrated in the achievement the intended purpose of the study by meeting all requirements independently without redirection. Grade Level B. An above average performance level is demonstrated while achieving the intended purpose of the independent study with minimal redirection. Grade Level C. An average performance level is demonstrated while achieving the intended purpose of the independent study with redirection consistently needed at times. Grade Level D. A below average performance is demonstrated in achieving the intended purpose of the independent study with consistent redirection. Grade Level F. Failure to achieve the intended purpose of the independent study with frequent redirection and constant reminders of the learning objectives and time lines. Approved: Revision: Updated: 12/22/2010 40 Independent Study conferences: The student and faculty or record should establish a schedule of regular meeting dates throughout the study time line to meet and discuss the progress of the student. The topic matters of these discussions should pertain to the knowledge the student is acquiring. The student would have the opportunity to discuss difficulties and barriers encountered as well as the progress toward the outcome of the study experience(s). Should the student need re-direction and counseling on his/her performance or progress toward achieving the objectives, it should be in summary at the end of the conference with expectations clearly defined. These should be documented for the record using the specifics of the objectives and other essential requirements of the study that have been documented in the independent study summary. These comments may be used to determine the outcome grade of the study. Independent study summary: A document entitled Independent Study Summary should be prepared providing the student's name and contact information, the final version of the written learning objectives, the method of measuring achievement, the conference schedule, and the grading criteria for the student and faculty record. Included on this document should be the last revision date. This should be completed prior to the implementation of the study by the student and be kept by the faculty of record. The student should be given a copy for reference throughout the study time. A copy may also be placed in the student file in the Orvis School of Nursing office. Length of independent study: The length of the study will have a finite length of time within the grading period allowed by the Orvis School of Nursing. Preparation for the study should be addressed with adequate time allowances prior to registration and implementation of the study. Suggested time frames for the student is to begin working on the required elements of the independent study toward the latter part of the prior semester (or at least a month before the fall semester) allowing a relationship with the faculty member to develop and solidify. The faculty has an option of disengaging from the proposed independent study if the required elements are not properly or adequately the independent study. The student must have the preliminary work completed and have an agreeing faculty of record before registering for the independent study. Revised 12/2010 MAL Approved: Revision: Updated: 12/22/2010 41 INDEPENDENT STUDY PREPARATION WORKSHEET* *intended use of this worksheet is for preparation only and does not constitute a learning contact. Student’s Name ____________________________________________________ Orvis School of Nursing level of study completed: 1 2 3 (circle one) Anticipated graduation date: _____________ Number of credit hour to be registered for (choose 1-10): ____________ Faculty of record for supervision: ________________________________________ Contact Number(s): ___________________________________________________ Independent study area of interest: Reason for pursuit of independent study: Preliminary study objectives (discuss these with your faculty member of record when complete): Use additional paper as needed to address the objectives. *intended use of this worksheet is for preparation only and does not constitute a learning contact. Approved by faculty 4/98. Revised to combined worksheet & guidelines 12/2010 MAL Approved: Revision: Updated: 12/22/2010 42 Progression Policies A. Students eligible to progress to the upper-division nursing major must meet the following requirements: 1. Submit a formal application to the School of Nursing by the date specified by the Admissions, Progression and Student Affairs (APSA) committee. No more than 13 prerequisite credits can be outstanding for the semester prior to admission. No more than one science course may be taken in the semester prior to admission. 2. Earn at least a 'C' grade in all prerequisite courses. The cumulative grade-point average earned in selected prerequisite courses is used to determine which students are selected to the upper-division nursing major. 3. Complete all prerequisite course requirements for the major by the end of the first summer session for admission in fall and by the end of fall semester for spring admission to the nursing major. 4. Students must have a minimum GPA of 3.0 on the selected courses qualify for application to the upper-division nursing major. 5. Have junior classification at the University of Nevada, Reno by the end of the application period for admission to the nursing major is required. 6. Take all prerequisite courses for a grade, and not on a satisfactory/unsatisfactory (S/U) basis. Transfer credit and courses taken for S/U credit are evaluated on an individual basis. Applicants with diverse backgrounds are encouraged to apply. The Orvis School of Nursing actively supports the University of Nevada, Reno's policies that ensure equal opportunity/ affirmative action and diversity. Nursing Sequence B. In order to progress within the nursing sequence, students must meet the following requirements: 1. Maintain at least a 2.0 cumulative grade-point average and achieve no less than a grade of “C” or satisfactory in each nursing course 2. Students in the upper-division nursing major may have to withdraw from the program for academic or non academic reasons. If a student withdraws, the following criteria are considered in determining whether the student may re-enter the nursing major: a. Beginning with the admission date to the upper-division nursing major, students are allowed three years to complete requirements for graduation. Withdrawal Academic Withdrawal: Students who are failing a nursing course, those who are considered clinically unsafe, or those students who have received less than 'C' as a final grade will be given the option to return to the upper-division Approved: Revision: Updated: 12/22/2010 43 nursing program on a space available basis during the following academic year. Following withdrawal for academic reasons, students may re-enter the upper-division program only one time. See process below. Nonacademic Withdrawal: Students who withdraw from the program for 'personal reasons' are required to present a written explanation at the time of withdrawal. The explanation must clearly state the exact reason for withdrawal, whether the student plans to return to the program, and the expected date of re-entry. The student must be receiving a 'C' in clinical and all theory courses at the time of withdrawal. The privilege to return to the program is given at the discretion of the director of the School of Nursing in consultation with the Admissions, Progressions/Student Affairs Committee. Following withdrawal from the program for nonacademic reasons, the student's re-entry is at the discretion of the Director of the School of Nursing in consultation with the Admissions, Progressions/ Student Affairs Committee. See process below. Readmission: space available basis Students who seek readmission to the upper-division nursing program must, at least four months prior to their return, meet the following requirements: 1. see their adviser at least four months prior to the appropriate academic semester to complete a withdrawl & readmission petition 2. withdraw from classes according to the following guidelines: a. student must withdraw from a class after earning a less than a ”C” grade and other courses as specified here b. Courses which must be taken or dropped as a unit: 1. NURS 301R, 301LR, 317R, 318 2. NURS 343R, 353, 346 3. NURS 433, 434, 439 4. NURS 453, 454 c. Courses which may be continued: NURS 331, 332, 418R, 441R, 485 3. apply directly to the APSA Committee at Orvis School of Nursing in order to be reconsidered for readmission 4. inform the Director of the School of Nursing of their intent to return to the upper-division program 5. formulate & follow a plan for remediation and readiness to demonstrate competency in academic & nursing skills 6. confirm that the problems causing their academic or nonacademic withdrawal have been resolved Students who withdraw and request readmission to the upper-division nursing major must: 1. show evidence of follow-through with specified plans made upon withdrawal and intent to return. Approved: Revision: Updated: 12/22/2010 44 2. Understand that placement back into the nursing major depends upon space available and whether the student has met the readmission plan and has met current School of Nursing requirements for the major. Withdrawing students in the RN/BSN program are considered on an individual basis. Petitioning C. Students, after consulting with their adviser, may petition for course substitutions or other considerations pertaining to the Orvis School of Nursing's curriculum requirements. If a student completes required courses more than l0 years before applying to the nursing major, the courses must be evaluated. Requests for course substitutions or waivers must be submitted to the Admissions, Progressions/Student Affairs Committee by petition for consideration and recommendation to the Director of the School of Nursing. Grading D. The following criteria for satisfactory/unsatisfactory (S/U) grading applies: Students pursuing the bachelor's degree may earn a maximum of 30 semester credits in courses graded on an S/U basis. Special Examinations E. Those students who have taken special examinations must meet the following requirements: 1. Students can earn credit by special examinations in accordance with university policies. 2. Students who are registered nurses may earn up to 29 upper-division nursing credits by special examinations. F. Individual students may be provided with the opportunity to pursue areas of interest through independent study courses. Note: see special nursing major application and admission guidelines Revised 12/2010/MAL Approved: Revision: Updated: 12/22/2010 45 Safe/Unsafe Clinical Practice Any of the following behaviors are sufficient grounds for faculty to determine that a student is clinically unsafe and cannot continue in the clinical practice course. This decision has serious consequences and adequate documentation is necessary. Failure to meet clinical objectives. Placing self, patients, co-workers, families and other human contacts in physical jeopardy. Refusal/failure to follow OSN regulations and agency protocols. Illegal behavior. Verbally or otherwise revealing confidential information. Failure to execute critical elements of procedures/protocols/practice. Absences/tardiness (see Policy on Absences). Inability to articulate rationale for care given to patients/clients. Dispensing inaccurate, untrue information. Failure to comply with Clinical Evaluation Tool (CET) Guidelines Revised 12/2010 MAL Approved: Revision: Updated: 12/22/2010 46 University of Nevada Orvis School of Nursing Uniform Dress Code The standard uniform consists of: White uniform top Navy blue uniform pants Solid white socks with white shoes, or solid navy blue socks with navy/black shoes. No canvas or open-toe shoes. Open-back shoes are permitted, but must be worn with the strap in position to hold the shoe on. Short white uniform lab coat Any shirt worn under the white uniform top must be white only, without decoration Photo identification tag worn at all times when in the clinical setting on the uniform top or lab coat Approved uniforms are available from: Renown Health Wear Plus 1155 Mill Street Reno, NV 89502 Telephone: (775) 982-5071 Fax: (775) 982-5005 Email: dbarone@renown.org 12/08 Approved: Revision: Updated: 12/22/2010 47 Approved by Faculty: 10/23/06 APA Format for Orvis School of Nursing th The following is from The Publication Manual of the American Psychological Association 5 edition. I. Format of the Paper a. Double-spaced throughout the entire paper b. 12-point Times New Roman typeface c. One inch margins all around d. Page numbers in the upper right-hand corner. Page one is the title page and is numbered. e. Header i. An abbreviated form of the title is placed five spaces before the page number on each page. II. Acronyms a. Must be spelled out completely for the first use and can then be abbreviated throughout the rest of the paper. i. Intensive Care Unit (ICU) III. Style a. Must be in third-person style. No “I, we, us, etc.” IV. Title Page a. Running Head i. An abbreviated title, in ALL CAPS flush left at the top of the page. The phrase “Running head” is before the abbreviated title in upper and lowercase. ii. The paper’s full title is centered on the page. Lower and uppercase are used. iii. No more that 50 characters are used in the running head, not including the words “Running head”, but including spaces b. The author’s name is below title and Orvis School of Nursing is below the author’s name followed by the date of the paper. V. The first page of the text a. The title of the paper is in uppercase and lowercase centered on the first line VI. Headings a. One level: i. Use level one: Only centered uppercase and lowercase headings b. Two levels: i. Use level one: Only centered uppercase and lowercase headings ii. Then level three: Flush left, italicized, uppercase and lowercase c. Three levels: i. Use level one: Only centered uppercase and lowercase headings ii. Then level three: Flush left, italicized, uppercase and lowercase iii. Then level four: Indented, italicized, lowercase paragraph heading ending with a period. The text begins directly after the period. d. Four levels: i. Use level one: Only centered uppercase and lowercase headings ii. Use level two: iii. Use level three: Flush left, italicized, uppercase and lowercase Approved: Revision: Updated: 12/22/2010 48 Approved by Faculty: 10/23/06 iv. Use level four: Indented, italicized, lowercase paragraph heading ending with a period. The text begins directly after the period. e. Five levels: i. Use level five: Centered Uppercase ii. Levels one, two, three and four follow VII. In Text Citations a. One author i. (Author, Year) b. Two authors i. (Author & Coauthor, Year) c. Three to five authors st i. 1 citation: (All authors, Year) ii. Any citation thereafter: (First author et al, Year) d. Six or more authors i. (First author et al., Year) e. Multiple sources from the same author: i. Chronological order, separated by comma 1. (Author, 1998, 1999) f. Multiple sources within same year i. (Author, 1999a, 1999b, 2000) g. Multiple sources within the same citation i. Separate sources by semicolon, alphabetical order ii. (Burke, 1998; Perez, 1992; Wilhite, 2001) VIII. Direct Quotes a. Quotation marks are used. Before the period, the (author, year, and p. #), then period i. “xxxxxxxx” (Smith & Jones, 2004, p. 365). ii. According to Smith and Jones (2004), “xxxxxxxxxx” (p. 365). 1. The word “and” is used instead of the ampersand symbol b. Electronic Sources i. May not be able to use page number. If not, a paragraph number should be used for the reader to locate the quote. 1. According to the American Nurses Association, “xxxxxxxxx” (2006, ¶ 52). c. Direct Quotes 40 or more words i. Quote is started on a new line ii. Block indention for the full quote iii. No quotation marks iv. Double-spaced v. Page reference appears after final period. i.e. xxxxxxxx. (p.3) IX. Citation of Secondary Sources a. Mays states ………… (as cited in Smith & Jones, 2003). b. Smith and Jones’ article would be in the reference list, not Mays’ X. Personal Communications (letters, emails, personal or telephone interviews) a. Cite only within the text b. Personal Communications are not included in reference list. c. (J.D. Smith, personal communication, May 1, 2006). Approved: Revision: Updated: 12/22/2010 49 Approved by Faculty: 10/23/06 XI. Reference Page a. The word “References” is centered in uppercase and lowercase b. References are listed in alphabetical order by author’s last name and then by year. c. Hanging indentation is used d. The author’s last name is followed with a comma and the initials. The ampersand symbol is used when listing more than one author. e. The title of the work has only the first letter and the first letter following a colon capitalized f. Journal article titles are not italicized, but the title of the journal, volume number and issue are italicized g. Book title are italicized and only the first word of the title is capitalized Approved: Revision: Updated: 12/22/2010 50 Approved by Faculty: 10/23/06 APA Format Running Head: APA FORMAT FOR THE ORVIS SCHOOL OF NURSING APA Format for the Orvis School of Nursing John Doe Orvis School of Nursing May 1, 2005 Approved: Revision: Updated: 12/22/2010 1 51 Approved by Faculty: 10/23/06 APA Format 2 Title of Paper Centered Uppercase and Lowercase on First Line Text of paper begins here. (Indented ½” or five spaces) LEVEL FIVE HEADING IS CENTERED UPPERCASE Level One Heading is a Centered, Uppercase and Lowercase Heading Level Two is a Centered, Italicized, Uppercase and Lowercase Heading Level Three is a Flushed Left, Italicized, Uppercase and Lowercase Heading Level Four is an indented, italicized, lowercase paragraph heading ending with a period. In level IV heading, text begins directly after the period. Approved: Revision: Updated: 12/22/2010 52 Approved by Faculty: 10/23/06 APA Format References (Journal Article) Auerbach, D. I., Buerhaus, P. I. & Staiger, D. O. (2000). Associated degree graduates and the rapidly aging RN workforce. Nursing Economics, 18(4), 178-184. (Book) Creswell, J. W. (1998). Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage Publications. (Book Chapter) Micklewright, J. (1994). The analysis of pooled cross-sectional data. In A. Dale & R. B. Davies (Eds.), Analyzing social & political change: A casebook of methods. London: Sage Publications. (Electronic Media) Robert Wood Johnson Foundation. (2002). Healthcare’s human crisis: The American nursing shortage. Retrieved February 25, 2006, from www.rwjf.org/pubications/publicationspdgs/nursing_report.pdf Approved: Revision: Updated: 12/22/2010 3 53 Communication Of Student Concerns The student has the obligation to express concerns by utilizing the following order of communication guidelines set forth by the Orvis School of Nursing. 1. Conference with instructor involved. 2. Conference with advisor. 3. Conference with Undergraduate/Graduate Coordinator. 4. Conference with the Director. 5. Conference with the Dean. Evaluation of Faculty By Students The University By-Laws require that faculty members be evaluated annually in order to assess the quality of professional performance of academically assigned responsibilities. Students will be expected to participate in the evaluation process by objectively rating the faculty's teaching effectiveness in the classroom and clinical settings. Professional responsibilities are a requirement for tenure, promotion or merit recognition. Students should be aware of the importance of their role in this evaluation process. Approved: Revision: Updated: 12/22/2010 54 National Student Nurses’ Association, Inc. Code of Professional Conduct As a member of the National Student Nurses’ Association, I pledge myself to: • Maintain the highest standard of personal and professional conduct. • Actively promote and encourage the highest level of ethics within nursing education, the profession of nursing, and the student nurses’ association. • Uphold all Bylaws and regulations relating to the student nurses’ association at the chapter, state and national levels, reserving the right to criticize rules and laws constructively, but respecting the rules and laws as long as they prevail. • Strive for excellence in all aspects of decision making and management at all levels of the student nurses’ association. • Use only legal and ethical principles in all association decisions and activities. • Ensure the proper use of all association funds. • Serve all members of the student nurses’ association impartially, provide no special privilege to any individual member, and accept no personal compensation from another member or non-member. • Maintain the confidentiality of privileged information entrusted or known to me by virtue of an elected or appointed position in the association. • Refuse to engage in, or condone, discrimination on the basis of race, gender, age, citizenship, religion, national origin, sexual orientation, or disability. • Refrain from any form of cheating or dishonesty, and take action to report dishonorable practices to proper authorities using established channels. • Always communicate internal and external association statements in a truthful and accurate manner by ensuring that there is integrity in the data and information used by the student nurses’ association. • Cooperate in every reasonable and proper way with association volunteers and staff, and work with them in the advocacy of student rights and responsibilities and the advancement of the profession of nursing. • Use every opportunity to improve faculty understanding of the role of the student nurses association. • Use every opportunity to raise awareness of the student nurses’ association’s mission, purpose, and goals at the school chapter level. • Promote and encourage entering nursing students to join and become active in NSNA. • Promote and encourage graduating seniors to continue their involvement by joining professional nurses’ associations upon licensure as Registered Nurses. Adopted by the 1999 House of Delegates Pittsburgh, PA at the 47th Annual NSNA Convention References: American Society of Association Executives and the National Society for Fund Raising Executives. Approved: Revision: Updated: 12/22/2010 55 National Student Nurses’ Association, Inc. Code of Academic and Clinical Conduct PREAMBLE Students of nursing have a responsibility to society in learning the academic theory and clinical skills needed to provide nursing care. The clinical setting presents unique challenges and responsibilities while caring for human beings in a variety of health care environments. The Code of Academic and Clinical Conduct is based on an understanding that to practice nursing as a student is an agreement to uphold the trust with which society has placed in us. The statements of the Code provide guidance for the nursing student in the personal development of an ethical foundation and need not be limited strictly to the academic or clinical environment but can assist in the holistic development of the person. A CODE FOR NURSING STUDENTS As students are involved in the clinical and academic environments we believe that ethical principles are a necessary guide to professional development. Therefore within these environments we: 1. Advocate for the rights of all clients. 2. Maintain client confidentiality. 3. Take appropriate action to ensure the safety of clients, self, and others. 4. Provide care for the client in a timely, compassionate and professional manner. 5. Communicate client care in a truthful, timely and accurate manner. 6. Actively promote the highest level of moral and ethical principles and accept responsibility for our actions. 7. Promote excellence in nursing by encouraging lifelong learning and professional development. 8. Treat others with respect and promote an environment that respects human rights, values and choice of cultural and spiritual beliefs. 9. Collaborate in every reasonable manner with the academic faculty and clinical staff to ensure the highest quality of client care 10. Use every opportunity to improve faculty and clinical staff understanding of the learning needs of nursing students. 11. Encourage faculty, clinical staff, and peers to mentor nursing students. 12. Refrain from performing any technique or procedure for which the student has not been adequately trained. 13. Refrain from any deliberate action or omission of care in the academic or clinical setting that creates unnecessary risk of injury to the client, self, or others. 14. Assist the staff nurse or preceptor in ensuring that there is full disclosure and that proper authorizations are obtained from clients regarding any form of treatment or research. 15. Abstain from the use of alcoholic beverages or any substances in the academic and clinical setting that impair judgment. 16. Strive to achieve and maintain an optimal level of personal health. 17. Support access to treatment and rehabilitation for students who are experiencing impairments related to substance abuse and mental or physical health issues. 18. Uphold school policies and regulations related to academic and clinical performance, reserving the right to challenge and critique rules and regulations as per school grievance policy. Adopted by the NSNA House of Delegates, Nashville, TN, on April 6, 2001 Approved: Revision: Updated: 12/22/2010