lt24175-sup-0001-suppinfo
advertisement
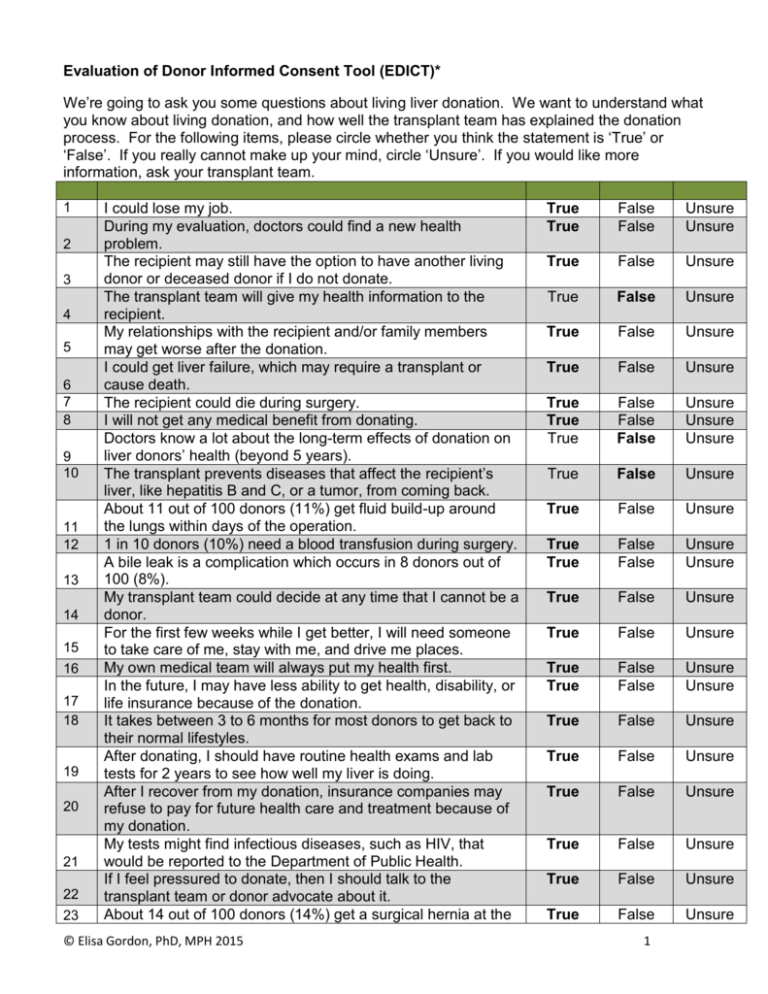
Evaluation of Donor Informed Consent Tool (EDICT)* We’re going to ask you some questions about living liver donation. We want to understand what you know about living donation, and how well the transplant team has explained the donation process. For the following items, please circle whether you think the statement is ‘True’ or ‘False’. If you really cannot make up your mind, circle ‘Unsure’. If you would like more information, ask your transplant team. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 I could lose my job. During my evaluation, doctors could find a new health problem. The recipient may still have the option to have another living donor or deceased donor if I do not donate. The transplant team will give my health information to the recipient. My relationships with the recipient and/or family members may get worse after the donation. I could get liver failure, which may require a transplant or cause death. The recipient could die during surgery. I will not get any medical benefit from donating. Doctors know a lot about the long-term effects of donation on liver donors’ health (beyond 5 years). The transplant prevents diseases that affect the recipient’s liver, like hepatitis B and C, or a tumor, from coming back. About 11 out of 100 donors (11%) get fluid build-up around the lungs within days of the operation. 1 in 10 donors (10%) need a blood transfusion during surgery. A bile leak is a complication which occurs in 8 donors out of 100 (8%). My transplant team could decide at any time that I cannot be a donor. For the first few weeks while I get better, I will need someone to take care of me, stay with me, and drive me places. My own medical team will always put my health first. In the future, I may have less ability to get health, disability, or life insurance because of the donation. It takes between 3 to 6 months for most donors to get back to their normal lifestyles. After donating, I should have routine health exams and lab tests for 2 years to see how well my liver is doing. After I recover from my donation, insurance companies may refuse to pay for future health care and treatment because of my donation. My tests might find infectious diseases, such as HIV, that would be reported to the Department of Public Health. If I feel pressured to donate, then I should talk to the transplant team or donor advocate about it. About 14 out of 100 donors (14%) get a surgical hernia at the © Elisa Gordon, PhD, MPH 2015 True True False False Unsure Unsure True False Unsure True False Unsure True False Unsure True False Unsure True True True False False False Unsure Unsure Unsure True False Unsure True False Unsure True True False False Unsure Unsure True False Unsure True False Unsure True True False False Unsure Unsure True False Unsure True False Unsure True False Unsure True False Unsure True False Unsure True False Unsure 1 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 wound site. After my liver segment has been removed, the doctors could find out that they cannot put it into the recipient. If I decide to not donate, a medical excuse will be given to the recipient and the recipient’s family. Up to 1 in 10 patients (10%) who get a blood transfusion get breathing problems, fever, headache, shock, kidney damage, or rash. The donated liver may not function in the recipient. The recipient and I will share the same medical team. I will have a scar on my belly. I may feel depressed, anxious, or emotionally distressed before, during, or after donating. If I need a transplant after donating, then I will be given high priority to get a new liver on the liver transplant waiting list. Most of the liver grows back within about 6 weeks of the surgery. Most fluid buildup cases happen 1 year after donating. If I am not honest about my medical history, there could be problems after I donate. About 13 donors out of 100 (13%) get a minor or severe infection. On average, 1 out of 250 donors (<1%) die from donation. The transplant team will discharge me as soon as medically possible so I do not get a hospital acquired infection. Surgeons will remove less than a fifth (20%) of the donor’s liver for an adult recipient. My donor advocate will help make sure that my rights are respected. A bile leak often gets better on its own, but sometimes needs surgery. About 3 donors out of 100 (3%) get temporary nerve damage in the arm. A mental health professional will ask about my reasons for donating. Surgeons will remove my gall bladder, which will have no impact on my lifestyle. I may stop the donation process for any reason, without penalty. Pain typically lasts for 3 to 12 weeks. Most wound site hernias happen 1 year after donating. Doctors may stop the surgery because my liver segment is no longer suitable for transplant. My hospital stay may last longer than expected because of complications. Even though my wound is healed, I may still feel tired. True False Unsure True False Unsure True False Unsure True True True True False False False False Unsure Unsure Unsure Unsure True False Unsure True False Unsure True True False False Unsure Unsure True False Unsure True True False False Unsure Unsure True False Unsure True False Unsure True False Unsure True False Unsure True False Unsure True False Unsure True False Unsure True True True False False False Unsure Unsure Unsure True False Unsure True False Unsure * Correct answers are in bold font. © Elisa Gordon, PhD, MPH 2015 2