CAAS Standards
advertisement

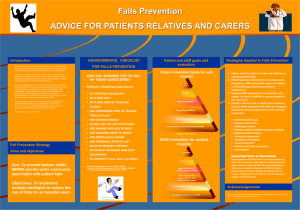
Care Assurance & Accreditation Standards for Acute and GP Hospitals 2015 1 Contents Introduction to Care Assurance & Accreditation Standards (CAAS) .................................................................................................................................... 3 Record of completion: .......................................................................................................................................................................................................... 5 Standard 1: Pressure Area Care .......................................................................................................................................................................................... 6 Standard 2: Falls .................................................................................................................................................................................................................. 8 Standard 3: Catheter Associated Urinary Tract Infection (including continence issues) ..................................................................................................... 10 Standard 4: Deteriorating Patient ....................................................................................................................................................................................... 12 Standard 5: Medicines Management .................................................................................................................................................................................. 14 Standard 6: Pain Control.................................................................................................................................................................................................... 16 Standard 7: Infection Prevention and Control ..................................................................................................................................................................... 18 Standard 8: Food Fluid & Nutritional Care.......................................................................................................................................................................... 20 Standard 9: Person Centred Health and Care .................................................................................................................................................................... 22 Standard 10: Older People in Acute Care & Adult Protection ............................................................................................................................................. 24 Standard 11: End of Life Care: ........................................................................................................................................................................................... 27 Standard 12: Effective Management of Resources & Staff Governance............................................................................................................................. 30 Standard 13: Working Effectively in the Multidisciplinary Team .......................................................................................................................................... 32 2 Introduction to Care Assurance & Accreditation Standards (CAAS) Delivering safe, effective, quality care to patients is at the heart of our business in healthcare. In being responsible and accountable for the quality of safe, effective and person centred care delivered to patient that care should be evidence based and appropriate to the needs of each individual 1. However measuring and assuring the quality and standard of nursing care delivered by individuals and teams is not easy. There is currently no formal system in place that enables us to consistently ensure and assure safe/effective and person centred care at ward/department/team level. To address this there is a professional desire to develop and implement a “Care Assurance and Accreditation System” This system is based on a model used within Salford Royal NHS Foundation Trust and each standard has been framed using the four domains within the Leading Better Care Role Framework (2008). Safe and effective patient care: Leading, managing and developing the performance of the team: Enhancing the patients experience of care: Contributing to the organisations objectives Whilst the CAAS aims to frame the standards using LBC it is also designed to encompass professional standards as well as the key components of the following national and professional drivers: NMC Code and Revalidation Scottish Patient Safety Programme, Person Centred Health and Care Collaborative, Older People in Acute Hospital Care Settings, Healthcare Environment Inspection and Healthcare Associated Infection The Care Assurance and Accreditation System (CAAS) is designed to support nurses and the multiprofessional team in practice to understand how they deliver care, identify what works well and where further improvements are needed. The overall responsibility and accountability for achieving and maintaining the required standards lies with the Senior Charge Nurse (SCN) and the wider team. The role of the senior professional nursing staff, (ie senior nurses, lead nurses or clinical nurse managers) and other specialist services (Practice Development, Quality Improvement support, Organisational Development etc) is to support the SCN and the team to ensure continuous improvement within their departments. 1 Scottish Government (2010) The Healthcare Quality Strategy for NHS Scotland. Available from www.scotland.gov.uk Accessed on 20.10.14 3 Assessment Process – being tested at present Further information on the Assessment Process can be found in the Assessment Framework Document 1. The CAAS lead will select a day to assess the ward, this will be unannounced. 2. The care assessment will cover the identified standards and will involve at a minimum, one third of patients and two thirds of staff. Observation of care given and patients documentation Discussion with patients and staff member 3. Each ward will have an assessment completed and will be accredited with a level 0 to 3. Reassessment will take place at a time interval dependent upon the results: BRONZE SILVER GOLD PLATINUM 5 bronze standards or more in total 3 - 4 bronze standards in total 1- 2 bronze standards in total 3 consecutive gold WAAS assessments PLATINUM competencies PLATINUM Panel PLATINUM Review Panels on a yearly basis Level 0 Level 1 Level 2 Level 3 Reassess in 2 months Reassess in 4 months Reassess in 8 months Reassess in 12 months 4 Care Assurance and Accreditation System 2014 Record of completion: Date: Ward and Specialty: Senior Charge Nurse: Lead Nurse Assessor: Senior Nurse / Head of Nursing: Service Manager: Associate Director of Nursing / Chief of Nursing Services: Overall Score Bronze Silver Gold PLATINUM Ward Level 0 Level 1 Level 2 Level 3 Date action plan due: 5 Standard 1: Pressure Area Care Patient harm from pressure ulcers is prevented 1.1 1.1.1 1.1.2 1.1.3 1.1.4 1.1.5 1.2 1.2.1 1.2.2 1.2.3 1.3 1.3.1 Element: Safe and effective patient care All patients are reliably risk assessed using an agreed tool and there is evidence of ongoing assessment SSKIN care bundle is reliably implemented for patients with an identified risk All patients with pressure area damage or those at high risk have an appropriate plan of care recorded and if grade 2-4 ulcer, a wound care plan in place Pressure relieving equipment is used appropriately for individual patients needs as per local guidance Patients who are identified as being at risk and those who have a diagnosed pressure ulcer are highlighted at ward handovers/ safety briefs / huddles Element: Enhancing the patients’ experience of care Evidence of patients and carers/relatives being encouraged to actively participate in pressure area care by maximising mobility Patient/relatives and carers are fully informed of any pressure damage that occurs Patients and where appropriate carers/relatives understand the plan of care and the importance of good nutrition and hydration and the need to relieve pressure areas regularly Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness Evidence Type Care record, recognised risk assessment tool Care record, SSKIN completion, intentional safety rounds/active care rounds Observation, wound care plan, SSKIN bundle, datix, TVN involvement Observation, discuss with staff, local guidance Compliant Comments OPAH Outcome 8/ SPSP OPAH Outcome 8/ SPSP OPAH Outcome 8/ SPSP Observe, discuss with staff Evidence Type SPSP Compliant Comments Care plan, patient/carers leaflets, discuss with patient/ relatives/carers Care record, discuss with patient/relatives/carers Information leaflets, discuss with patient/relatives/carers, care record. Evidence Type Folder, link nurse descriptor monitored, discuss with SCN . discuss with link nurse PU improvement plan in place, days between PU Mapped to OPAH Outcome 8 / SPSP Mapped to OPAH Outcome 8/ SPSP / PCHC OPAH Outcome 8/ SPSP / PCHC OPAH Outcome 8/ SPSP / PCHC Compliant Comments Mapped to OPAH Outcome 8/ SPSP / VoL 6 1.3.2 Staff have undertaken education and development relating to pressure ulcer risk assessment, prevention and management including the SSKIN bundle Learning plans, training records, discuss with link nurse/SCN OPAH Outcome 8/ SPSP 1.3.3 Staff are aware of how to access specialist pressure relieving equipment both in and out of hours Element: Contributing to the organisations objectives Mattress is checked for signs of damage in line with organisational policy. Patients who have a pressure ulcer are reported in line with organisational policy / guidance including discussion with family / carer Monthly pressure ulcer information is displayed on the ward performance board Discuss with staff OPAH Outcome 8/ SPSP Mapped to Equipment / stock is available to support the prevention and treatment of pressure ulcers Scores Observe, discuss with SCN, stock records 1.4 1.4.1 1.4.2 1.4.3 1.4.4 Evidence Type Compliant Comments Mattress audits OPAH Outcome 8/ SPSP / HEI Datix Lanqip, safety cross, ward displays OPAH Outcome 8/ SPSP OPAH Outcome 8/ SPSP Bronze Silver Gold Best Practice/Comments 7 Standard 2: Falls Patient harm from falls is prevented 2.1 2.1.1 2.1.2 2.1.3 2.1.4 2.1.5 2.1.6 2.2 2.2.1 2.2.2 2.2.3 2.2.4 Element: Safe and effective patient care All patients being reliably risk assessed for falls and evidence of ongoing falls risk assessment All elements of the falls safe care bundle is reliably implemented for patients with an identified risk of falling (i.e. blood pressure, footwear, mobility aids, glasses, medication review etc) Bed rail risk assessment is completed to minimise risk of harm and plan of intervention recorded Patients who have fallen or who have a high risk of falls have a recorded plan of care in line with the level of risk Patients who are identified as high risk of falling and / or who have had a fall are identified at the ward safety brief/huddle and actions taken to minimise risk in line with organisational policies Following a patient fall actions are taken to examine and minimise the risk of further falls, lessons learned are shared across the team Element: Enhancing the patients’ experience of care Patient, relatives/carers are provided with falls prevention information at admission and during stay on ward Patients and relatives /carers are encouraged to actively participate in minimising the risk of falls i.e. appropriate foot wear / glasses sticks etc Patients/relatives/carers are informed, at the earliest opportunity, when a fall occurs, the outcome of the patient falls and actions taken to minimise further risk Patients feel safe and supported and are aware of how to call for assistance when mobilising and alternative systems are in place if patient is unable to use call bell system Evidence Type Care record, falls risk assessment tool Care record, falls safe bundle Compliant Comments Mapped to OPAH Outcome 7 / SPSP OPAH Outcome 7 / SPSP OPAH Outcome 7 / SPSP Care record, audit tools Care record OPAH Outcome 7 / SPSP OPAH Outcome 7 / SPSP Observe, safety briefs, intentional safety rounds/active care rounds, red triangle Debrief, discuss with staff, datix Evidence Type OPAH Outcome 7 / SPSP Compliant Comments Mapped to Discuss with patient/relatives/ carers, information leaflet OPAH Outcome 7 / SPSP / PCHC Discuss with patient/relatives/ carers, observe, care record OPAH Outcome 7 / SPSP / PCHC Care record, discuss with patient/relatives/carers OPAH Outcome 7 / PCHC Discuss with patient/relatives/ carers, observe, falls audit tool OPAH Outcome 7 / SPSP / PCHC 8 2.3 Element :Leading, managing and developing the performance of the team Evidence Type 2.3.1 . The link nurse ensures that staff are up to date with their knowledge and practice, and there is evidence of their effectiveness. OPAH Outcome 7 / SPSP 2.3.2 Staff have undergone education and development in relation to falls risk assessment and falls risk minimisation Learning plans, discuss with staff, discuss with SCN/ link nurse, review falls data/ falls improvement plan Learning plan, training record, discuss with staff 2.3.3 Staff are aware of how to contact specialist support and advice in relation to falls (falls coordinator / physio / podiatry / moving & handling coordinator etc) in line with organisational policy Element: Contributing to the organisations objectives Monthly falls information is displayed on the ward performance board Patients who have a fall are reported in line with organisational policy / guidance including discussion with relatives/carers Scores Discuss with staff , review referrals to specialist services, discuss with specialist services OPAH Outcome 7 / SPSP 2.4 2.4.1 2.4.2 Evidence Type Ward poster, safety cross, lanqip Datix, care record Compliant Comments Mapped to OPAH Outcome 7 / SPSP Compliant Comments Mapped to OPAH Outcome 7 / SPSP OPAH Outcome 7 / SPSP Bronze Silver Gold Best Practice/Comments 9 Standard 3: Catheter Associated Urinary Tract Infection (including continence issues) Patient harm from catheter associated urinary tract infection is prevented. 3.1 3.1.1 3.1.2 3.1.3 3.1.4 3.1.5 3.1.6 3.2 3.2.1 3.2.2 3.2.3 3.2.4 Element: Safe and effective patient care All patients are reliably risk assessed with reference to CAUTI Rationale for insertion of a urinary catheter is documented as well as date, time, type, size, batch number, amount of water in the catheter balloon for patients where catheterisation is required The catheter insertion bundle is reliably implemented for patients who require catheterisation The catheter maintenance bundle is reliably implemented for patients who have a catheter inserted Accurate fluid balance recording is in place for patients with indwelling urinary catheters in line with organisational policy / guidance Patients with an indwelling urinary catheter or who have been identified as having continence issues are highlighted at ward handovers / safety briefs / huddles /intentional rounds Element: Enhancing the patients’ experience of care Patients and where appropriate relatives / carers are actively encouraged to be involved in their care planning and continence management Patients are fully assisted to use toilet facilities and continence aids / devices to reduce the need for an indwelling urinary catheter Patients with an indwelling urinary catheter are encourage to maintain oral fluid intake in line with organisational policy / guidance Patients/relatives/carers are notified at the earliest opportunity when a CAUTI suspected and diagnosed Evidence Type Compliant Comments Mapped to SPSP Care record Care record SPSP Care record SPSP Care record, specimens, lab results Care record, fluid balance chart SPSP Observe, handovers, intentional safety rounds/active care rounds SPSP Evidence Type SPSP Compliant Comments Mapped to Care records, discuss with patient/relatives/carers SPSP / PCHC Observe, discuss with patient/relatives/carers SPSP / PCHC Patient information leaflet, discuss with patient/relatives/carers Care record, discuss with patient/relatives/carers SPSP/ PCHC PCHC 10 3.3 3.3.1 3.3.2 3.3.3 3.4 3.4.1 3.4.2 3.4.3 Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice, and there is evidence of their effectiveness. Staff have undergone education and development in relation to continence management, catheter insertion and indwelling catheter care. Staff are aware of how to access specialist services in relation for continence support and advice Element: Contributing to the organisations objectives Monthly CAUTI information is displayed on the ward performance board Antimicrobial prescribing policy is followed in relation to urinary catheter management and information displayed There is effective and efficient use of resources to support both continence management and catheter care within the clinical area ( e.g. stock rotation, number and size of continence devices etc) Scores Evidence Type Compliant Comments Mapped to Learning plans, CAUTI improvement plan, discuss with SCN / link nurse, training records Learning plan SPSP Discuss with staff SPSP Evidence Type Ward information board, lanqip, safety cross Prescribing information, discuss with staff Observe, review stock, discuss top up with staff, discuss with ward staff SPSP Compliant Comments Mapped to SPSP SPSP / Antimicrobial Stewardship SPSP Bronze Silver Gold Best Practice/Comments 11 Standard 4: Deteriorating Patient Patient harm from unidentified deterioration, sepsis, and cardiac arrest is prevented. 4.1 4.1.1 4.1.2 4.1.3 4.1.4 4.1.5 4.1.6 4.2 4.2.1 4.2.2 4.2.3 Element: Safe and effective patient care Patients observations are reliably recorded at the correct frequency and appropriate actions taken, using the correct equipment Staff identify patients who are deteriorating respond effectively and record the plan of care Emergency medical equipment is available and is checked daily . Sepsis 6 trolleys are cleaned and stock maintained, reviewed and restocked after patient use (where in use) Where appropriate, DNACPR / Ceilings of Treatment /Treatment Escalation Plans should be considered, recorded including evidence of discussion with patients / relatives / carers. This should be reviewed if patient status changes Patients who are identified as high risk / deteriorating / have sepsis are identified at the ward safety brief / huddle and actions taken to minimise risk in line with organisational policies Element: Enhancing the patients’ experience of care When appropriate, patient who are identified of at risk and their relatives /carers , have explained to them what the plan of care and outcomes are in a supportive and sensitive manner Patients/relative/carers feel listened to and are as involved as possible in the decisions regarding their care (consideration of Daily Goals/ ACP / Ceilings of Treatment taken into account) Patients know what to expect and understand the need and frequency of clinical observations to be undertaken Evidence Type Care record, MEWS chart, audit data Compliant Comments Care record, discuss with staff Mapped to SPSP / SIGN guideline 139 Observe, audit, trolley checklist SPSP /SIGN guideline 139 SPSP Observe, checklist, audit SPSP Care record SPSP / PCHC / OPAH Outcome 2 / SIGN guideline 139 Observe, safety brief, care record, intentional safety rounds/active care rounds SPSP/ SIGN guideline 139 Evidence Type Discuss with staff / patient / relatives/ carer Care record, discuss with patient/relatives/carers Discuss with patient/ relatives/carers Compliant Comments Mapped to SPSP / PCHC / OPAH Outcome 2/ SIGN guideline 139 SPSP / PCHC/ OPAH Outcome 2/ SIGN guideline 139 SPSP / PCHC/ SIGN guideline 139 12 4.2.4 Patients/relatives/carers are fully informed about any deterioration in the patient’s condition at the earliest opportunity Discuss with patient/relatives/ carers 4.3 Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice and there is evidence of their effectiveness Staff have access to equipment to monitor the patients condition and can use it appropriately and correctly Staff have undertaken education and development in relation to the recognition of the deteriorating patient / sick patient (including sepsis where appropriate) Evidence Type 4.3.1 4.3.2 4.3.3 4.3.4 4.3.5 4.4 4.4.1 4.4.2 4.4.3 Staff are aware of how to contact specialist support and advice in line with organisational policy (i.e. HECT / ERT/Dual Response etc) Staff are up to date with Basic Life Support and if required Intermediate or Advanced Life Support Element: Contributing to the organisations objectives Cardiac arrest, sepsis and deteriorating patient information is displayed on the ward performance board Staff are aware of organisational policy in relation to the deteriorating patient and escalation of treatment Where there has been a cardiac arrest event or unidentified deterioration of a patient a case note review is completed and lessons learned shared Scores Compliant Comments SPSP / PCHC/ OPAHOutcome 2/ SIGN guideline 139 Mapped to Learning plans, improvement plan, discuss with SCN / link nurse, training records Observe, discuss with staff, training records Training records, discuss with staff/ link nurse / HECT / dual response Discuss with staff / HECT / dual response SIGN guideline 139 Training records, discuss with link nurse / RTOs/ staff Evidence Type SPSP / SIGN guideline 139 Mapped to SPSP/ SIGN guideline 139 SPSP/ SIGN guideline 139 SPSP/ SIGN Guideline 139 Compliant Comments Observe SPSP Discuss with staff, debriefs SPSP / SIGN Guideline 139 SPSP Discuss with staff, cardiac arrest debriefs, discuss with RTO Bronze Silver Gold Best Practice/Comments 13 Standard 5: Medicines Management Patients medicines are stored and administered accurately and safely 5.1 5.1.1 5.1.2 5.1.3 Element: Safe and effective patient care All medicines, including IV infusions, are stored in accordance with organisational policy e.g. PODs, locked trolley / cupboards, locked fridges, IV preparation areas Patient’s weight and allergy status are recorded on the medicine prescription chart, all patients have an accurately completed wristband in situ Medicines reconciliation has been completed on admission to hospital and transfer / discharge Evidence Type Observe Prescription chart, transfer summary, discharge summary, care record Prescription chart Medicine prescription charts and discharge prescriptions are legible and accurate 5.1.5 All medicines are administered in line with organisational policy and best practice Observe drug round, audit of prescription charts 5.1.6 Patients with no medicines reconciliation completed or requiring high risk medicines are highlighted at safety briefs / handovers Element: Enhancing the patients’ experience of care Measures are taken to minimise interruptions during the medicines administration process Review safety brief, review documentation, ask staff Patients/relatives/carers understand the medicines being administered , reason for administration and implications If medicines are omitted this is recorded accurately, including the reason for omission, and action is taken Ask patient/relatives/carers Medicines reconciliation on admission has taken place which involves the patient / relatives and or carers Review notes, ask patient/relatives/carers 5.2.1 5.2.2 5.2.3 5.2.4 Comments Care record, prescription chart, observe patients 5.1.4 5.2 Compliant Evidence Type Coloured tabards, quiet zones observe Review prescription charts Compliant Comments Mapped to NMC standards medicines management NMC standards medicines management NMC standards medicines management NMC standards medicines management NMC standards medicines management NMC standards medicines management Mapped to NMC standards medicines management NMC standards medicines management NMC standards medicines management NMC standards medicines management 14 5.2.5 Where patients require medicines for their discharge home / transfer these have been explained to p/r/c and to another care setting this is undertaken to minimise delays Element: Leading, managing and developing the performance of the team The link nurse/person ensures that staff are up to date with their knowledge and practice and there is evidence of their effectiveness Staff have access to key sources of medicines information whilst on the ward and know how to access them e.g..eBNF, BNF , drug data sheets, IV monographs, clinical guideline Staff receive appropriate training relating to medicines administration Care record, observe, discharge summary Staff can access pharmacy support in relation to medicines queries and administration. Where IV drugs require administration staff are appropriately trained, assessed and competent and keep their skills up to date Element: Contributing to the organisations objectives Controlled drugs are stored, administered and checked in line with legal and organisational requirements Ask staff, discuss with pharmacy 5.4.2 All medication incidents are recorded and there is evidence of appropriate learning shared Datix 5.4.3 There is effective and efficient management of medicines stock levels and spending, with evidence of review processes Scores Review pharmacy order, observe drug cupboards/trolleys 5.3 5.3.1 5.3.2 5.3.3 5.3.4 5.3.5 5.4 5.4.1 Evidence Type NMC standards medicines management Compliant Comments Mapped to Review training records, speak to link nurse/SCN Ask staff, observe medicines management NMC standards medicines management Review training records/PGD/ CPD NMC standards medicines management NMC standards medicines NMC standards medicines management Mapped to Review training records, ask staff Evidence Type Review controlled drug book Compliant Comments NMC standards medicines management / Dangerous Drug Act NMC standards medicines management NMC standards medicines management Bronze Silver Gold Best Practice/Comments 15 Standard 6: Pain control Patients’ pain will be controlled to an acceptable level 6.1 6.1.1 6.1.2 6.1.3 6.2 6.2.1 6.2.2 6.3 6.3.1 6.3.2 6.3.3 Element: Safe and effective patient care All patients have a pain assessment using a recognised pain tool recorded on admission and reassessment appropriate to patient status and severity of pain Analgesia is prescribed and administered in line with patients severity of pain and organisational protocol and are monitored for effectiveness Patients who have high risk pain control therapy (such as PCA , epidural, syringe driver) are highlighted at safety briefs / handovers Element: Enhancing the patients’ experience of care Pain relieving measures are taken promptly and the effectiveness of the intervention to alleviate pain reviewed. This may include comfort measures, distraction therapy etc Patients and where appropriate carers / relatives are encouraged to actively participate in pain management Element: Leading, managing and developing the performance of the team The pain control link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness Device managers ensure that staff are able and competent to use appropriate devices to administer pain relief. Staff are aware of how to contact specialist service relating to effective pain management Evidence Type Review case notes Compliant Comments Review case notes/ pain charts Observe safety brief, ask staff Evidence Type Compliant Comments Mapped to SIGN guidance 136 SIGN guidance 106 OPAH Outcome 1 SIGN guidance 136 SIGN guidance 106 OPAH Outcome 1 SIGN guidance 136 SIGN guidance 106 OPAH Outcome 1 Mapped to Review case notes/ pain chart, ask patient/relatives/carers SIGN guidance 136 SIGN guidance 106 Patient information leaflets SIGN guidance 136 SIGN guidance 106 Evidence Type Compliant Comments Mapped to Review training records, discuss with link nurse / SCN SIGN guidance 136 SIGN guidance 106 Review training records SIGN guidance 136 SIGN guidance 106 Ask staff , discuss with specialist pain services SIGN guidance 136 SIGN guidance 106 16 6.4 6.4.1 Element: Contributing to the organisations objectives Pain control and pain management guidelines are available and reliably implemented , including palliative care protocols, pain management for patients with dementia 6.4.2 Devices are available, maintained and serviced in line with agreed organisational processes. Scores 1 ‘no’ in each element / 50% ‘no’ / 7 no’s 2 ‘no’s / less than 50% in total and the rest ‘yes’ 1 ‘no’ in total and the rest ‘ yes’ / 100% ‘yes’ Best Practice/Comments Evidence Type Compliant Comments Mapped to Review availability, ask staff SIGN guidance 136 SIGN guidance 106 Ask staff, review any devices available re maintenance check SIGN guidance 136 SIGN guidance 106 Bronze Silver Gold 17 Standard 7: Infection Prevention and Control Patients receive care in a clean environment, where risks of Healthcare Acquired Infection are minimised 7.1 Element: Safe and effective patient care Evidence Type Compliant 7.1.1 Hand washing facilities or alcohol based hand rubs SICPs audits, ward displays, are available at the ward entrances and at point of ask visitors, observe care delivery and staff / visitors encouraged to use them 7.1.2 The decontamination of commonly used equipment SICPs audits, observe, review i.e. commodes, I.V. stands, mattresses , bed spaces cleaning records is carried out in accordance with Standard Infection Control Procedures (SICPs) and are labelled appropriately. Records of regular cleaning are maintained 7.1.3 All staff clean their hands appropriately in line with the SICPs audits 5 key moments for hand hygiene and the six steps. 7.1.4 Personal Protective Equipment (PPE) is worn in line SICPs audits with SICPs and is removed between patients and if necessary between care delivery interventions with the same patient and hands cleaned. 7.1.5 Patients with a suspected or known infection are SICPs audits isolated and cared for in line with Transmission Based Precautions 7.1.6 The peripheral vascular catheter / central vascular SICPs audits catheter insertion and maintenance bundle is reliably implemented for patients 7.1.7 Environmental Infection Control audit is completed SICPs audits every 6 months 7.2 Element: Enhancing the patients’ experience of Evidence Type Compliant care 7.2.1 Patients and carers / relatives are encouraged to Observe, ask patients/relatives actively participate in assisting in reducing the risks of HAI 7.2.2 Patients who require to be isolated feel safe and are Ask patients/relatives/carers, understand what is happening and how to get observe, discuss with staff assistance if required Visitors are aware of their role in preventing further infection Comments Mapped to SICPS HEI SICPS HEI SICPS/ HEI SICPs /HEI SICPs / HEI SICPs / HEI SICPs /HEI Comments Mapped to 18 7.2.3 7.2.4 7.3 7.3.1 7.3.2 7.3.3 7.3.4 7.4 7.4.1 7.4.2 7.4.3 7.4.5 Patients who require isolation are risk assessed to ensure other care needs are not compromised i.e risk of falls, dementia, wellbeing Patients/relatives/carers are informed, at the earliest opportunity, there are any suspected or actual infection control issues at the earliest opportunity Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness All staff have completed and are up to date with compulsory infection control learning modules Staff know how to access and follow organisational policies in relation to infection control issues i.e outbreak management, escalation procedures, sickness absence management Staff are aware of how to contact specialist support relating to infection prevention and control issues Element: Contributing to the organisations objectives The ward environment is clean, clutter free and in a good state of repair and ward cleaning schedules are available and monitored Linen is appropriately bagged and tagged in line with SICPs and organisational policy Safe disposal of waste is undertaken in line with organisational policy Performance information relating to HAI (MRSA / CDiff,SAB) is displayed in a meaningful way for both patients and staff Scores Review case notes, discuss with staff HAI standards Review case notes, ask patient/relatives/carers Evidence Type Compliant Comments Mapped to Discuss with link nurse/ SCN, review folder HAI standards Review training records HAI standards Ask staff, discuss with infection prevention and control team HAI standards SICPS Ask staff, discuss with infection prevention and control team Evidence Type SICPs Compliant Comments Mapped to Observation Observation, ask staff Observation, ask staff Observation Bronze Silver Gold Best Practice/Comments 19 Standard 8: Food Fluid & Nutritional care Patients experience of eating and drinking enhances their health and well being 8.1 Element: Safe and effective patient care Evidence Type 8.1.1 Patients nutritional status has been reliably assessed Review case notes using a recognised screening tool and plan of care clearly recorded A clear process for identifying individual patient’s nutritional requirements and support is in place (e.g. white board, safety brief.) 8.1.3 Patients have the opportunity to clean their hands before mealtimes 8.1.4 Patients are offered fresh, cold water at regular intervals and encouraged to maintain oral intake as appropriate. 8.1.5 Where required patients are positioned to allow them to eat safely 8.1.6 Staff clearly identify patients who are fasting or NBM and follow organisational guidelines for their management 8.1.7 Staff clearly identify patients who require enteral or parenteral feeding and follow organisational guidelines for their management 8.1.8 All food and fluid charts are completed and monitored regularly 8.1.9 Appropriate and timely referrals are made for patients identified as being in need of specialist nutritional support 8.1.10 Patients with swallowing difficulties are offered the correct texture of food and fluids after assessment 8.2 Element: Enhancing the patients’ experience of care 8.2.1 Patients who have been identified as requiring support with eating and drinking are given assistance as appropriate, in a dignified manner 8.2.2 Relatives, carers or volunteers are positively encouraged to assist at meal times for appropriate individuals 8.1.2 Compliant Comments Observation of whiteboard /safety brief, ask staff, observe mealtime Observation, ask patients Ask patients, observation Mapped to OPAH Outcome 1,6 FFN Standards (2014) 2.1, 2.2, 2.3, 2.9 OPAH Outcome 6 FFN Standards (2014) 4.1 (a) FFN Standards (2014) 4.8 OPAH Outcome 6 FFN Standards (2014) 4.5 Observation, ask staff Observation, ask staff Review notes, ask staff Review notes FFN Standards (2014) 4.1 (g) Review notes, referral data from specialty services. Review notes, ask staff Evidence Type Compliant Comments FFN Standards 4.11 Mapped to Meal time observation FFN Standards (2014) 4.1 (e), 4.6 Meal time observation, ask patient/relatives PCHC 20 8.2.3 8.2.4 8.3 8.3.1 8.3.2 8.3.4 8.3.5 8.3.6 8.4 8.4.1 Patients are given sufficient time to eat and drink at their own pace Patients are asked about likes and dislikes and this is recorded and acted upon Observation, ask patient Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness All staff have completed and are up to date with the Food Hygiene LearnPro module. A mealtime coordinator is identified every day on the duty rota sheet The number of staff involved is adequate to support all the processes in the Standard Operating Procedure for Mealtimes Staff undertake a meal time sweep Evidence Type Element: Contributing to the organisations objectives All the principles of the Mealtime Bundle/ Protected Mealtimes are embedded within the clinical area Scores Ask patient, observe, review notes Compliant Comments Review link nurse folder if available, training records, discuss with link nurse/SCN Review training records FFN Standards (2014) 4.1.(d) FFN Standards (2014) 2.2 (c) 4.1 (d) Mapped to FFN Standard 6.3 Review duty rota, observe Review rosters, observe Meal time observation, discuss with staff/patient/relatives/carers Evidence Type Observation FFN Standards (2014) 4.6 Compliant Comments Mapped to FFN Standards 4.7 Bronze Silver Gold Best Practice/Comments 21 Standard 9: Person Centred Health and Care Patients experience person centred care and feel safe and supported within the care environment 9.1 9.1.1 9.1.2 9.1.3 9.1.4 9.1.5 9.2 9.2.1 9.2.2 9.2.3 Element: Safe and effective patient care Ward environment is clean, clutter free, calm and noise kept to a minimum, particularly in respect of those patients who experience cognitive impairment Environmental and specific risks are taken into consideration relevant to specific patient needs There is evidence that patients needs are assessed and addressed on an ongoing basis Staff are able to access support for patient’s spiritual needs If patients have been transferred between wards the reason for transfer is clearly documented and is clinically appropriate. Element: Enhancing the patients’ experience of care Patients, relatives and carers are orientated to the environment on admission and ongoing. i.e how to call for assistance, where toilets are, mealtimes, visiting times etc Patients, carers and relatives are encouraged to be involved in decisions regarding the patients care and take an active role in contributing to the plan of care Patients are addressed by their preferred name 9.2.4 Patients are asked about “who and what matters most to me..” and this is recorded and acted upon 9.2.5 Patients receive care which is dignified and respectful i.e appropriate use of curtains, sensitivity regarding going to toilet, ensuring patients dignity preserved Corporate feedback tools are clearly visible and accessible for patients and visitors (Care to Comment Card, ‘our customer service – what do you think?) 9.2.6 Evidence Type Observe Compliant Comments Observe, care record, safety brief, discuss with staff Care record, observe OPAH Outcome 1 OPAH Outcome 2,5,9 OPAH Outcome 1,5 Care record, discuss with patient Care record, transfer/handover forms Evidence Type Mapped to Compliant Comments Mapped to Care record, ward information sheet, discuss with patient/ relatives/ carers OPAH Outcome 1 Care record, discuss with patient/relatives/carers OPAH Outcome 2,3,4,9 Observe, care record, discuss with patient Care record, Getting to Know Me document, discuss with patient/relatives/carers Observe, discuss with patient OPAH Outcome 2, 5,9 Observe, discuss with staff PCHC PCHC 22 9.2.7 9.3 9.3.1 9.3.2 9.4 9.4.1 9.4.2 9.4.3 Information leaflets appropriate to the care environment are visible and easily accessible for patients Element: Leading, managing and developing the performance of the team The link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness There is evidence that staff have undertaken some learning and development relating to person centred health and care Element: Contributing to the organisations objectives There is a patient feedback board visible for staff and relatives within the area that is clearly being used All staff are aware of, and have access to, National Care Standards Customer Care / patient experience audits are carried out at the designated intervals and appropriate action plans put in place Scores Observe Evidence Type Compliant Comments Mapped to Compliant Comments Mapped to Review link nurse folder if available, training records, discuss with link nurse/SCN Learning plan, PDP, discuss with staff Evidence Type Observe PCHC Discuss with staff National Care Standards National Care Standards Review of audits and action plans Bronze Silver Gold Best Practice / comments 23 Standard 10: Older People in Acute Care & Adult Protection Ensure older & vulnerable patients’ needs are met in the acute ward setting 10.1 Element: Safe and effective patient care Evidence Type 10.1.1 Ward environment is welcoming, hazard free, with correct signage that is appropriate for patients with cognitive impairment clocks visible in each room, colour scheme 10.1.2 Glasses, hearing aids, and dentures are accessible to patients Walking aids are for individual patients and kept within reach 10.1.3 Patient has been fully assessed for cognitive impairment, ensuring that where there is cognitive impairment, delirium is excluded. 10.1.4 Where cognitive impairment has been identified, correct care bundles are in place and the correct identifiers used. Where delirium has been identified the TIME bundle is in place 10.1.5 Where cognitive impairment is identified an assessment of capacity is undertaken within the AWI legal framework 10.1.6 Staff are aware of how to access specialist help and advice from Mental Health/Elderly Mental Health/Learning Disability Team/Social Work 10.1.7 All patients assessed as having capacity issues have an Adults with Incapacity Certificate and Treatment Plan in place 10.1.8 All patients who have Power of Attorney have it clearly identified in notes and copy of documentation requested and retained 10.1.9 Stress/ distress managed in ward using Newcastle Model ( recommended by NES) with as required medication closely monitored and reviewed 10.1.10 Appropriate assessment of pain using tool suitable based on need ( Abbey pain tool if unable to verbally communicate pain) Compliant Comments Mapped to Observation OPAH Commitment 10 Observation, review case notes OPAH Commitment 10 Review case notes OPAH 11.1, 11.2, 13.1, Commitment 10 Commitment 10 OPAH 12.1, 12.3 Delirium Guidelines. OPAH 2.1, 2.3, 2.4, 12.6 Review case notes Medical notes, AWI treatment plan, record of carer involvement Audit, evidence of referrals With specialist services, ask staff OPAH Commitment 10 Review notes OPAH Commitment 10 Review notes OPAH Commitment 10 Drug kardex prescription audits, review record for impact of medication used Review notes OPAH Commitment 10 OPAH Commitment 10 24 Element: Enhancing the Patient’s experience of care Full assessment of patient needs is completed on admission to the ward. 10.2.2 All patients with cognitive impairment have a completed Getting To Know Me document completed Evidence Type Review notes 10.2.3 Review notes 10.2 10.2.1 10.2.4 10.2.5 10.2.6 10.3 10.3.1 10.3.2 Accurate next of kin details are recorded at admission, including details of legal guardianship/power of welfare attorney Staff respond appropriately and timeously to requests for support with attending to basic hygiene and toilet needs All care is carried out in a discreet and respectful manner There is evidence that the patient and relatives / carers participate in care and decision making Element: Leading, managing and developing the performance of the team Audit of physical environment is carried out using the dementia environment checklist All staff have access to training in caring for patients with cognitive impairment: Comments Review notes Mapped to OPAH 6.6, 9.6 Commitment 10 OPAH 3.1, 3.2,Commitment 10 OPAH Commitment 10 Observation OPAH Commitment 10 Observation OPAH Commitment 10 OPAH Commitment 10 Mapped to Review case notes, discuss with relatives/carers Evidence Type Observation, audit results Review training records Compliant Comments OPAH Commitment 10 OPAH Commitment 10 Informed/ skilled level Promoting Excellence NES Delirium module Stress/ Distress training NES Think Capacity OPAC/Dementia link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness 10.3.4 Guidelines are in place to support staff to maintain patient safety with regard to risk assessment and increased supervision of patients at risk 10.3.5 The ward has an identified Carers Champion/s and Staff are aware of how to access the carers liaison service and the advocacy service 10.3.3 Compliant Review link nurse folder if available, training records, discuss with link nurse/SCN Ask staff, review records OPAH Commitment 10 Ask staff Commitment 10 OPAH OPAH Commitment 10 25 10.4 Element: Contributing to the organisations objectives 10.4.1 Standards of care are measured on a regular basis to ensure compliance with care bundles and organisational values Scores Evidence Type Audits, complaints, patient feedback Compliant Comments Mapped to OPAH Commitment 10 Bronze Silver Gold Best practice / comments 26 Standard 11: End of Life Care: Patients and their families / carers are supported effectively during End of Life Care 11.1 11.1.1 11.1.2 11.1.3 11.1.4 11.1.5 11.2 11.2.1 11.2.2 11.2.3 11.2.4 Element: Safe and effective patient care Staff are able to identify patients who require End of Life care and plan care appropriately There are clearly documented records of discussions relating to ceilings of treatment and DNACPR with patients and families / cares where appropriate within the clinical / care record Where discussions have identified Preferred Place of Death as home/care home, provide necessary support to expedite transfer Staff initiate and coordinate the rapid discharge of a dying patient from hospital to home, if requested and involve the discharge coordinator for assistance and support Staff are aware of and know how to seek advice on areas of care such as nutrition, hydration and pain / sedation management in End of Life care Element: Enhancing the patients’ experience of care Staff are aware of the support available to themselves and their patients, relatives and carers through the spiritual care team Relatives of a dying patient have access appropriate information and facilities i.e. quiet space, refreshments, telephone Information for relatives following a bereavement (i.e ‘What to do After a Death’ or ‘Information and Support for When Someone Dies’ ) and bereavement support is made available Staff are aware of verification of death policy( in care settings without 24hour medical cover) and how death or acute deterioration is communicated to relatives who are present, or via telephone Evidence Type Review case notes, ask staff Compliant Comments Review case notes Mapped to OPAH Outcome 3, OPAH Outcome 4 OPAH Outcome 3, OPAH Outcome 4 Review case notes, ask staff OPAH Outcome 4 Ask staff re process, review records OPAH Outcome 4 Ask staff, review records OPAH Outcome 3, OPAH Outcome 4 Evidence Type Compliant Comments Mapped to Ask staff, review information available on ward OPAH Outcome 4 Observation, ask staff OPAH Outcome 4 Review information available OPAH Outcome 4 Ask staff 27 11.2.5 11.3 11.3.1 11.3.2 11.3.3 11.3.4 11.4 11.4.1 11.4.2 11.4.3 11.4.5 Staff undertake the last offices for the deceased patient in a safe, respectful and dignified manner in line with organisational policies. Element: Managing and developing the performance of the team Staff are trained in end of life care and can demonstrate principles of bereavement care and support for patients, families and carers The palliative care link nurse / bereavement care link nurse ensures that staff are up to date with their knowledge and practice , and there is evidence of their effectiveness Staff can access support in line with organisational structures if required following a personal or patient death (i.e employee counselling, HR, Spiritual Care Team, Staff Care Team, Occupational Health) Human Resources policies are adhered to in relation to staff following a bereavement Element: Contributing to the organisations objectives Staff are aware of the content of organisational policies relating to End of Life and Bereavement care Contact numbers for community support services , care teams , social work, palliative are services etc are readily accessible for staff, patients / carers and families Staff follow organisational protocol relating to death certification, procurator fiscal involvement and are able to communicate this ins a supportive and sensitive manner to bereaved relatives. When a death is unexpected a case note review is undertaken to identify any avoidable harm and, where appropriate lessons learned shared. Scores Ask staff Evidence Type Compliant Comments Mapped to Compliant Comments Mapped to Ask staff Review link nurse folder, staff training records Ask staff, review information available for staff Review rosters Evidence Type Ask staff Review information available Ask staff Review debrief, learning from event plan, discuss with staff Bronze Silver Gold 28 Best Practice/Comments 29 Standard 12: Effective Management of Resources & Staff Governance Ward systems and processes enhance safe, effective and person centred care 12.1 12.1.1 12.1.2 12.1.3 12.1.4 12.1.5 12.2 12.2.1 12.3 12.3.1 12.3.2 Element: Safe and effective patient care Staff rosters comply with organisational policy and national guidance A nurse in charge / shift coordinator is identified on every shift to ensure smooth and efficient care delivery and can be identified Nurse in charge / shift coordinator identifies and escalates any gaps in staffing/ increase in shift workload to ensure appropriate effective patient safety and high standards of person centered care are maintained. Ward processes are designed, implemented and reviewed to ensure the efficient delivery of safe, effective and person centred care Stock levels are maintained appropriately and within agreed budget to deliver safe, effective and person centred care. Element: Enhancing the patients’ experience of care Feedback from a range of sources is used to inform and improve practice including learners and students Element: Leading, Managing and developing the performance of the team Predictable absence and supplementary staffing is monitored and appropriate action taken to ensure compliance with National workforce workload tools and within budget Link nurse / champions within the clinical area have clearly defined roles and responsibilities and there is evidence of their effectiveness Evidence Type Review rosters Compliant Comments Mapped to Evidence Type Compliant Comments Mapped to Practice placement audits, discuss with ward mentors/PEF’s, student feedback, patient feedback/complaints Evidence Type Compliant Comments Mapped to Review rosters/whiteboard Review rosters, review datix in relation to staffing issues Named nurse, audit datix reports and Riddors, review/observe safety brief and patient care, review ward dashboard if in place Observe stock levels/ward, review budgets Review rosters Review link nurse folder 30 12.3.3 Professional registration is monitored and staff are aware of their roles and responsibilities including , revalidation and the application of the NMC Code. 12.3.4 There are appropriately selected, trained and maintained mentors to effectively support learning and assessment within the practice environment All staff have a PDP in place and have PDP reviews documented All staff have undertaken compulsory and mandatory training relevant to organisational policies 12.3.5 12.3.6 12.4 12.4.1 12.4.2 12.4.3 12.4.4 Element: Contributing to the organisations objectives Policies relating to organisational Human Resources are reliably implemented Health and safety legislation and policies are reliably implemented and issues escalated in line with agreed protocols Ward budgets are maintained within agreed levels and the SCN is aware of any financial exceptions Equipment / other resources are available to support safe and effective care delivery Scores Review record of professional practice, audit local process in place for monitoring/reporting, NMC registration, discuss with staff Practice education mentor database, review practice placement audits, training records Review PDP figures (eKSF) Review training records, review managers learnPro reviewer reports Evidence Type OPAH Outcome 10 Compliant Comments Mapped to Discuss with staff/ SCN/LN & HR support managers/ Occupational Health, review staff complaints, promoting attendance records, disciplinary hearings, complaints Review ward datix reports, stress risk assessments Review budgets Observation Bronze Silver Gold Best Practice/Comments 31 Standard 13: Working Effectively in the Multidisciplinary Team Robust and effective communication & documentation enhances safe, effective and person centred care. 13.1 13.1.1 13.1.2 13.1.3 13.1.4 13.1.5 13.1.6 13.1.7 13.2 13.2.1 13.2.2 13.2.3 13.2.4 Element: Safe and effective patient care Patient information boards are clean, up to date and display relevant nursing / medical / AHP information Registered nursing staff take an active role in the ward round and contribute effectively to discussions relating to safe, effective and person centred care, recording the plan of care in the care record. There is evidence of effective multidisciplinary team working which promotes safe, effective and person centred care Staff take an active part in Safety Briefs / Safety Huddles / Whiteboards / meetings at a local / departmental level Patients who are identified at risk are highlighted Intentional Safety Rounding is reliably implemented within the ward area Staff record incidents (actual or near miss) on DATIX, investigations occur and lessons learned are shared There is evidence of action following informal or formal debriefs, examining data for improvement, from patient safety executive walk rounds, inspections , and / or scrutiny visits Element: Enhancing the patients’ experience of care Staff introduce themselves to patients and their visitors in a friendly and professional manner at all times The nurse in charge is known to patients , relatives and carers Patient information leaflets are readily accessible to patients / relatives and carers and staff answer questions if required Patient care is assessed, planned and recorded in line with the nursing process and reviewed and updated Evidence Type Observation Compliant Comments Mapped to Compliant Comments Mapped to Observe, ask staff, review records Case note review, discuss with members of the MDT Ask staff , review attendance, observe Audit patient records, observation Review datix and actions taken As above Evidence Type Observation Ask staff, observation Observation Review case notes 32 13.2.5 13.2.6 13.3 13.3.1 13.3.2 13.3.3 13.3.4 13.3.5 13.3.6 13.4 13.4.1 13.4.2 Staff are available/accessible when relatives /carers visit to discuss the patients well being/progress and care and this is recorded within the care record. Patients / relative and carer feedback is used to inform area for improvement Element: Leading, managing and developing the performance of the team Clinical record keeping complies with legal and professional standards and action taken to improve record keeping standards at a personal / ward level The SCN assures the quality of care within their sphere of responsibility There is evidence of robust communication across the team i.e. handovers, team meetings, team newsletters, team cascade discussions etc Staff identify evidence to support Professional Revalidation There is a clearly identified learning plan within the clinical area All staff new to the clinical area receive relevant role and departmental induction Element: Contributing to the organisations objectives Organisational policy relating to IT systems is adhered to The Health and Safety Control Book is maintained and is up to date and there is evidence of actions taken to minimised identified health and safety issues Scores Review case notes Review feedback and actions Evidence Type Compliant Comments Mapped to PDP/eKSF, ward learning plan, staff training records Review ward learning plan with staff/SCN Local Induction plan, discuss with staff/SCN/LN, review training records Evidence Type Compliant Comments Mapped to Review case notes Quality performance data, regular quality meetings Review minutes from team meetings, staff survey results Review, observe practices Review book Bronze Silver Gold Best Practice/Comments 33