File

Nayri Hatsakorzian
Pharm.D/MPH candidate 2014
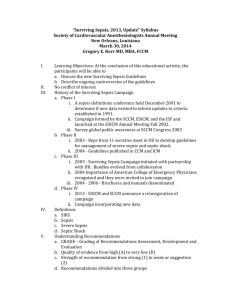
Guidelines for management of severe sepsis and septic shock
Sepsis is a systemic, deleterious host response to infection leading to
Severe sepsis: acute organ dysfunction or tissue hypoperfusion secondary to documented or suspected infection o Systemic hypoperfusion: SBP<90 or MAP<70 or a SBP decrease >40 or less than two standard deviations
And septic shock: severe sepsis plus hypotension not reversed with adequate fluid resuscitation.
Sepsis is the presence of probable or documented infection together with systemic manifestations of infection (>=2 of SIRS criteria).
Sepsis-induced tissue hypoperfusion is defined as infection-induced hypotension, elevated lactate or oliguria. When HR is above 90 and RR is above 20 then more CO2 is being accumulated in the blood due to the rapid breathing, this can lead to acidosis and passing out. Acidosis, if not resolved can lead to mental status changes leading to encephalopathy (loss of O2 in brain leads to inflammatory cytokines and CNS depression). In addition, continuous hypotension can lead to myocardial ischemia.
Site of Infection: it usually results from lung infections, followed by intra-abdominal, genitourinary, soft tissue, primary bacteremia,
IV catheter associated, surgical site and CNS.
Risk Factors: DM, surgery, cancer, immunosuppressive therapy (Prednisone > 10mg), EtOHism, COPD, chronic renal and liver, and heart failure.
Presentation: Signs and symptoms:
CNS o Altered mental status
-
-
Cardiovascular o SBP <90 or >40 reduction or MAP <65-70 o Myocardial ischemia: troponin elevations o Tachycardia; HR >90
Respiratory o Hypoxemia: decrease PaO2 o Hypercapnia: increase PaCO2 poor ventilation o Tachypnea; RR>20 and more CO2 accumulation acidosis
-
-
-
-
Renal o Oligouria: decrease urine output o Increase SCr
Metabolic o Metabolic acidosis pH<7.4 metabolic dysfunction organic acid accumulation (lactic acid)
Lactic acid elevation or persistent elevation is poor prognostic indicator. o Hyperglycemia > 120
Hematologic o Increase WBC, increase neutrophils o Fever o Thrombocytopenia
Liver o Increase in ALT/AST and bilirubin (bilirubin is a sign of liver insult) o Coagulopathy (Increase INR and aPTT)
Inflammatory markers o ESR, CRP
Localized signs of infection o Swelling, erythema, tenderness, pain, warmth, purulent drainage, or not so apparent d/t deep seated infections
Initiation of therapy:
-
-
-
Start ABX within the first 30min of onset of hypotension, every 1 hr delay is reducing chance of survival by ~8% in the first 6 hours—use broad spectrum
Draw cultures without delaying ABX
Resuscitation with crystalloid or colloid o Crystalloids: NS, 1/2NS, D5W, D5W-1/2NS, LR; up to 6-10L in the first 24 hours
LR is the most physiologically suitable for Na, Cl concentrations
NS may induce hypercholoremic metabolic acidosis since Cl=154 mEq/L
-
A disadvantage for crystalloids is that it may reduce osmotic pressure by diluting colloids and may contribute to pulmonary edema o Colloids: albumin 5% is used for resuscitation rather than 25%.
It will decrease edema by drawing fluid from interstitial space; but usually reserved for refractory cases or low albumin levels
Fluid challenges of 300-500ml every 30-60 min, then assess BP, MAP, and urine output
Agent & dose
Epinephrine (2 mg/250 ml D5W,NS)
-0.01-0.5 mcg/kg/min
- > 0.5 mcg/kg/min
- 2 nd best line
α1
- ++
- Most potent
α2
- ++
- Most potent
β1 β2
- Most potent
- +++
- +++
- +
Norepinephrine (4 mg/250 D5W,
NS)
Levophed
- 0.01-3 mcg/kg/min
- 1 st line for septic shock
- Often combined with dobutamine
Dopamine (800 mg/250 D5W, NS)
- 1-5 mcg/kg/min
- 5-15 mcg/kg/min
->10-20 mcg/kg/min
- 1 st line for septic shock
- A precursor to NorEpinephrine
+++
- 0
- 0/+
- +++
+++
- 0
- 0
- 0
+++ +++
- +
- Most potent
- Most potent
- 0
- ++
- +
Predominant clinical effects
- Increase HR, CO,
SVR
- Both inotropic and chronotropic
- Relaxes smooth muscles of bronchial tree
- Little change in
HR and CO
- Increase SVR vasoconstriction
- Low doses (1-5 mcg/kg/min): increase renal blood flow and urine output
- Intermediate doses: increase renal blood flow,
HR, contractility and CO
- High doses: alpha adrenergic effects predominates, vasoconstriction
increase BP
Side effects/notes
- Arrhythmogenic potential increase cardiac oxygen demand myocardial ischemia and direct toxicity to arterial walls
- Cardiac dysrhythmias (supraventricular tachycardia, A fib)
- Small doses can cause vasodilation thru
B2 vascular receptors
- Large doses may produce skeletal and vasculature vasoconstrictions
- Phentolamine is a adrenergic blocking agent
- Cardiac arrhythmias are likely to occur in patients with existing MI
- Norepinephrine has been shown to cause platelet hyper-reactivity and enhance platelet-mediated coagulation associated with thrombotic risk.
- Phentolamine is a adrenergic blocking agent
- Commonly induces tachycardia and arrhythmias when dose exceed 20 mcg/kg/min
- Profound effect on HR and CO
- Minimum effect on SVR
Phenylephrine (50 mg/250 D5W,
NS)
- 0.5-9 mcg/kg/min
- Synthetic a-adrenergic with no B effects used for sudden severe hypotension
+++
Dobutamine (500 mg/250 D5W, NS)
- 2-10 mcg/kg/min
- > 10-20 mcg/kg/min
- +
- ++
+
- 0
- 0
0 0
- Most potent
- Most potent
- ++
- +++
- No effects on HR,
CO.
- Increases SVR
- Profound effect on HR and CO
- Profound decrease in SVR
using alone exacerbates hypotension bc it lowers central venous pressure never use alone in pt with MAP= 60
- Reserved for patients that develop tachycardia or arrhythmia to other agents
- NorEpi is associated with serious arrhythmias
- Cardiac output is known to be high and
BP persistently low
- As salvage therapy when combined inotrope/vasopressor drugs and low-dose vasopressin have failed to achieve the
MAP target.
- Vasodilator especially at low doses at hypovolemic patients
- Used in burned patients to increase circulation to extremities
- Do not use Dobutamine in heart failure patients due to increase mortality
- Dobutamine significantly increases myocardial oxygen consumption induction of ischemia
Vasopressin
- 0.01-0.03 U/min
- Increases cAMP which increase water permeability to renal tubules resulting in decrease urine volume and increased osmolality
- Direct vasoconstrictor without inotropic or chronotropic effects
- Increase BP,
SVR, and urine output
- Doses over 0.03U/min should be reserved for salvage therapy (failure to achieve MAP)
- May be useful in Hemophiliacs bc it increases Factor VIII levels
- Mainly used for diabetes insipidus
- May be added to norepinephrine to increase MAP or to decrease
CO= HR x Stroke Volume; Stroke Volume= End diastolic volume – End systolic volume
- DO NOT administer vasopressin as initial vasopressor in septic shock pt
SIRS
- Fever >38.3 or hypothermia < 36
- HR > 90
- RR > 20
- Leukocytosis > 12 or leukopenia <4
Severe sepsis
- Systemic hypotension:
SBP<90 or MAP<70 or a SBP decrease >40 or less than two standard dev
- Lactate above NL
- Uop < 0.5ml/kg/hr >2 hr despite fluid resuscitation
- Pa O2/FiO2 <250 in absence of PNA
- SCr > 2
- Bilirubin > 2
-Thrombocyotpenia <
100,000
- INR > 1.5
norepinephrine dose.
Septic shock
- Severe sepsis plus hypotension not reversed with adequate fluid resuscitation.
First 3 hrs
- lactate, blood Cx
- broad spectrum
ABX
- 30ml/kg crystalloid for hypotN & lactate>
4
VTE PPX
- Daily LMWH
- SCD
Stress Ulcer PPX
- H2RA
- PPI
Nutrition
- Enteral vs. TPN
Unseccessful resuscitation -->
Vasopressors -->
- MAP>65
- Normalized lactate
- Uop > 0.5ml/kg/hr
- O
2 saturation of
70%
Glucose controle with insulin if
BG> 180; goal <
180
Mechanical ventilation of sepsis induced ARDS
- elevated head of bed to prevent VAP
Reference: Dellinger RP, et al. Society of Critical Care Medicine and the European Society of Intensive Care Medicine. Surviving Sepsis
Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. DOI: 10.1097/CCM.0b013e31827e83af
-
-
-
-
Vasopressors:
-
-
-
Vasopressor therapy initially target a MAP of 65
Norepinephrine as the 1 st choice vasopressor
Epinephrine (added or substituded to NorEpi) when an additional agent is needed to maintain adequate blood pressure
Vasopressin (up to 0.03U/min) can be added to NorEpi with the intent of raising MAP to target or decreasing
NorEpi dosage
Low dose Vasopressin is not recommended as the single initial vasopressor for treatment of sepsis-induced hypotension, and vasopressin doses higher than 0.03-0.04 U/min should be reserved for salvage therapy (failure to achieve an adequate MAP with other vasopressor agents)
Dopamine as an alternative vasopressor agent to NorEpi only in highly selected patients (patients with low risk of tachyarrhythmias and absolute or relative bradycardia)
Phenylephrine is not recommended in the treatment of septic shock except in the following circumstances: o NorEpi is associated with serious arrhythmias o Cardiac output is known to be high and BP persistently low o As salvage therapy when combined inotrope/vasopressor drugs and low-dose vasopressin have failed to achieve the MAP target.