ERAS Collaborative Pathway Summary Word Document
advertisement
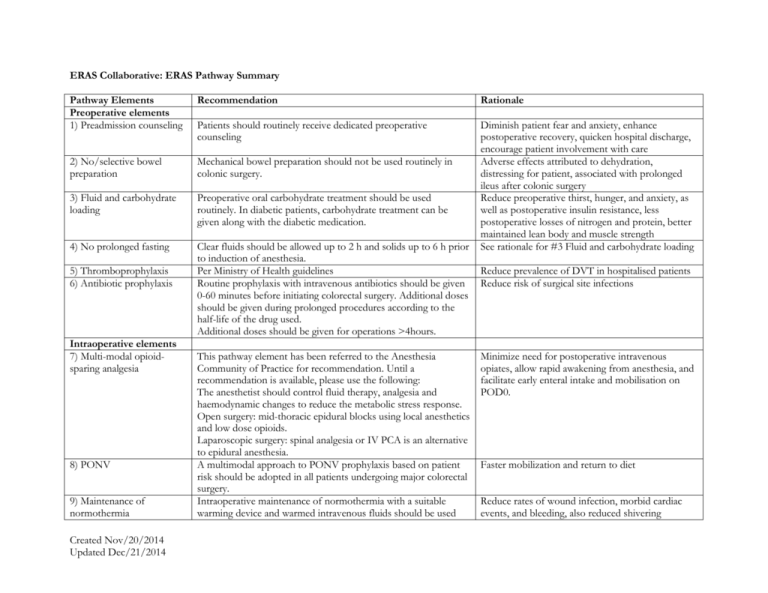
ERAS Collaborative: ERAS Pathway Summary Pathway Elements Preoperative elements 1) Preadmission counseling Recommendation Rationale Patients should routinely receive dedicated preoperative counseling 2) No/selective bowel preparation Mechanical bowel preparation should not be used routinely in colonic surgery. 3) Fluid and carbohydrate loading Preoperative oral carbohydrate treatment should be used routinely. In diabetic patients, carbohydrate treatment can be given along with the diabetic medication. 4) No prolonged fasting Clear fluids should be allowed up to 2 h and solids up to 6 h prior to induction of anesthesia. Per Ministry of Health guidelines Routine prophylaxis with intravenous antibiotics should be given 0-60 minutes before initiating colorectal surgery. Additional doses should be given during prolonged procedures according to the half-life of the drug used. Additional doses should be given for operations >4hours. Diminish patient fear and anxiety, enhance postoperative recovery, quicken hospital discharge, encourage patient involvement with care Adverse effects attributed to dehydration, distressing for patient, associated with prolonged ileus after colonic surgery Reduce preoperative thirst, hunger, and anxiety, as well as postoperative insulin resistance, less postoperative losses of nitrogen and protein, better maintained lean body and muscle strength See rationale for #3 Fluid and carbohydrate loading 5) Thromboprophylaxis 6) Antibiotic prophylaxis Intraoperative elements 7) Multi-modal opioidsparing analgesia 8) PONV 9) Maintenance of normothermia Created Nov/20/2014 Updated Dec/21/2014 This pathway element has been referred to the Anesthesia Community of Practice for recommendation. Until a recommendation is available, please use the following: The anesthetist should control fluid therapy, analgesia and haemodynamic changes to reduce the metabolic stress response. Open surgery: mid-thoracic epidural blocks using local anesthetics and low dose opioids. Laparoscopic surgery: spinal analgesia or IV PCA is an alternative to epidural anesthesia. A multimodal approach to PONV prophylaxis based on patient risk should be adopted in all patients undergoing major colorectal surgery. Intraoperative maintenance of normothermia with a suitable warming device and warmed intravenous fluids should be used Reduce prevalence of DVT in hospitalised patients Reduce risk of surgical site infections Minimize need for postoperative intravenous opiates, allow rapid awakening from anesthesia, and facilitate early enteral intake and mobilisation on POD0. Faster mobilization and return to diet Reduce rates of wound infection, morbid cardiac events, and bleeding, also reduced shivering routinely to keep body temperature 36-38ºC. 10) Avoid salt and water overload 11) No drains Post-operative elements in PAR 12) Chewing gum 13) Urinary drainage 14) Early oral nutrition 15) Early mobilisation 16) Nasogastric intubation 17) Audit (This temperature range is consistent with Canadian Patient Safety Initiative Safer Healthcare Now! guidelines.) This pathway element has been referred to the Anesthesia Community of Practice for recommendation. Until a recommendation is available, please use the following: Patients should receive intraoperative fluids (colloids and crystalloids) guided by flow measurements to optimise cardiac output. (increases oxygen consumption at a critical time) and pain in hypothermic patients. Fewer complications caused by fluid overload Routine drainage is discouraged because it is an unsupported intervention that probably impairs mobilisation. Faster independent mobilisation Chewing gum started in PAR Removal of catheter by POD2 Postoperative patients should be encouraged to take a full fluid diet in POD0-1 and diet as tolerated by POD2. Patient ambulated for any length of time in POD0-1. Patient ambulated for any length of time at least two times in POD2. Prevention of post-operative ileus Prevent urinary tract infections Reduce risk of infection and LOS Postoperative nasogastric tubes should not be used routinely. Nasogastric tubes inserted during surgery should be removed before reversal of anesthesia. For the Collaborative, collect approved minimum data set for 100% of elective colorectal cases. Reduce rate of fever, atelectasis, and pneumonia Early return of gut function Prolonged immobilisation increases the risk of pneumonia, insulin resistance, and muscle weakness. A systematic audit is essential to determine clinical outcome and measure compliance to establish successful implementation of the care protocol. Recommendations are based on clinical experience of implementing ERAS in BC sites and evidence found in the literature (primarily, Gustafson et al. “Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations.” World J Surg (2013) 37:259-284. Created Nov/20/2014 Updated Dec/21/2014