Conditions of Participation Proposed CMS Rule
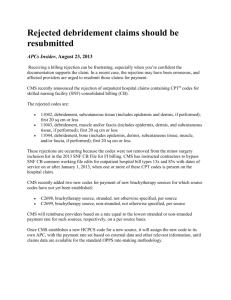
advertisement

CMS PROPOSED RULE: CONDITIONS OF PARTICIPATE; REGULATORY CHANGES Medicare and Medicaid Programs: Reform of Hospital and Critical Access Hospital Conditions of Participation; and Regulatory Provisions May 2012 to Promote Program Efficiency, Transparency, and Burden Reduction On May 10, 2012 the Centers for Medicare and Medicaid Services (CMS) published two final rules (CMS-3244-F and CMS-9070-F) aimed at reducing procedural burdens on providers by identifying existing regulations that, according to the agency, “can be eliminated as obsolete, unnecessary, burdensome, or counterproductive or that can be modified to be more effective, efficient, flexible, and streamlined.” CMS estimates that the reforms designated in the two rules will save nearly $1.1 billion across the healthcare system within a year and over $5 billion over five years. Reform of Hospital and Critical Access Hospital Conditions of Participation (CMS-3244-F) The first rule revises the Conditions of Participation (CoPs) that hospitals and critical access hospitals (CAHs) must meet in order to be eligible to participate in the Medicare and Medicaid programs. CMS estimates that total hospital savings as a result of this rule will be approximately $940 million in the first year, and the agency attributes the cost savings directly to reduced regulatory burdens rather than to reimbursement reductions. CMS released a proposed rule in October 2011 revising the CoPs for hospitals and CAHs, and requested stakeholder comment on its proposals. CMS received over 1,700 public comments, a majority of which were submitted by representatives from the hospital industry, physician groups, and non-physician practitioners. The agency noted in the rule that a number of the commenters representing physician groups were disappointed with “what they viewed as the Agency’s endorsement of the replacement of physicians with nurses and non-physician practitioners,” whereas many non-physician practitioners expressed their support for proposals that would expand their roles “to the full extent allowed under their respective State laws and regulations”. CMS addressed all comments in its responses to the proposed provisions. Noteworthy Provisions in the Final Rule The final rule allows hospitals to maintain a single governing body responsible for all facilities within a hospital system, but does not permit a multi-hospital system to be directed by a single medical staff. Hospitals therefore must maintain a “single and separate” medical staff for each hospital in their system. The AHA has since released a statement praising CMS for granting hospitals flexibility in defining a governing body while criticizing its decision to deny the same privileges to a medical staff. The final rule also adds a provision requiring at least one medical staff member to be on a hospital’s governing board, which has caused some hospitals to raise conflict of interest and time commitment concerns regarding their board members. In opposition to those commenters who supported permitting only physicians with specialized training to administer certain medications, CMS ultimately decided to allow non-physician personnel to administer certain intravenous medications and blood transfusions. The rule also finalizes its proposal to allow medical staff to include non-physician practitioners, so long as they adhere to the requirements of their hospital and/or state. Provisions Promoting Further Burden Reduction Allow CAHs to provide certain services (diagnostic and therapeutic, laboratory, radiology, and emergency procedures) through contracts with other providers or temporary agencies rather than being required to provide them directly. Allows nursing plans to be incorporated into an existing interdisciplinary plan rather than necessitating a separate plan. Permits hospitals to use their own judgment when assigning staff directors to outpatient departments based on the scope and complexity of their outpatient services, rather than requiring a single Director of Outpatient Services position. Regulatory Provisions to Promote Program Efficiency, Transparency, and Burden Reduction (CMS-9070-F) The second rule on Medicare regulatory reform is expected to save an estimated $200 million in the first year by eliminating duplicative, overlapping, and outdated regulatory requirements. The proposed rule, released in October 2011, included 14 specific proposed reforms as well as a request for comments on additional areas of future reform. Among the finalized provisions set forth by CMS, the rule will Eliminate various infection control instructions for Ambulatory Surgical Centers (ASCs); Medicaid qualification standards for physical and occupational therapists; and duplicative requirements for governing bodies of Organ Procurement Organizations; Require only higher risk End Stage Renal Disease (ESRD) facilities to comply with the full National Fire Protection Agency Life Safety Code requirements; Eliminate the specific list of emergency equipment that must be maintained by ASCs; Allow facilities, in conjunction with medical staff and their governing bodies, to develop policies and procedures that specify emergency equipment appropriate to the services they provide; Update e-prescribing technical requirements so Medicare Prescription Drug Plans meet current standards; and Replaces language referencing outdated personnel qualifications for Physical and Occupational Therapists. A complete outline of all changes to the provisions in both rules can be found in the attached tables. 2 Reform of Hospital and Critical Access Hospital Conditions of Participation (CMS-3244-F) Provision Governing body (§482.12) Patient’s rights (§482.13) Purpose Proposed Rule Final Rule Reasoning I. Revisions to Allow Flexibility and Eliminate Burdensome CoPs Changes interpretation “Governing body” can be a Same as proposed rule Reflects CMS’s belief that hospitals of the term “governing single governing body that with one addition: in a multi-hospital system can be body” to reflect a is legally responsible for all effectively governed by a single hospital’s current facilities within a multiRequires that a hospital’s governing body, and that a organizational structure. hospital system. governing body must formalized link between these include at least one interdependent entities is medical staff member. appropriate. Revises hospital reporting standards in cases of patient death that involve soft twopoint wrist restraints and no use of seclusion. Establishes new standards for staff training and death reporting. Cases in which a patient dies after being restrained with soft, two-point wrist restraints and was not held in seclusion do not need to be reported to CMS within 24 hours. Hospitals have seven days to notify CMS following the date of patient death in these cases. Hospitals must make this information available to Same as proposed rule with the following revisions: The new provision is also expected to ensure regular communication between a hospital’s governing body and its medical staff(s). Use of soft, two-point wrist restraints is not proven to be associated with patient death. Clarifies that for those deaths related only to soft, two-point wrist restraints the hospital staff must record the information regarding the patient’s death in an internal log or other system. The staff must document 3 Provision Purpose Proposed Rule CMS in either written or electronic form immediately upon request. In addition to telephone, reporting can be done by facsimile and electronic reporting when available. Medical staff (§482.22) Relaxes the restrictions on personnel that can be designated as a member of a hospital medical staff. Physicians and nonphysicians can practice in a hospital even if they are not appointed to the hospital’s medical staff; however, they must meet the requirements of their specific hospital and adhere to laws of their state. The list of professionals eligible to serve as Final Rule Reasoning in the patient's medical record the date and time the death was: (i) Reported to CMS; or (ii) Recorded in the internal log or other system. Each entry must document the patient’s name, date of birth, date of death, name of attending physician or other licensed independent practitioner who is responsible for the care of the patient, medical record number, and primary diagnosis(es). Same as proposed rule with the following revisions: Medical staff may also include other categories of non-physician practitioners determined as eligible for appointment by the governing body in accordance with State law, including scope-of- Will allow hospitals flexibility in developing “new and expanded approaches to caregiving”. Prior regulation was too burdensome on non-physician practitioners such as APRNs, PAs, PTs, etc. Intended to address healthcare workforce shortages and provide better care to medically underserved communities. 4 Provision Purpose Proposed Rule president is expanded to include doctors of podiatric medicine (DPMs). Nursing services (§482.23) Modifies guidelines related to nursing care plans and the administration of drugs, biologicals, blood transfusions, and intravenous medications. Introduces a new policy regarding self- Nursing plans can be incorporated into an existing interdisciplinary plan rather than being a separate plan. Extends capability to prepare, administer, document, and sign for drugs and biologicals to practitioners outside of Final Rule practice laws. Medical staff must examine the credentials of all eligible candidates and then make recommendations on medical staff membership to the governing body. A candidate who has been recommended by the medical staff and appointed by the governing body be subject to all medical staff bylaws, rules, and regulations, in addition to the requirements contained in §482.22. Same as proposed rule with the following revisions: Drugs and biologicals may be prepared, administered, documented, and signed on the orders of other practitioners not specified under §482.12(c) only if Reasoning Most states laws already permit DPMs to serve in hospital leadership positions Developing two separate plans was overly burdensome on nursing staff. Limiting categories of practitioners able to administer drugs and biologicals delayed treatment and access to care. Standing orders have been proven to be effective when used by Rapid Response Teams (RRTs), in ED 5 Provision Purpose administration of certain medications for patients and their caregivers. Proposed Rule §482.12(c), provided they adhere to State and practice laws. Drugs and biologicals can be administered from standing orders (preprinted and electronic). Lifts the special training requirement for blood transfusions and intravenous medications, provided it is conducted in accordance with state law and hospital policy. Medical record services (§482.24) Changes the timeframe in which a practitioner must authenticate orders. Eases regulations regarding standing orders related to Introduces a new provision that allows hospitals to create policies where patients and their caregivers can administer certain medications. Orders can be authenticated by either the ordering practitioner or another practitioner directly responsible for the patient. Removes 48-hour Final Rule such practitioners are acting in accordance with State law, including scope- of- practice laws, hospital policies, and medical staff bylaws, rules, and regulations. A hospital must document the administration of medication “as reported by the patient (or the patient’s caregiver/support person where appropriate), in the patient’s medical record.” Same as proposed rule with the following revisions: Reasoning triage, for increasing immunization rates, and for postoperative recovery. Blood transfusion and intravenous medication training is standard practice; additional training was unnecessary. New patient self-administration provision would allow care to be more patient-centered and adaptable to patient needs. 48-hour timeframe requirement for authentication of verbal orders was overly burdensome on providers and did not result in better or safer patient care. Clarifies that all orders, must be dated, timed, and authenticated promptly by Relaxing the requirements related the ordering practitioner to standing orders is intended to 6 Provision Purpose medical records. Proposed Rule timeframe requirement and defers to hospital policy or State law to determine a timeframe. Hospitals can use standing orders in regards to medical records services provided all hospital protocols were met. Infection control (§482.42) Removes requirement for hospitals to maintain a log identifying infection control problems. Eliminates the requirement to maintain a separate infection log. Outpatient services (§482.54) Changes personnel requirements for individuals in charge of overseeing hospital Allows hospitals to assign one or more individuals to be responsible for outpatient services. Final Rule or by another practitioner who is responsible for the care of the patient “only if such a practitioner is acting in accordance with State law, including scope-ofpractice laws, hospital policies, and medical staff bylaws, rules, and regulations.” Same as the proposed rule. Same as proposed rule with the following revisions: Reasoning improve evidence-based medicine practices and provide more consistent care for patients. Maintaining a separate infection log in addition to hospitals’ infection control surveillance systems was redundant and burdensome. we would also note the universal support for this proposal from several major infection control groups, such as the Infectious Diseases Society of America (IDSA), the Association for Professionals in Infection Control and Epidemiology (APIC), and the Society for Healthcare Epidemiology of America (SHEA). Many hospitals have either integrated their inpatient and outpatient services or expanded their outpatient departments, and 7 Provision Transplant Center Process Requirements – Organ recovery and receipt (§482.92) Definitions (§485.602) and Provision of services (§485.635) Purpose Proposed Rule Final Rule Reasoning outpatient departments. Hospitals can use their own judgment when assigning staff members based on the scope and complexity of their outpatient services. Critical Access Hospitals (CAHs) are exempt from the requirement for hospitals to have a single director of outpatient services. therefore frequently assign more than one individual to oversee outpatient coordination. Requiring an additional “overseer” was creating unnecessary costs and confusion associated with staffing. Eliminates some requirements for transplant centers related to blood type verification Same as proposed rule. CfC blood type verification rules were redundant of existing transplant center an OPO regulations, and therefore removing them will not result in harm to patient safety Changes requirement that CAHs must provide certain services directly Removes requirement that the transplant team must verify blood type before organ recovery Eliminates requirement that CAH staff must provide the following services directly: (1) certain diagnostic and therapeutic services; (2) laboratory services; (3) radiology services; and (4) emergency procedures. Same as proposed rule. Removing the unnecessary extra verification will free up time and resources for transplant centers Not allowing CAHs flexibility to contract with providers or temporary agencies hinders their ability to alleviate work force shortages and most efficiently coordinate their resources Governing body or person responsible for the CAH will be responsible for all 8 Provision Purpose Pharmaceutical services (§482.25) Technical change to quality assurance reporting requirement Personnel qualifications (§485.604) Revises definition of clinical nurse specialist Proposed Rule Final Rule services furnished by the CAH whether furnished directly or under contracts or arrangements. II. Clarifying Changes The term “quality Same as proposed rule. assurance program” is replaced with the term “quality assessment and performance improvement program”. All drug errors, adverse reactions, and incompatibilities will be subject to requirements of QAPI programs listed under §482.21. A clinical nurse specialist is Changes the definition now a “registered nurse slightly: licensed to practice nursing in the State in which the A clinical nurse specialist is clinical nurse specialist “a registered nurse and is services are performed, licensed to practice that holds an advanced nursing in degree in a defined clinical the State in which the area of nursing from an clinical nurse specialist accredited educational services are performed in institution” accordance with State nurse licensing laws and regulations; and holds a master’s or doctoral level Reasoning Reflects a more current term that has been undertaken at hospitals to ensure quality of care. Adding the phrase “in accordance with State nurse licensing laws and regulations” will ensure that an existing CNS will continue to be evaluated based on their State licensing laws and regulations. CMS agreed with some commenters who felt it would be unfair to require national certification for CNSs. 9 Provision Surgical services (§485.639) Purpose Clarifies that surgical services are an optional service for CAHs Proposed Rule Language of statue now reads: “If a CAH provides surgical services, surgical procedures must be performed in a safe manner…” Final Rule degree in a defined clinical area of nursing from an accredited educational institution.” Same as proposed rule. Reasoning Surgical services are not mandatory for CAHs as specified under section 1820(c) of the surgical services CoP Regulatory Provisions to Promote Program Efficiency, Transparency, and Burden Reduction (CMS-9070-F) Provision End-Stage Renal Disease (ESRD) Facilities (§494.60) ASC Emergency Equipment (§416.41 Purpose Prior Regulation Final Rule Regulation I. Removes Unnecessary Burdensome Requirements Lessens regulatory fire ESRDs were subject to the Mandatory compliance with and safety requirements same set of standardized NFPA 101 LSC regulations is on ESRDs Federal Life Safety Code restricted to only those facilities (LSC) and National Fire that are adjacent to “high hazard Protection Agency (NFPA) occupancies” (i.e. close proximity regulations as all other to flammable liquids). All ESRD providers. facilities will be subject to state and local fire codes and safety standards. Grants ASCs flexibility in ASCs were required to deciding which maintain emergency emergency equipment is equipment compliant with ASCs, their governing bodies, and medical staffs can determine which emergency equipment is Reasoning ESRDs have “non-residential and unique characteristics” that are not conducive to standard CMS provider regulations and were duplicative of existing ESRD regulations. There is a very low risk of fire in outpatient dialysis fires while the costs of compliance (i.e. renovation) with fire safety regulations were disproportionately high. Some of the equipment required in prior regulations was outdated or unnecessary 10 though §416.43 and §416.49 through §416.52) appropriate for their facility rather than requiring adherence to a standardized list. all items specified in CfC 414.44, including items such as emergency call system, ventilator assistance equipment, manual breathing bag, etc. necessary and appropriate for the procedures performed at their facility. The equipment must meet the acceptable standards of practice of the ASC industry. to the services performed at a particular ASC facility. Revocation of Enrollment and Billing Privileges in the Medicare Program (§424.525) Changes the period of time a provider or supplier whose Medicare privileges have been revoked must wait before being reeligible for Medicare, depending on reason for revocation. Changes guidelines surrounding Any Medicare provider, supplier, delegated official, or authorizing official that has had their billing privileges revoked was barred from participating in Medicare for a period of no less than one year and no longer than three years. Medicare billing privileges could be deactivated if Medicare claims were not submitted during a period of 12 consecutive months. Eliminates the re-enrollment bar when the provider or supplier was removed on the basis of not responding to revalidation requests in a timely fashion. The re-enrollment bar will remain for instances when the Medicare privileges revocation was more serious. Medicare billing privileges will only be revoked for providers and suppliers who fail to submit the enrollment form (CMS-8551) for individual physicians and nonphysician practitioners. The re-enrollment bar in these situations was deemed to be an overly harsh consequence because providers’ delayed responses was usually unintentional. Deactivation of Medicare Billing Privileges (§424.540) Medicare billing privileges could be revoked if the provider failed to furnish complete and accurate enrollment information within 90 days of receiving notification to do so. Duration of Agreement for Intermediate Care Facilities for the Changes time limits for provider agreements for Intermediate Care Facilities for the Intellectually Disabled (ICFs/ID). ICFs/ID provider agreements were subject to Medicaid annual time limits. ICFs/ID were required to be surveyed for compliance at Deactivates rather than revokes privileges If a provider or supplier does not furnish requested information within 90 days of receiving notification to do so. Removes time limited agreements for ICFs/ID and replaces them with open ended agreements that will remain in effect until the Secretary or a state determines the facility does There were numerous instances in which practitioners had valid reasons for not submitting claims during a 12-month period. Prior reactivation procedure was time-consuming and overly burdensome for Medicare contractors as well as for providers and suppliers. Changes to the survey and certification period are intended to allow ICF/ID facilities flexibility in scheduling and staffing, and are expected to have a positive 11 Intellectually Disabled (§442.15 through §442.109) OMB Control Numbers for Approved Collections of Information (§400.300 and §400.310) Removal of Obsolete Provision Related to Initial Determinatio n, Appeals, and Reopenings of Part A and Part B Claims and Entitlement Determinatio ns (§405.701 Adds a requirement establishing time frames for surveying ICFs/ID for compliance. least every 12 months on a fixed schedule. If a facility was surveyed earlier due to a complaint, they were required to complete a survey again at the 12 month mark. not meet conditions of participation. impact on their ability to provide higher quality care to patients. ICFs/ID can be surveyed during a 12 – 15 month interval, which is consistent with the schedule for surveying nursing homes. If a facility is surveyed earlier in that time frame, for example at 10 months, they can use that survey for their annual certification rather than completing another one at the 12-15 month mark. II. Removes Obsolete or Duplicative Regulations or Provides Clarifying Information Updates requirements Required the collection and Removes entire requirement for An inventory of currently for collection and display of OMB-assigned the collection and display for approved CMS information display of OMB control control numbers OMB control numbers collections is displayed on the numbers public website: www.reginfo.gov/public/do/PR AMain, which is a more suitable and efficient method to publish this information. Removes obsolete All provisions concerning Replaces these procedures Replacing previous provisions appeals process rules initial determinations, formally listed in subparts G and with one set of guidelines is from the Benefits appeals, and reopenings of H with a set of new procedures intended to remove confusion Improvement and Part A and Part B claims, and specified in subpart I. and simplify the appeals process Protection Act of 2000 determinations and appeals for providers, suppliers, and (BIPA) that have since regarding an individual’s beneficiaries. been replaced with entitlement to benefits updated rules. under Parts A and B, were specified 42 CFR part 405 subparts G and H 12 through §405.877) ASC Infection Control Program (§416.440) Eliminates those infection control requirements for ASCs that were listed under the Environment CfC 42 CFR §416.44(a)(3) E-prescribing (§423.160) Updates e-prescribing foundation standards for e-prescribing in the Medicare Part D program. Under the physical environment standard in 42 CFR 416.44(a)(3) ASCs were required to establish a program for identifying and preventing infections, maintaining a sanitary environment, and reporting the results to the appropriate authorities Required use of Health Care Eligibility Benefit Inquiry and Response Version 4010 and 4010A1 specified under the HIPAA Electronic Transaction Standards rule for covered entities conducting HIPAA standards. Required use of NCPDP Telecommunication Standard Implementation Guide Version 5.1 and Batch Standard Implementation Guide Version 1.1 for transmitting eligibility inquiries and responses between dispensers and Part D sponsors. Physical and Occupational Therapist Updates language regarding qualifications Current provider qualifications for physical Completely removes the Environment CfC ASCs are already subject to infection control requirements in the Infection Control CfC under §416.51. Requiring additional compliance under the Environment CfC for the same conditions was duplicative and confusing. Covered entities that conduct HIPAA standards must now use Health Care Eligibility Benefit Inquiry and Response, Version 5010 by January 1, 2012. Maintains consistency with current HIPAA transaction standards Requires NCPDP Telecommunication Standard Implementation Guide Version D.0 and Batch Standard Implementation Guide Version 1.2 for retail pharmacy drug transactions including health care claims or equivalent encounter information, eligibility for a health plan, referral certification and authorization, and coordination of benefits. Removes language referencing outdated personnel Prior regulations contained outdated terminology 13 Qualifications (§440.110) for physical therapists and occupational therapists participating in Medicare and Medicaid. therapists are located under 42 CFR 440.110(a)(2) and for occupational therapists under 440.110(b)(2). qualifications under §440.110 of current Medicaid regulations and replaces it with an instruction to cross-reference updated qualifications under §484.4. Definition of Donor Document (§486.302) Updates the definition of “donor document” Previous regulation identified an “individual’s choice” but not does allow the individual to be more specific should they choose to include more detail regarding which tissues and/or organs they wish to donate. New definition of donor document will be “any documented indication of an individual’s choice regarding his or her wishes concerning organ and/or tissue donation that was made by that individual or another authorized individual in accordance with any applicable State law.” Administratio n and Governing Body (§486.324) Corrects typographical error (a duplicative paragraph) in 71 FR 30982 Requirement for Enrolling in the Medicare Program (§424.510) Corrects typographical error (an incorrect reference) in §424.510(a) Redefining Discontinues use of Incorrect reference in paragraph (c) referencing the effective date for reimbursement for providers and suppliers seeking accreditation concerning professional organizations and did not deal with professionals who received training outside of the United States. Updating the definitions will allow fewer PT and OT professionals to be excluded from providing Medicaid services and “strengthens the consistency of standards across Medicare and Medicaid”. New definition reflects the various new choices an individual has when indicating they wish to be a donor. New definition also includes the “executed by the patient” language to emphasize the voluntary nature of donation. Removes paragraph (e) which is duplicative of paragraph (d) immediately preceding it Error correction Changes the reference to paragraph (d) which contains information on enrollment requirements Error correction III. Responds to Stakeholder Concerns The term “recipient” was “Beneficiary” means all Reflects terminology that is 14 the Term “Beneficiary” (§400.200 through §400.203) term “recipient” and replaces it with “beneficiary” throughout 42 CFR chapter IV. used interchangeably with the term “beneficiary” individuals who are entitled to or eligible for Medicare or Medicaid services. already widely used Replace the Terms “Mental Retardation” and “Mentally Retarded” with “Intellectual Disability” and “Intellectuall y Disabled” (throughout CFR title IV) Updates terminology regarding intellectually disabled individuals. The terms “mentally retarded” and “mental retardation” were used in statutory language. “Intellectually disabled” will replace “mentally retarded” and “intellectual disability” will replace “mental retardation”. “Individuals with Intellectual Disabilities” will replace all of the following terms: “the mentally retarded”; “mentally retarded persons”; and “mentally retarded individuals”. Also we clarify that “individuals with intellectual disabilities or developmental disabilities” will replace “mentally retarded or developmentally disabled.” After public comment from provider and advocate organizations, CMS wanted to be consistent with “Rosa’s Law” (Pub. L. 111-256) that amended terminology related to intellectual disabilities in this way. 15