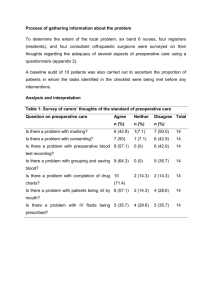
Supplementary data tables Table 1 supplementary: Quality

Supplementary data tables
Table 1 supplementary: Quality assessment checklist used to evaluate studies
Representative sample
Blinding
Baseline comparability
Source description
Was the source of participants adequately described?
Referral pattern
Was the recruitment method adequately described? eg. Representative sample: participants were selected as consecutive or random cases.
Patient characteristics
Was the population of interest adequately described for key characteristics: severity, co-morbidity, inclusion/exclusion criteria, age and sex?
Yes, if all characteristics are reported.
No, if the description is limited to age and sex characteristics, or none.
Sample size
Was the sample size large enough? The rule of thumb: At least 10 cases per independent variable are required at a power of 80% and a 5% significance level (eg. The author runs a comparison for age, sex, symptom duration, pre-/post-operative neurological scores, etc).
Blinded assessor
Were MRI assessors involved in the study blinded to clinical data? eg. Blinded outcome assessment: assessor was unaware of prognostic factors at the time of outcome assessment.
Compared baseline performance of clinical status
Is baseline performance of clinical status measured?
If yes, is the absolute difference between the groups less than 10%?
If yes, score the quality criterion as YES.
If no, did the analysis take into consideration the baseline imbalance (for example, analysis of co-variance or analysis by change scores between groups? eg. Statistical adjustment: multivariate analyses conducted with adjustment for potentially confounding factors.
If yes, score the quality criterion as YES.
If no, score the quality criterion as NO.
Otherwise, if no comparison is completed, then NA
Compared baseline performance of other prognostic variables
Is baseline performance of age, sex and symptom duration measured?
If yes, is the absolute difference between the groups less than 10%?
If yes, score the quality criterion as YES.
If no, did the analysis take into consideration the baseline imbalance (for example, analysis of co-variance or analysis by change scores between groups? eg. Statistical adjustment: multivariate analyses conducted with adjustment for potentially confounding factors.
If yes, score the quality criterion as YES.
If no, score the quality criterion as NO.
Otherwise, if no comparison is completed, then NA
Yes No Comments
Follow-up
Validation of outcome measurement
Validation of prognostic factor measurement
Complete
Was follow up reported?
If yes, was follow-up complete? Follow-up >80%: outcome data were available for at least 80% of participants at one follow-up point.
If not, then score the quality criterion as NO.
Comparison of drop outs with remained
Were those followed up comparable to those who dropped out?
Reasons of drop outs
Were reasons for loss to follow-up provided?
Valid
Were outcome measures adequately valid?
Yes, if the prognostic study tested the validity of measurements used or referred to other studies which had established validity.
Otherwise, no .
Reliable
Were outcome measures adequately reliable?
Yes, if the prognostic study tested the reliability of measurements used or referred to other studies which had established reliability.
Otherwise, no .
Defined
Were definitions or descriptions of MRI prognostic factors adequately provided?
Yes, if there is clear indication of measurement method such as detailed description of MRI protocol including planes (axial/sagittal and thickness of slices).
Otherwise, no .
Reliable
Were prognostic factors measures adequately reliable?
Yes, if inter/intra-observer reliability tests with/without coefficient value are reported (eg. Cronbach alpha or Kappa coefficients).
Otherwise, no.
Tables 2 supplementary: Evidentiary summary of studies on prediction of outcomes after surgery in patients with CSM (FS = Functional Score; RP= Recovery %)
Dark grey – excellent study, Light grey – good study, White – Poor study
Predictor Outcome
FS
Author Results
TA (transverse area)
CR
(compression ratio)
AP
(anteroposterior diameter)
RP
FS
RP
FS
RP
Morio et al 2001 (31 OPLL & 42 CSM patients). Significant association between post-JOA scores and preoperative spinal cord surface (r=0.398, p =
0.0015) was found at follow up (6 months to 10 years, mean follow up of 3.4 years). After adjustment for age, duration of symptoms and preoperative scores, the preoperative surface area of the spinal cord is not associated with the functional score of
CSM patients.
Fukushima et al 1991 (13 OPLL, 29 CSM, 13 CHD patients). Significant association between transverse area and post-operative JOA scores (r=0.298, p <0.05) was found at mean follow up of 17 months (from 6 to 48 months after surgery).
Morio et al 2001 Found mild significant association between recovery percentage and preoperative cross-sectional area of spinal cord (r=0.243, p =
0.0517).
Fukushima et al 1991 Found significant difference in recovery percentage in groups with a spinal cord area of less than 0.45 cm 2 ( p <0.01), reflecting the
Okada et al 1993 irreversible pathology of spinal cord.
(23 OPLL, 34 CSM, 17 CHD patients). Showed an association for each individual etiology group, OPLL (ossification of the posterior longitudinal ligament) (r=0.678, p <0.01) and CSM (cervical spondylotic myelopathy) (r=0.586, p <0.01). After adjusting for disease etiology, duration of symptoms, signal intensity changes, the investigators showed that the preoperative cross-
Shin et al 2010
Chen et al 2001 sectional area of spinal cord is an independent predictor of recovery percentage in CSM patients (no follow up time was reported).
(137 CSM patients). Insignificant association between compression and post-operative JOA scores was found at mean duration of follow-up of 32.7 months ( p =0.595, no r-value reported).
(64 CSM patients). Reported similar findings with a report of insignificant association between preoperative compression ratio and recovery percentage at 6 months follow up after surgery (r=0.026, p =0.836).
Okada et al 1993
Shin et al 2010
Chung et al 2002
Ahn et al 2010
Yone et al 1992
Yone et al 1992
Reported that the recovery percentage was not significantly associated with compression ratio irrespective of etiology (OPLL/,
CSM or CDH (cervical herniated disc)) (follow up period was not reported).
Insignificant association between compression and percentage recovery was found at mean duration of follow-up of 32.7 months ( p and r values were not reported).
(37 CSM/CHD/LF patients involving more than three levels). Showed that compression ratio is associated with recovery percentage calculated from the JOA scores from 24 to 84 months after surgery (mean follow up of 42 months), where patients were divided into two groups according to the recovery percentage – a ‘good’ group ( n
=19), and a ‘fair’ group ( n =18). The results showed that patients in the good group showed a greater compression ratio ( p <0.05).
(39 CSM patients). The spinal cord compression ratio was positively associated with the recovery percentage defined the JOA scale at mean follow-up period of 19.1 months (r=2.54, p =0.00).
(45 OPLL, 64 CSM, 31 healthy patients). No relationship was found between AP diameter and post-operative functional scores
(follow up period was not reported).
The author found significant association between recovery percentage, evaluated by the Hirabayashi’s formula based on the JOA scores, and preoperative minimum AP diameter among OPLL but not CSM patients. Although the authors reported the differences in recovery percentages between two pathologies, no statistical analysis and mean of JOA scores were documented.
Predictor Outcome Author Results
Grades of spinal cord compression
FS
RP
Singh et al 2001
Uchida et al 2005
Matsuyama et al 2004
Nagata et al 1996
Matsuyama et al 2004
Kasai et al 2001
Nagata et al 1996
(69 CSM patients) found no significant association between spinal cord compression and post-operative walking scores obtained at 3 months follow up (r=0.07, p =0.60).
(135 CSM/OPLL patients) retrospectively studied morphological and functional scores assessed by JOA scale obtained from
12 months to 12.8 years (mean follow up of 8.3 years) after surgery. The percentage rate of flattening and canal narrowing were used to estimate the morphological changes of spinal canal and cord on sagittal T1-weighted MRI. The authors reported that the better functional scores of OPLL, but not CSM patients, are associated with the preoperative spinal canal narrowing by ossification of <40% and an extent of cervical cord flattening of ≥50%. The validity of findings is difficult to judge due to poor description of performance (no report of mean, SE, p and r values).
(44 OPLL patients). Examined the relationship between morphological characteristics of spinal cord deformities on the preoperative MR image and functional score assessed by JOA score obtained at 1 month following surgery. Although the mean functional disability scores were reported in three groups (triangular cord configurations, A=31.8 mm 2 , post-JOA =
11.6; teardrop cord, A=39.0 mm 2 , post-JOA = 15.2; boomerang cord, A= 35.4 mm 2 , post-JOA = 14.2), no direct comparisons were reported.
(74 CSM, 52 CDH, 49 OPLL patients) retrospectively studied morphological and functional scores obtained from 12 months to 4.5 years (mean follow up of 1.5 years) after surgery in elderly patients. The author reported that their patients performed better with lesser cord distortions at baseline. The validity of these findings is difficult to judge due to poor description of performance (no report of mean, SE, p and r values).
Compared recovery percentage, calculated based on JOA scores obtained at 1 month follow up, across categories. These categories are described cross-sectional spinal cord configurations of three shapes: boomerang, teardrop, and triangular with the following means of percentage of recovery: 61.8%, 72.1% and 23%, respectively (no p or r values were reported).
(128 CSM patients) retrospectively studied a new method of evaluating the cumulative severity of stenosis captured on preoperative T1- and T2-weighted sagittal images and recovery percentage at 12 months to 9.7 years after surgery (mean follow up of 4.8 years). The authors used a six grade scale to classify the severity of spinal cord compression, describing severity in terms of anterior/posterior space and cord compressions ( Table 3.4 (II) ). The recovery percentage was calculated based on the JOA scores obtained at long term follow-up and correlated with the preoperative MRI cumulative score. As a result, the authors found a significant negative correlation between the defined MR imaging findings and recovery percentage
(r = -0.436, p <0.01).
(300 CSM patients) prospectively compared preoperative MRI and recovery percentage calculated based on the JOA scores collected at an average follow up of 19 months. The morphological changes of the spinal cord were stratified into four categories of preoperative cord compression on sagittal T1-weighted MRIs ( Table 3.4 (II) ). As a result, they found that the degree of spinal cord compression on sagittal T1-weighted MRI is not significantly correlated with the severity of myelopathy
(no p or r values were reported).
Predictor
T2 signal changes
Outcome
FS
Author
Papadopolous et al
2004
Singh et al 2001
Results
(42 multilevel CSM patients, further classification of etiology is uknown). Showed consistent association of signal intensity changes on sagittal T2-weighted MR images and functional scores assessed by JOA scale at 6 months follow up ( p <0.001, r value was not reported).
Showed that it has association with functional score assessed by walking scale at 3 months after surgery. The authors concluded that
CSM patients with higher severity scores at admission and T2 signal showed more change in functional score. Because clinical severity at baseline was not statistically adjusted between comparison groups, it is difficult to conclude that high T2 signal changes alone are
RP
Predictor
Degree of spinal intensity changes
Outcome
FS
RP
Chatley et al 2009 independently associated with functional scores after surgery (r=0.26, p =0.0011).
(64 CSM/radiculomyelopathy patients). Reported findings with a report of insignificant association between preoperative signal intensity changes on T2W and functional score assessed by the modified JOA scale at 6 months follow-up period (exact p and r values were not reported).
Yukawa et al 2007 (142 CSM/OPLL/CDH/calcification of the yellow ligaments patients). Showed consistent association of signal intensity changes on sagittal T2-weighted MR images and functional scores assessed by JOA scale, on average, 40 months follows up after surgery ( p =0.012, r value was not reported).
Houten et al 2003 (38 CSM/OPLL patients). Found that there was no significant difference across comparison groups obtained at 2 months to 18 months after surgery (mean follow up of 7.2 months) (exact p and r values were not reported).
Matsuda et al 1991 (12 CDH, 16 CSM, 1 OPLL). Showed consistent association of signal intensity changes on sagittal T2-weighted MR images and functional scores assessed by JOA scale at 1 month to 14 months after surgery (mean follow up of 5.4 months) ( p <0.05, r value was not reported).
Yagi et al 2010 (60 CSM, 11 OPLL patients). The JOA scores assessed, on average, at 60.6 months (range 36–132 months) were significantly lower in patients whose MR images indicated the intramedullary signal intensity change ( p = 0.039, r value was not reported).
Wada et al 1995
Shen et al 2009
Houten et al 2002
Mizuno et al 2003
Yone et al 1991
Chung et al 2002
Yamazaki et al 2002
Showed the absence of a relationship between signal changes and functional score obtained at 1.5 months. The inconsistencies in findings by Wada et al 1995 could be due to variable view dimensions (axial versus sagittal) and approaches used to describe signal intensity changes (‘yes/no’ versus ‘snake eye/non-snake eye’ appearances).
(64 cervical spondylosis (ie, cervical radiculopathy and/or myelopathy)). Reported findings with a report of insignificant association between preoperative signal intensity changes on T2W and functional score assessed by the original JOA scale at 1, 26, 104 weeks follow-up (exact p and r values were not reported).
There was not statistically significant correlation between high T2 signal and recovery percentage, evaluated by the Hirabayashi’s formula based on the modified version of JOA scale ( p and r values were not reported).
(82 CSM, 62 OPLL patients) found significant difference in recovery percentage, calculated from JOA scores from 3 to 6 months after surgery (mean follow up of 3.7 months), in SEA (snake-eye appearance, characterized as nearly symmetrical round high signal intensity of the spinal parenchyma resembling the face of a snake; 32.2 ±15.1%) compared to the NSEA (no snake-eye appearance) group (47.1
±12.1%) ( p <0.001, r value was not reported).
There was not statistically significant correlation between high T2 signal and recovery percentage, evaluated by the Hirabayashi’s formula based on the original JOA scores ( p and r values were not reported).
Shen et al 2009
Author
(64 cervical spondylosis (ie, cervical radiculopathy and/or myelopathy)). Reported findings with a report of insignificant association between preoperative signal intensity changes on T2W and functional score assessed by the original JOA scale at 1, 26, 104 weeks follow-up (exact p and r values were not reported).
Results
Avadhani et al 2010 (35 cervical compressive myelopathy patients, no specifics of etiology was listed) found non-significant difference in functional score, calculated from Nurick scale from 36 to 83 months after surgery (mean follow up of 51.3 months), in Grade 1 (intermediate intensity) compared to the Grade 2 group (bright intensity) ( p >0.05, r value was not reported).
Shin et al 2010 (70 cervical myelopathy patients, no specifics of etiology was listed) found significant difference in functional score, calculated from the original JOA obtained from 10.4 to 50.5 months after surgery (mean follow up of 32.7 months), in Grade 1 (light intensity change) compared to the Grade 2 group (bright intensity) ( p <0.0001, r value was not reported).
(64 CSM patients). To study the effect of this variable on functional recovery percentage after controlling for other important Chen et al 2001 confounding variables such as age, sex, preoperative JOA score, cervical curvature, and cord compression ratio, Chen et al confirmed these associations (p <0.001).
Yukawa et al 2007 (142 CSM/OPLL/CDH/calcification of the yellow ligaments patients) showed an association between highly intense and well-defined
Area of signal intensity changes
Intensity ratio
FS
PR
FS
RP
Uchida et al 2005 (135 CSM/OPLL patients) reported no significant association, the observed differences could be attributed to different MR imaging classifications used to assess the degree of signal intensity changes ( PCC = 0.32, p <0.05).
Avadhani et al 2010 There was no significant difference between degree of signal intensity changes & recovery percentage.
Shin et al 2010 border of signal intensity area and poor recovery percentage obtained from 12 to 90 months after surgery (mean follow up of 40 months),
( p = -0.018).
Patients w/o T2 signal changes had the best outcomes. The patients in Group 1 (w/ predominantly faint and indistinct border) had significantly better recovery than the Group 2 (w/ predominantly intense and well-defined border) (p =0.002, r value was not reported).
Using multiple regression, lower degree of signal intensity change was found to be associated w/ better outcomes ( p =0.03, r value was not reported).
Chatley et al 2009
Mastronardi et al
2007
The T2 hyperintensity changes were quantified and divided into 2 groups: focal (≤2 segments) and multisegmental (>2 segments). The postoperative mJOA scale scores were statistically significantly lower in patients with multisegmental signal intensity change as compared w/ those w/o this change or those with focal signal intensity change ( p < 0.05).
Patients with signal intensity changes in multiple segments showed a poor outcome in comparison with those patients with only focal signal intensity changes; the mean postoperative mJOA score was 14.6 ± 1.3 in patients with signal changes in multiple segments and
15.8 ± 0.9 in patients with focal signal intensity changes, a non-significant difference.
Wada et al 1999 (85 CSM patients), reported a significant relationship between multisegmental area of high signal intensity on preoperative MRIs and lower functional scores obtained from 24.4 to 48.3 months after surgery (mean follow up of 35.1 months) ( p <0.05).
Avadhani et al 2010 Showed no significant differences in original and modified Nurick scores between patients with focal or multisegmental high-intensity
T2 signal change ( p =0.32 and p =0.32, respectively).
Shin et al 2010 The length of signal intensity did not correlate significantly with functional score assessed by JOA scale (p =0.096, no r value was reported).
Wada et al 1995
Papadopolous et al
2004
Found no statistical difference in post-operative JOA scores obtained at 1.5 months between patients with multisegmental areas of high
MRI intensity (13.4±1.1) and ones with focal areas (13.5±2.0%) ( p >0.05).
(42 CSM patients). Reported a significant relationship between multisegmental area of high signal intensity on preoperative MRIs and poor recovery percentage obtained at 6 months follow up ( p =0.001).
Chatley et al 2009
Wada et al 1999
Fernandez et al
2007
Wada et al 1995
Ahn et al 2010
Zhang et al 2010
Zhang et al 2010
Okada et al 1993
The recovery rates, evaluated by mJOA scale score, were statistically significantly lower in patients with multisegmental signal intensity change as compared with those w/o this change or those w/ focal signal intensity change ( p < 0.05).
Reported a significant relationship between multisegmental area of high signal intensity on preoperative MRIs and poor recovery percentage ( p <0.05).
(12 CDH, 55 OPLL patients) reported a significant relationship between multisegmental area of high signal intensity on preoperative
MRIs and poor recovery percentage obtained from 23 to 120 months after surgery (mean follow up of 39 months) ( p <0.001).
(31 CSM patients) reported no significance in recovery percentage obtained at 1.5 months follow up after surgery across comparison groups ( p >0.05).
The localized marginal pattern of the segments with high signal intensity on the T2-weighted images showed a significant inverse correlation with the recovery rate (r = -0.31, p = 0.00; r = -2.42, p = 0.00, respectively). The negative correlation became more significant with increasing height of the upper segment with high signal intensity (r = 2.42, p = 0.03).
(73 patients with cervical compressive myelopathy patients, etiology was not listed) showed the significance of the relationship between post-operative JOA score obtained at 12 months follow up and the mean preoperative intensity ratio ( p <0.001, r value was not reported).
Using multivariate analysis, the author showed the role of SI ratio in predicting the extent of functional recovery: recovery rate = 0.591 -
0.006 × age - 0.842 × lg (SI ratio) - 0.001 × duration of disease + 0.46 × preoperative JOA score + 0.1 × Babinsk sign. Renter = 0.10,
Rout = 0.15, R = 0.857, R 2 = 0.734.
(23 had OPLL, 34 had CSM, 17 CDH patients) showed the significance of the relationship between recovery percentage and the mean preoperative intensity ratio at baseline, in particular in groups of myelopathy due to OPLL and CSM, r=0.537 ( p <0.01) and r=0.426
( p
<0.01), respectively. The recovery percentages were illustrated in all thee groups (OPLL, RR (54.7 ±17.7%); CSM, recovery
Patterns of
T1/T2 on sagittal image
FS
RP
Position of T2 signal changes
Predictor
Focal versus multisegmental
RP
Outcome
FS
RP percentage (52.21 ±5.9%); CDH, recovery percentage (78.3 ±19.1%), however the CDH group had a significantly higher recovery percentage ( p <0.01) (no follow up time was reported).
Avadhani et al 2010 A significant difference was observed in the postoperative Nurick grades w/ low SI changes in preoperative T1WI, although the two groups of patients were similar in terms of mean age, duration of symptoms, pre- and postoperative transverse area of the spinal cord, preoperative Nurick score, and follow-up period.
Yagi et al 2010 There was a significant correlation between hypointensity in T1-weighted MR images and poorer functional status evaluated by JOA scale ( p =0.069, no r value was reported).
Morio et al
Yagi et al 2010
The authors showed a statistically significant difference in N/Hi (48.0± 24.9%) groups and Lo/Hi (19.1± 22.8%), respectively
( p =0.0259). Using stepwise multiple regression, the best model for prediction of recovery percentage included preoperative signal pattern combined with clinical features such as age and duration of symptoms (adjusted r 2 = 0.297; p =0.0002).
Avadhani et al 2010 A significant difference was observed in the postoperative Nurick grades w/ low SI changes in preoperative T1WI, although the two groups of patients were similar in terms of mean age, duration of symptoms, pre- and postoperative transverse area of the spinal cord, preoperative Nurick score, and follow-up period. Using multiple regression modelling, the author confirmed the significance of low SI changes on T1WI as a predictor for recovery after surgery ( p <0.001, no r value was reported).
In our study, 21 (42%) of 50 patients had hypointensity in T1-weighted images (Grade III), and the tendency that hypointensity in T1-
Shen et al 2009 weighted MR images correlated to poor long-term surgical outcome was observed ( p = 0.069 and p = 0.079, respectively).
The statistically significance in percentage recovery progressed with longer time intervals of follow ups between Group A (ISI in graymatter group) and Group B (ISI in both-gray-and-white-matter), assessed by the original JOA scale at 1, 26, 104 weeks follow-up
( p =0.286, p =0.023, p =0.003, respectively).
Author Results
Singh et al 2001 (69 CSM patients) prospectively compared preoperative MRI and functional score calculated based on the Nurick scores collected at 3 months follow up. The number of levels affected by compression was scored from 0 to 7. As a result, they found that the levels of spinal cord compression on sagittal T2-weighted MRI is significantly correlated with functional scores (r=0.34, p =0.004).
Uchida et al 2005 (77 CSM, 58 OPLL patients). Reported findings with a report of significant association between preoperative number of disc level involvement and recovery percentage assessed by the original JOA scale at 12 months to 12.8 years after surgery (mean follow up of 8.3
Park et al 2006
Avadhani et al
2010 years) (CSM, PCC=0.85; OPLL, PCC=0.23, p values were not reported).
(61 CSM, 11 OPLL, 8 CDH patients). Reported findings with a report of insignificant association between preoperative number of compressed segments and recovery percentage assessed by Neurosurgical Cervical Spine Score at 3 months follow-up period (r=-0.04, p =0.37).
(35 CSM patients). Reported findings with a report of insignificant association between preoperative number of compressed segments and recovery percentage assessed by the original and modified Nurick scale on average at 9.34 months follow up after surgery ( p =0.32 and p =0.32, respectively, no r values were provided).
Ahn et al 2010 (39 CSM patients). Reported findings with a report of insignificant association between preoperative number of compressed segments and recovery percentage assessed by the original JOA scale at the mean follow-up period of 19.1 months ( p =0.37, no r value was provided).