02 Programme Handbook 2013 Midwifery
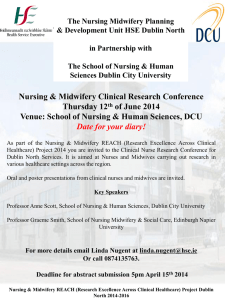
advertisement

Faculty of Health and Applied Sciences Version 1/2013 Date 06/09/2013 Programme Handbook The Programme Handbook provides you with a reference point throughout your studies at UWE Programme Name: BSC (HONS) MIDWIFERY 3 YEAR Programme Leader: Geraldine Lucas Campus and Cohort: Glenside September 2013 Academic Year: 2013/14 Version 6.1 26/06/13 Aim of the Handbook The handbook is designed to provide information relevant to the programme. The information in the handbook may also be provided in a number of other electronic or paper sources and this document provides links to the definitive data sources wherever possible. The B.Sc.(Hons) Midwifery programme has been designed to produce midwives who, upon registration, offer women and their families safe and holistic care, which recognises individual emotional, cultural and socio-economic needs. The programme offers a variety of opportunities to develop the professional skills, knowledge and values necessary for effective midwifery practice; which include skills in leadership and advocacy, a critical awareness of issues impacting upon maternity services and the ability to seek out and critique the evidence that informs practice. The development of these key elements are carefully constructed through academic personal tutoring, shared and inter-professional learning and opportunities to engage in skills simulations. During your period of education at this University, you will be encouraged to adopt a professional approach to your learning and to ensure that your interactions with the general public, women and families in your care, mentors and tutors fully reflect the Code of Practice that governs midwifery practice. The midwifery profession is regulated by the Nursing and Midwifery Council (NMC). This professional body exists to safeguard the health and well-being of the public. To facilitate this objective, a register of all qualified midwives is maintained and midwives are required to complete an intention to practice (ITP) form on an annual basis, once qualified. The NMC sets standards for midwifery practice and the education of midwives, one of which is that each Higher Education Institute (HEI) assigns a Lead Midwife for Education (LME). The appointed LME at this university is Teresa Shalofsky. The LME is the strategic lead for all midwifery education programmes within the HEI and is accountable to the NMC for leading and monitoring education and workforce development. To do this, the LME liaises closely with the Head of Department, Sarah Green, local supervisors and heads of midwifery. At the end of a programme of midwifery studies, the LME is responsible for determining that a student is competent to perform the role of the midwife and is required to sign a declaration of good health and character, for that student, prior to his or her entry to the register. For more information about the NMC Code of Practice for Nurses and Midwives, Midwives rules and standards and the standards for preregistration midwifery education you should visit the NMC website www.nmc-uk.org. Throughout your programme of education these documents will be constantly referred to. The Midwifery programme is part of the University’s interprofessional undergraduate modular framework which includes various nursing, social work, physiotherapy and radiology programmes. These programmes consist of a number of differing types of modules: 2 Professional pathway modules These are the modules that are focused on midwifery theory and practice where you will develop the core skills and knowledge required of midwives; Interprofessional modules These are modules where you will, together with other health and social care professionals, be introduced and assisted to develop knowledge, skills and attitudes that actively promote interprofessional and interagency collaboration: There is one IP module in year 2 and one in year 3; Shared learning modules These are modules where you share the same knowledge base as other health and social care professionals and therefore learn together. In the midwifery programme, there are 5 shared modules: 1 in year one (shared across all nursing branches and midwifery ), a shared research module in year 2, and a shared dissertation module in year 3. During the programme you will spend at least 50% of your time in clinical placement. UWE currently links to a number of different NHS trusts and placement areas in Wiltshire, South Gloucestershire, Bristol, Somerset and Gloucestershire. You will experience midwifery and other associated practice in both primary and acute care settings, spending time in community midwifery teams, midwifery led units, hospital wards and clinics and delivery suites. This will involve daily travel and shift patterns, which span the requirements of the service, and which will involve nights, weekends and bank holiday periods. You are expected to follow the shift pattern of your assigned mentor but may, in exceptional circumstances, request to alter a shift. Permission to change your shift is granted at the discretion of the midwife responsible for co-ordinating student off-duty. It is important that you make the most of placement opportunities in order to make the necessary links between theory and practice to enable you to meet NMC pre-registration midwifery standards against which you will be assessed. The programme is co-ordinated by programme manager, Geraldine Lucas and coprogramme manager Susan Davis. Individual modules are managed by module leaders. You should familiarise yourself with the systems for referral within this handbook, should you find you have any concerns. You will be allocated an academic personal tutor who will work with you to develop your graduate and clinical skills and who will signpost you to further, more targeted, support as required. This relationship is largely directed by you and you are expected to keep your academic personal tutor appraised of significant changes in your circumstances which may affect your performance. 3 On behalf of the midwifery team, we hope that you enjoy the midwifery programme and find it both challenging and rewarding. Lead Midwife for Education Programme Manager Co Programme Manager [Add other relevant links here] Please note that the electronic version of the handbook will be kept up to date and you will be notified of any significant changes. If you have taken a hard copy of any information please remember to refer back to the electronic version to ensure that you are working with the most up to date information. [To update table of contents and page numbers below, click into the table until the tab update table appears (just above the word ‘content’, click update table then select page numbers only]. 4 Contents 1. Programme team contact information .................................................................. 6 2. Programme specific information .......................................................................... 8 3. Additional Information ........................................................................................ 24 4. Key Faculty Staff................................................................................................ 36 5. Communication .................................................................................................. 38 6. Regulations/Policies .......................................................................................... 39 7. Advice and Support ........................................................................................... 43 8. Insurance Guidelines ......................................................................................... 45 5 1. Programme team contact information At UWE Bristol, the programme manager is a core member of the team. They are responsible for overseeing the quality of the relevant courses. They will work closely with academics and practice colleague to achieve this. An important role of the programme manager is to support their team to design and deliver innovative and creative curriculums. This can be achieved in a number of ways, including the use of technology and service users. Programme managers take an active role in the revalidation process, ensuring that students are fit to practice upon qualification. Programme managers will also work in close collaboration with academic personal tutors to ensure that students are being supported, and receive guidance with their training. The programme manager in midwifery is supported by a co programme manager for quality of placements Programme Manager Geraldine Lucas Programme Team: - Please below for team members and contact information To dial direct, use Bristol code 0117 (if necessary) followed by 32 and the extension number Name Surname Marian Bailey 1A04 Andy Yelland 2A07 Jo Jones 2A06 88587 Jo.Jones@uwe.ac.uk Sue Davis 1A07 88639 Susan.Davis@uwe.ac.uk Jane Pilston 1A07 88333 2A05 88694 Rona.Lockyersheppsheppard@uwe.ac.uk Rona LockyerShes sheppard Room No Ext No 88524 88776 6 email address marian2.Bailey@uwe.ac.uk.uk Andrew.yelland@uwe.ac.uk Jane.Pilston@uwe.ac.uk Jenny Hall 2A02 88586 Jenny.Hall@uwe.ac.uk Teresa Shalofsky 2A01 88579 Teresa.Shalofsky@uwe.ac.uk Sian n Mclaughli 2A02 88519 Sian.Mclaughlin@uwe.ac.uk Mary Mitchell 2A06 88892 Mary.Mitchell@uwe.ac.uk Gerry Lucas 2A03 88578 Geraldine.Lucas@uwe.ac.uk Caroline Rutter 2A07 88798 Caroline.Rutter@uwe.ac.uk Gillian 1A04 88963 2B24 88560 Fax 88811 Ottley Administration Contact Jenny Phillips 7 Gillian.Otttley@uwe.ac.uk 2. Programme specific information PROGRAMME SPECIFICATION Section 1: Basic Data Awarding institution/body University of the West of England Teaching institution University of the West of England Delivery Location(s) University of the West of England Faculty responsible for programme Health and Life Sciences Modular Scheme title Professional Statutory or Regulatory Body Links (type and dates) Nursing and Midwifery Council Highest award title BSc(Hons) Midwifery Default award title None Interim award titles Cert HE Health and Social Studies Dip HE Health and Social Studies BSc Health and Social Studies 8 UWE progression route Mode(s) of delivery Full-time Codes UCAS code B711 JACS code ISIS code HESA code Relevant QAA subject benchmark statements Midwifery (2001) On-going/valid until* (*delete as appropriate/insert end date) 01/09/2010 – for students enrolling on this programme on or after 1st Sept 2010 Valid from (insert date if appropriate) Original Validation Date: Latest Committee Approval… Date:… Version Code 9 Section 2: Philosophy of the Programme Midwifery is a practice based profession. The essential values and beliefs on which the award is founded are inextricably linked to the philosophy of midwifery care. This is based upon the assertion that midwifery is both an art and a science, with practice that is grounded in evidence. The focus is upon a woman-centred, midwifery model of care in which normality and the naturalness of pregnancy is promoted and women are supported in achieving positive and emotionally fulfilling childbirth experiences. The curriculum is therefore designed to prepare students to become self-aware, reflective, competent, contemplative midwives who are able to support and care for women in ways which echo this philosophy. It also involves knowing when and how to intervene to promote safety if this becomes necessary. It acknowledges the need to work with other professional groups and agencies within safe boundaries to provide effective, holistic and equitable care for women in all situations. Educational aims of the programme To prepare the student for entry to Part 2 of the Nursing and Midwifery Council’s Professional Register in accordance with the professional and statutory requirements. To enable the student to become a safe, competent and reliable practitioner who, on the point of registration, will be able to provide holistic and high quality care which is both empowering and respectful of individual needs. To develop a midwife who is able to study independently and who is committed to the concept of lifelong learning in both his/her personal and professional development. To promote the development of a reflective and reflexive practitioner. To enable the student, at the point of registration, to be an accountable, critical thinking midwife, able to communicate information and ideas, and whose practice is informed by a range of sources of evidence. 10 To actively participate in and strengthen shared learning within the Faculty. To provide wide ranging clinical experience which prepares the student to develop the skills required to fulfil the responsibilities of a midwife in a variety of clinical and non-clinical practice settings. To provide a programme that focuses on a model of care in which normality and the naturalness of pregnancy and childbirth is promoted, but also acknowledges the need to be “with woman” when complex issues arise. To actively involve students in caseload midwifery and prepare them for autonomous practice. To utilise innovative teaching and learning strategies which enable student to value theory and practice. To develop a midwife who is able to work flexibly within both a national and international context. Section 3: Learning outcomes of the programme The award route provides opportunities for students to develop and demonstrate knowledge and understanding, qualities, skills and other attributes in the following areas: … A Knowledge and understanding Learning outcomes A Knowledge and understanding of: Teaching, Learning and Assessment Strategies Teaching/learning strategies: 11 methods and 1. The skills and attitudes appropriate to providing midwifery care. 2. The impact of psychological, sociological, political and spiritual factors and how these affect the woman, her neonate and family 3. The biological sciences which underpin and support midwifery practice Acquisition of 1-5 is through structured study days within the University and the content of these may include lectures, student-led seminars, reflection, skills sessions, discussions, workbooks and work-based learning days. Additional support is provided through library and IT sessions to develop study and computer skills. 4. The contribution of the midwife to public health 5. The principles and practice of medicines management for women accessing midwifery care Throughout, the student is encouraged to undertake independent reading both to supplement and consolidate what is being taught/ 2learnt and to broaden individual knowledge and understanding of the subject. Assessment Testing of the knowledge base (1-5) is through assessed coursework which includes; written assignments, tasks undertaken under examination conditions, and by the achievement of the required NMC proficiencies and E.U. directives. 12 B Intellectual Skills B Intellectual Skills Teaching/learning methods and strategies On successful completion of the Intellectual skills (1-5) are developed programme the student will be able to: through the use of problem solving scenarios and other activities that facilitate clinical decision making and evaluation of practice issues. The 1. Integrate theory with midwifery integration of theory with practice is by practice the use of reflective and reflexive approaches in both the University and 2. Develop an enquiring, analytical practice settings e.g. use of the reflective and creative approach to all portfolio. aspects of midwifery care. Assessment 3. Utilise independent judgement, critical self- awareness and reflective and reflexive practice. 4. Apply appropriate sources of evidence and information technology to inform midwifery theory and practice. 5. Develop the skills of critical analysis, reasoning and problem solving to enhance practice A variety of assessment methods are employed, including OSCE’s, (objective structured clinical examinations), written assignments and exams. Students will undertake a dissertation focussed on a service improvement issue and this will enable them to demonstrate creativity and synthesis of relevant information. 13 C Subject, Professional and Practical Skills C Subject/Professional/Practical Skills Teaching/learning methods and On successful completion of the programme the student will be able to: strategies Teaching and learning takes place in a variety of forms across all modules. 1. Provide seamless, woman-centred Practical sessions in a skills laboratory care and respond to the needs of are reinforced in the practice placement the woman, her newborn and the family. by triggers and work based learning sessions to help students reflect on their 2. Analyse critical knowledge of placement experiences. physiological, psychological and pathological factors which influence the wellbeing of the The students also build on their prior women and their families and experiences as they revisit their safely apply this knowledge in midwifery placements every year, and midwifery practice additionally have the opportunity of 3. Demonstrate the ability to critically placements in related specialist practice evaluate maternity care provision areas such as Gynaecology, Day by themselves and others Assessment Units, Children’s Centres, including Sure Start. In addition, there is 4. Communicate effectively, both an elective placement opportunity where orally and in writing with women students can arrange a placement to and their families throughout the further explore midwifery practices within childbearing process a national / international context. 5. Promote an effective interprofessional and multi-agency Students will also care for a small approach to the provision of caseload of women where they will midwifery care identify and provide care for them during the antenatal, intrapartum and postnatal 6. Recognise and effectively periods. undertake a range of management options for women and their newborn when there are complex needs / complications Throughout the programme, students are encouraged to undertake independent 7. Apply the principles and practice reading both to supplement and of effective medicines consolidate what is being learned and to management broaden their individual knowledge and understanding of the subject 8. Demonstrate an awareness and understanding of their professional obligations as a registered 14 midwife. Assessment Skills (1 - 7) are primarily assessed using the practice document, which includes grading of clinical practice grids for each year of the programme. Additionally skills (2, 3 and 5) are assessed using the OSCE (Objective Structured Clinical Examination.) 15 D Transferable Skills and other attributes D Transferable skills and other attributes On successful completion of the programme the student will be able to: Teaching/learning methods and strategies The transferable skills (1 – 10) are inherent within the modules. Skill 2 is 1. Actively participate in clinical particularly addressed in the shared decision making by taking a module Evidence Based Practice in problem solving approach Nursing and Midwifery. Skills 3 and 7 are addressed in the shared module 2. Demonstrate skills in research and Communication in a Diverse World. A variety of teaching/ learning strategies critical appraisal of sources of evidence in order to optimise are used as identified in the specific clinical effectiveness module specifications. 3. Demonstrate the ability to integrate interpersonal skills and partnership working to create an environment which facilitates effective relationships with the woman, her family and other members of the interprofessional team. Skill 4 is addressed every year through the professional practice modules. Assessment Numeracy is assessed on a yearly basis 4. Apply numeracy concepts within as part of the required proficiencies in the the context of midwifery practice in practice documentation. The students order to provide therapeutic are given a Numeracy workbook and interventions additionally, they undertake an online numeracy test requiring a specific 5. Achieve information technology skills to support learning and percentage to pass. In order for them to practice achieve their drug calculations proficiency they must take evidence of 6. Work effectively within a team their online mark to their mentor and complete a drug calculation in practice in 7. Demonstrate the ability to order for them to have this proficiency accommodate diversity in signed off. collaborative working 8. Demonstrate personal leadership skills, including time management, prioritisation of workload, the Opportunities to develop transferable 16 ability to self evaluate and the ability to organise others 9. Demonstrate skills of reflective writing 10. Incorporate ethical principles to inform learning and practice skills will be evident throughout the programme and activities that assess the competence of the students will be visible through formative and summative assessment within modules e.g. on-line patchwork assessment, case study and reflective portfolio. Assessment regulations -The NMC requirements for the programme are as follows: All outcomes within a progression point period (for example an academic year) have to be achieved and confirmed within 12 weeks of entering the next academic level. (Standard 15) All assessments must be completed and have been passed prior to successful completion of the programme Full-time delivery should be no less than 3 years and each year shall contain 45 programmed weeks. Delivery is to be completed in not more than 5 years including interruptions. For the 78 week programme, the programme shall be not less than 78 weeks with delivery completed in not more than 2 years and 6 months(Standard 10) Clinical practice must be graded and be counted as part of the academic award (Standard 15) In order to transfer programmes, students need to meet the University criteria. BRIEF OVERVIEW OF THE MODULES CONTRIBUTING TO THE PROGRAMME Communication in a diverse world This is a shared module with all nursing and midwifery students. The essence of this module will be the facilitation of communication skills and self-awareness appropriate to meet the needs of a diverse society. Fundamentals of midwifery care This module introduces the students to fundamental midwifery theory and will enable the students to build and develop their midwifery knowledge with application to Practice which will be further enhanced in the Introducing Midwifery practice module. 17 Introducing Midwifery Practice In this module, the students will be introduced to fundamental midwifery practice skills and they will engage with a range of clinical opportunities that will enable them to achieve the prescribed proficiencies required by the first progression point. An element of the assessment of this module will be graded and this has been developed from the professional requirement to grade clinical practice (NMC 2009) as already discussed in this document. Professional Development of Midwifery This module will focus on the factors influencing the development of the profession whilst acknowledging the value of inter-professional working. In this module the students will also gain an understanding of the current national and international government policy drivers for maternity care. The Purpose, Scope and Context of Interprofessional Collaboration This module will further enhance partnership working and a commitment to work effectively within and across professional boundaries. This module is shared across the undergraduate provision within the School of Health and Social Care. As the title of the module suggests, the syllabus covers a range of interprofessional issues including equal opportunities, service user and carer perspectives and communicating and working in partnership with other professionals Complexities of Midwifery Care This module will respond to the current challenges midwives face supporting women with medical/obstetric problems. This module also takes into consideration the socio-psychological dimension and a family wide perspective Developing Midwifery Practice This module, the second of the three 40 credit practice modules, will build on the fundamental clinical skills and competencies acquired by the students in their first year. Again, in this module, an element of the assessment of the module will be graded. The synergy between the aforementioned modules will facilitate the student midwives’ development of more complex skills. 18 Evidence based practice for Nursing and Midwifery This module is part of a suite of modules designed to facilitate nursing and midwifery students’ understanding, and use of, sources of evidence that may inform and challenge professional practice. Rather than designing the standard type of research module that would equip students with a fundamental understanding of the research process and critiquing skills, this innovative module takes a wider perspective. It promotes the importance of students’ understanding the need for health service improvement through the implementation of evidence-based practices. Thus students will attain the necessary knowledge, understanding and skills to appraise a wide range of sources of evidence that may inform practice. Grounding this module in the reality of practice has the potential to make it more meaningful for students than the standard type of research module. Exploring Quality Practice for Interprofessional / Inter-agency Collaboration This module continues some of the themes developed in the first inter-professional module. It also explores international, national and local policies affecting intraagency collaboration in the light of the changing landscape of health and social care provision. Meeting Contemporary Challenges in Midwifery This module builds on the policy issues already covered in the year 1 module Professional Development of Midwifery. It also explores the provision of current services both within and out of the NHS including particular political visions (Oakley 2009). Therefore in this module, students will develop an understanding of a range of management styles and leadership roles. Midwives are professional practitioners and as such are required to maintain professional competence and public confidence at all times. Therefore legal, professional and ethical issues are also explicit in this module. Consolidating Midwifery Practice This module will build on the midwifery practice skills developed in the Years 1 and 2 practice modules. In this module the students will acquire the skills and proficiencies to equip them for practice as registered midwives and the grading of practice assessment centres on care for a woman in their caseload. Service user involvement in this assessment is an innovation planned for the new curriculum Nursing and Midwifery Dissertation 19 This module is designed to enable students to critically evaluate evidence for the purpose of instigating change in practice (NHS 2006). Engaging with evidence in this way makes the project dynamic in nature and highlights both the opportunities and the barriers inherent in change management processes. Commensurate with the ‘Evidence Based Practice for Nursing and Midwifery’ module, it is acknowledged that the development of critical appraisal skills is integral to the process. It is envisaged that the common principles of the module will be delivered through the medium of shared learning. The professional and subject specific context of the module will be through independent study supported by appropriate supervision. Course overview. Year one Acad Week No (inc) Overview of Theory Overview of Practice 8 Induction Week 9-11 Communication in a Diverse World (module) 12-21 Fundamentals of Midwifery Care (module) Introducing Midwifery Practice (module) 19 22-23 Annual Leave 2 weeks 24-30 Introducing Midwifery Practice (module) First practice period (6 weeks) –birth unit and community experience. 1 Work Based Learning Day 20 31-33 Professional Development of Midwifery (module) 34 Reading week 35-37 Fundamentals of Midwifery Care (module) Professional Development of Midwifery (module) 38 Annual Leave one week 39 Reading week 40-1 Second practice period (14 weeks) birth unit and community experience. Introducing Midwifery Practice (module) 2-5 Annual Leave 4 weeks 6-7 Second year Please note some students may have to move zones to obtain birth unit experience. 2 Work Based Learning Days will be scheduled during this period. During this placement period GRADING OF PRACTICE will take place and this will be arranged by the student in agreement with the Sign-off Mentor. Study period. Please refer to your module handbooks to confirm submission dates 21 How your degree will be calculated Due to variations between the total credit requirements for different degree with honours awards, a single University-wide formula, which uses the same number of credits for all students, is used to calculate degree classifications. This is unless a professional or statutory body requires the use of a different method. Your Programme Leader will be able to advise you if this is the case for your award. The key features of the formula are: Only the marks for 100 credits at level 3 and 100 credits at level 2 (or other level 3 credits) are included. Marks for the 100 level 3 credits are weighted three times those at level 2. Marks used are the best overall module marks a student has achieved. Please see the UWE website for more information: http://www1.uwe.ac.uk/students/academicadvice/degreeclassification Non-standard calculations If the total credit value of the best module marks at level 3 add up to more than 100, only part of the credit for the module with the lowest mark will be used in the level 3 calculation. The remaining credit will be carried over to the level 2 set of marks and treated as a level 2 module. The partial module credit and the mark may then be included in the best overall marks if it falls into the best 100 credits at level 2. For example: A student has 5 x 30 credit modules at Level 3 and 3 x 30 credit modules at Level 2. Level 3 marks (ranked in order – highest first) Credit size Running total (100 max) 69% Module A – 30 credits 30 credits 58.1% Module B 30 credits 60 credits 56% Module C – 30 credits 90 credits 52.2% Module D – 30 credits 100 credits (10 of the 30 credits are used in the level 3 calculation) 22 48.8% Module E – 30 credits Not included in the calculation as this is the lowest mark Level 2 marks (ranked in order – highest first) Credit size Running total (100 max) 65% Module F – 30 credits 30 60.9% Module G – 30 credits 60 55.3% Module H – 30 credits 90 52.2% (level 3 module, moved down to level 2) Module D – 30 credits 100 (10 of the 30 credits are used in the level 2 calculation) In exceptional circumstances, for example, where some of module marks are not expressed as percentages, or where the credit total includes modules awarded as Accredited Learning, the total credits counting towards the classification at one or both levels may be lower than 100 credits. In these circumstances the degree will be calculated on the basis of all available marks at each level. Foundation Degree A Foundation degree contributes 240 credits towards the total of 360 for an honours degree, and students take the remaining 120 credits in year 3. The classification for students who progress from a Foundation Degree to the final year of an honours degree will be calculated based only on the marks achieved in that year. In the Calculation, the best overall module marks for 100 credits achieved at level 3 are weighted there times those of the remaining 20 credits. 23 3. Additional Information link to placement handbook Placement Information Much of the information you will require for working in the practice setting is available via the Student Practice Information Document (SPID) and the Practice Support Net http://hsc.uwe.ac.uk/net/student/Default.aspx?pageid=327 It is important that you refer to this prior to practice Additional information as listed below will be found in the placements handbook. Practice hours Shift patterns Bank holidays / Annual leave Adverse weather (snow / Flooding) Private study days Duty Rosters Can I go early? Supernumary status in clinical placement Meal breaks Working with your mentor Timesheets Making up hours Absence due to: Sickness Compassionate leave – Jury service – Military reserve personnel – Authorised absence – Interview days What counts as practice hours? Pregnancy, Maternity Leave and Maternity Support Award (Paternity Leave) Accommodation whilst on Placement Accidents in clinical practice 24 Work based learning days During practice placements the link between theory and practice will be enhanced by prescribed work based learning days in your zoned (practice) area on certain weeks of the academic year. These sessions will use your clinical experience as a trigger to review and consolidate your learning, and as a springboard for further exploration and discovery. The philosophy that underpins the curriculum not only recognises the importance of a programme of preparation that is practice centred, but acknowledges the need to promote the integration of theory and practice for the achievement of professional competence. The work based learning days aim at strengthening this theory practice integration in a number of ways: 1. expanding the opportunity for students to develop independence, autonomy, flexibility and reflective thinking; 2. using real life scenarios to facilitate student learning; 3. accessing sources of information to support midwifery practice as it is delivered; The focus of the Work Based Learning Days will be on incidents emerging from practice. These could range from broad situations such as advocacy and empowerment to specific case studies. What is important is they are deemed appropriate to the learning outcomes of the Professional Practice module the student is undertaking. Since these Work Based Learning Days occur within each practice placement experience, more information about the dates and organisation of these days will be contained within the relevant practice module handbook. Attendance at work based learning days is compulsory and absence requires you to contact your Academic Personal Tutor with an explanation. . 25 Brief description of practice allocations. Throughout the three years, you will be provided with practice placements that facilitate your development of midwifery skills, knowledge and values and the achievement of the learning outcomes as outlined in each year of the Student assessment document Whilst recognising that health care is increasing being delivered in Community settings. You will have the opportunity to deliver midwifery care in the home, birth units and in hospital. A varied number of learning opportunities will therefore be possible during these allocations to meet the required learning outcomes within different care settings. In order to provide you with this variation, midwifery students at UWE are expected to travel to placements areas across the region. Unfortunately, it is not possible to guarantee all placements will be geographically close to where you live. Students allocated a placement for which travel or accommodation may be necessary are advised to make an appointment with a student advisor to discuss their eligibility for claiming travel and accommodation costs. Placements are allocated through the Professional Practice Office and each placement must meet the NMC requirements of the programme. Students are not able to request certain placement areas. If a student has a personal reason to not be allocated a particular placement area/ speciality (for example, family member is a service user in that area), then they can do so through negotiation with their programme manager. Because of the complexity of placements and the need to ensure transparency, tracking and equity, students will not be allowed to contact and/or organise their own placements (unless undertaking an elective experience). This includes altering allocated shifts. Midwifery students are expected to follow the shift pattern of their mentor to include; early, late, night, weekend and bank holiday shifts. Requests for shift changes must be made to the appropriate co-ordinating midwife and will only be granted in exceptional circumstances. Students are not allowed to request shift changes to facilitate routine social or family commitments. Inappropriate requests will be forwarded to the programme lead. Retrieval of practice If you fail the final placement of each year, a retrieval placement will be considered at the award board. Retrieval must occur in the first 12 weeks of the subsequent year in order to meet NMC requirements. If this is not possible, the student needs to step off the programme and return at a later date, if appropriate. 26 Please note, a retrieval placement is not an automatic right and the decision is made by the award board, not a member of the midwifery programme team. Retrieval placements are arranged through the Professional Practice Office. Retrieval placements are usually for a minimum of 5 weeks, but may be longer, depending on individual student circumstances. The academic year dates are published on the University website, see: http://www1.uwe.ac.uk/aboutus/termdates/2012-13termdates.aspx Theory The theory element of the programme is an NMC requirement and you should be spending 40- 50% of allocated programme hours engaged in theoretical learning. Attendance at timetabled sessions is, therefore, essential, and expected, and for this reason will be monitored closely by the programme lead and LME. A high level of attendance demonstrates professionalism and good character. Regular non-attendance may invoke professional suitability procedures. Clinical Skills Sessions All students must attend clinical skills sessions in appropriate dress and footwear for the skill being undertaken. This is particularly important for Manual Handling and Basic Life Support sessions for health and Safety reasons. Students who arrive more than 10 minutes late or dressed inappropriately will be asked to leave. Nonattendance at clinical skills sessions will adversely affect your ability to go into placement Monitoring Of Absence Where non-attendance is giving concern students will, in the first instance, discuss the nature of such absence with their Academic Personal Tutor and, thereafter, with the Programme Manager and/or the LME. Students who do not advise the faculty of the reason for their absence and/ or fail to submit medical certificates, when appropriate, may have their bursary suspended, and be discontinued from the programme. Failure to meet the attendance criteria for both theory and practice elements of the course may result in registration delay or being unable to register as a qualified midwife. You must make up theory missed through self-directed activity. Clinical skills session make up will be organised in negotiation with the module leader. All absence retrieval activities must be reported to your APT and recorded. 27 PROGRAMME SPECIFIC REGULATIONS RELATING TO WORKING TO THE CODE : STANDARDS OF CONDUCT, PERFORMANCE AND ETHICS FOR NURSES AND MIDWIVES (2008) The Midwifery programme leads to eligibility for professional registration with the Nursing and Midwifery Council (NMC) and, as such, requires a sensitive, reliable and responsible approach towards others. The student is required to demonstrate these qualities in general attitude and behaviour towards other students, staff of the University and in the practice areas towards staff, clients, carers and the general public. Students are obligated to learn, accept and demonstrate the responsibility and accountability increasingly demanded of practitioners in health and social care services. Any student who fails to demonstrate appropriate standards of behaviour, either at University or on practice placement, may be deemed to be unsuitable to enter the profession if he/she:-. 1 Has failed to meet the criteria of The Code : Standards of Conduct, Performance and Ethics for Nurses and Midwives (NMC 2008). Students are required to comply with ‘Guidance on professional conduct for nursing and midwifery students’ (NMC 2009). 2 Is deemed to be guilty of an act, practice or breach of conduct that contravenes the Nursing and Midwifery Code of Professional Ethics that may involve a patient, client, member of staff or other person with whom the student is in contact and/or 3 Engages in behaviour, which is deemed to bring the profession into disrepute and/or engages in behaviour which fails to demonstrate an appropriate standard of professionalism, either at University or on practice placement. Falsification of documentation is one such behaviour that falls into this category. Unsuitability will be judged from the evidence:1 Reports from University staff and/or practice mentors and/or practice staff. 2 Failure in the Assessment of Practice documentation. 3 Academic censure relating to plagiarism/cheating and or criminal conviction. In any of the above criteria a student may be asked to withdraw from the programme at any stage and will not be eligible for the BSc (Hons) Midwifery Award with registration. The Award Board will ratify the decision. 28 Returning students. The NMC requires that students self - declare their good character and health annually. In order for this to be accomplished, all nursing and midwifery students must therefore complete the following declaration: □ I have read and understood understand the NMC guidance available here Good Health and Good Character for student nurses and midwives. □ I understand that I must notify the University and the Programme Manager of any criminal warnings, cautions, reprimands or a warning recorded on police central records, which includes both ‘spent’ and ‘unspent’ convictions since the last Disclosure Barring Service (DBS) check (formerly Criminal Records Bureau CRB) or declaration and complete a DBS self-assessment form available through this link. http://hsc.uwe.ac.uk/net/student/disclosurebarring-service-dbs.aspx □ I have not received any criminal warnings, cautions, reprimands or a warning recorded on police central records, since the last DBS check (formerly Criminal Records Bureau CRB) or self-declaration. (Do not include motoring offences where you receive a fixed penalty unless it lead to your disqualification) □ I declare that my health and character are sufficiently good to enable me to practise safely and effectively and that all of the above information is a true and accurate record Good health is necessary to undertake practice as a nurse or a midwife. Good health means that a person must be capable of safe practice. Good character is also important as nurses and midwives must be honest and trustworthy. Good character is based on a person’s conduct, behaviour and attitude. It also takes account of any convictions and cautions that are not considered to be compatible with 29 professional registration and that might bring the profession into disrepute. A person’s character must be sufficiently good for them to be capable of safe and effective practice without supervision. It is important that you are aware that your behaviour and conduct, both during your programme and in your personal life, including on any social networks you are part of such as Facebook, may have an impact on: o your fitness to practise o your ability to complete your programme o the willingness of the university to sign the declaration of good health and good character for you to become a registered nurse or midwife. □ I will practice in accordance with the NMC Guidance on professional conduct for nursing and midwifery students.pdf □ I have read and agree to abide by the principles contained within the Faculty of Health and Applied Sciences UWE student conduct policy Please note. A false declaration to the above, subsequently discovered, in itself may lead to a student being investigated through UWE Professional Suitability and Professional Conduct Policy. This could, in turn, lead to discontinuation from the relevant programme. Please note that the on-line declaration form for Good Health and Good Character is contained within the ARC system. Any student who does not complete their declaration will subsequently not be allowed to access their placement details through ARC. As a result the student will therefore not be allowed to attend placement. http://hsc.uwe.ac.uk/net/student/disclosure-barring-service-dbs.aspx The European Union and Article 40 (training of midwives) of Directive 2005/36/EU from the NMC standards for student midwives Advising of pregnant women, involving at least 100 prenatal examinations supervision and care of at least 40 women in labour the student should personally carry out at least 40 deliveries; where this number cannot be reached owing to the lack of available women in labour, it may be 30 reduced to a minimum of 30, provided that the student participates actively in 20 further deliveries Active participation with breech deliveries. Where this is not possible because of lack of breech deliveries practice may be in a simulated situation Performance of episiotomy and initiation into suturing. Initiation shall include theoretical instruction and clinical practice. The practice of suturing includes suturing of the wound following an episiotomy and a simple perineal laceration. This may be in a simulated situation if absolutely necessary supervision and care of 40 women at risk in pregnancy, or labour or postnatal period supervision and care (including examination) of at least 100 postnatal women and healthy newborn infants observation and care of the newborn requiring special care including those born pre-term, post-term, underweight or ill care of women with pathological conditions in the fields of gynaecology and obstetrics Initiation into care in the field of medicine and surgery. Initiation shall include theoretical instruction and clinical practice. GUIDELINES FOR COMPLETION OF CLINICAL EXPERIENCE REGISTERS At the completion of the programme, the LME must sign a declaration that you have met the standards required of the programme, in order to be admitted to the NMC professional register. To facilitate this, you must ensure that you keep copies of evidence that you have completed EU directives, competencies and timesheets. Your APT will monitor your progress and record evidence of clinical experience throughout the programme. Your clinical register, together with your on-going clinical assessments and timesheets provides this evidence. As a professional midwife, part of your responsibility will be to keep accurate, contemporaneous records. For this reason most of the record keeping relating to your clinical experience is your own responsibility and, with the exception of vaginal examinations (VE’s), does not require countersigning by a midwife. However, suspected dishonest practice will be investigated. A midwife is required to sign VE’s, so that their accuracy can be authenticated and a platform for discussion is provided. When you are working in the 31 delivery suite, you should ask your personal tutor to look at these every time you have an appointment. By the time you have performed 40 VE’s, it is hoped that competency can be demonstrated. Should proficiency not be reached, you will be required to perform more, until competence is demonstrated. VE’s should be performed on women for whom you are providing care. For all other clinical experience, your own documentation will be sufficient proof of achievement. PLEASE REMEMBER TO MAINTAIN CONFIDENTIALITY. A more detailed explanation of the requirements to be recorded can be found below. It is useful for your transcript of training if you continue to record additional experience, especially of deliveries and of women at risk, even when you have fulfilled the NMC registration criteria. For simplifying the recognition that all the required clinical experience has been completed, please record or highlight items that you witness in green, all “at risk” cases, in red and the remainder in black. So please record all experiences 100 Antenatal Examinations These should include advising mothers and performing both a general examination and abdominal palpation. The 100 should include women at all stages of pregnancy. One woman can be examined on several occasions as long as the examinations are made on different days. By seeing the same woman on several occasions the changes in pregnancy can be more clearly observed, especially if a week or more elapses between each examination. Witnessed Births These should be normal vaginal births and includes the delivery of the placenta and membranes. You are advised to witness some before facilitating births personally and you should have been involved in the care of the mother beforehand. The number that you witness before conducting deliveries yourself will depend upon the judgement of your midwifery mentor. Various factors will be considered, such as your progress and the suitability of the mother and her labour for a learner’s first delivery. Supervision and Care of at Least 40 Women in Labour These can include any woman for whom you care for a reasonable length of time during her labour. The 40 personal deliveries should all be conducted on mothers for whom you have provided care. Conduct 40 Personal Deliveries 32 Students are required to conduct 40 deliveries during the course of their training. Ideally, the pregnancy should be at term (from 37 weeks) and the placenta and membranes should also be delivered. Students should strive for this, but record all deliveries from 24 weeks viability and those which require the manual removal of an adherent placenta, following the employment of midwifery skills to facilitate delivery and ensure the safety of the mother. Stillbirths can be recorded only where midwifery skills have been utilised to facilitate delivery and may be counted only where the student has been unable to achieve 40 live births. If medical aid has to be sought in order to complete the delivery of the baby, the delivery may no longer be counted as a personal birth. However, the experience can go toward those mothers that you care for who are at risk. You should examine all the newborn babies of the mothers you deliver. Performance of Episiotomies and Suturing Initiation into the performance of episiotomies and perineal suturing must include both theoretical instruction and clinical practice. Suturing practice should include repair of both episiotomies and simple perineal lacerations. This may be in a simulated situation if absolutely necessary. Supervision and the Care of 40 Women at Risk in Pregnancy, Labour or the Postnatal Period In order to ensure a balance this should be divided into: 10 women at risk antenatally, 10 mothers at risk in labour, 10 deliveries in which the second or third stage is abnormal and 10 mothers who have a postnatal complication. The EU directives require a total of 40 women in these categories to be looked after but for your future transcript of training, please record all such experiences. The 10 mothers whose deliveries are complicated in the second or third stage should be in addition to the other 10 women who are at risk in labour. Some of the mothers should have pathological conditions. It does not matter how early in pregnancy the care is given. With antenatal and postnatal mothers, evidence of continuity of care is desirable. The NMC require you to actively participate in vaginal breech deliveries. Please take the chance to be involved whenever it occurs. If no opportunity arises, simulated practice can be undertaken instead. Twin deliveries are not a specific requirement but are also a useful adjunct to your experience. At risk labours should include any mother in whom the normal physiology of labour is altered. These therefore include augmentation and induction of labour by any means except the use of prostaglandins alone. Epidurals can also interfere with normal progress. Posterior positions in labour can be included in the complicated labours. If any mother in a risk category delivers 33 normally and you conduct the delivery, the experience can be counted as both a personal delivery and as the care of a woman at risk in labour. The Neonate at Delivery You are required to be proficient in fulfilling the midwife’s role in relation to the healthy baby at birth. You should be capable of initiating and maintaining respiration in the mildly respiratory depressed baby for whom paediatric assistance is not being sought. Checking resuscitation equipment and assisting the paediatrician with a compromised baby is valuable experience which you should endeavour to acquire. 100 Postnatal Examinations Supervision and care of at least 100 postnatal women: This includes the examination of both the mothers and their healthy newborn babies, encompassing all aspects of holistic care. Each mother and baby should only be counted once. If possible you should follow up postnatal women and their newborns for at least three days and, where the opportunity exists, for a full 28 days as the midwife may be responsible for care up until that time. Attendance at Clinics You should ask your community midwife to arrange these. It is suggested that a minimum of one family planning and one child health clinic should be observed. The midwife may be able to suggest other appropriate observational visits to enhance your understanding of the health needs of the local child bearing population. Administration of Drugs As per the drugs policy 34 Faculty of Health and Applied Life Sciences DEPARTMENT OF NURSING AND MIDWIFERY Policy for UWE 3 year Midwifery Students The qualified midwife remains accountable for the correct administration of the drugs as prescribed on all occasions (NMC Midwives Rules and Standards, 2004). The 3 year BSc (Hons) Midwifery students are not registered nurses and therefore they will need active involvement in drug administration from their first clinical placement. They will be expected to sit a numeracy test and achieve a pass mark of 80% during the initial 20 weeks of the programme. They will also need to meet the drug/numeric assessment requirements in the clinical assessment documentation for years 1, 2 and 3. This will not be achievable unless they are actively participating in drug administration. In year 2 and 3 students will also undergo a written assessment in preparation of practice registration. This means: The student should gain substantial experience of drug administration in the midwifery practice environment. The student should be fully aware of the implications of the drugs in relation to midwifery The student should also be aware of and comply with local policies and the patient group directives. Please note that student midwives can be involved with the administration of drugs covered under MIDWIVES EXEMPTIONS (not including controlled drugs) only if they are supervised by a SIGN-OFF MENTOR. It is an expectation that students will participate in the administration of drugs including situations when one or two trained persons are required to check the drug prior to administration. In these circumstances students will be observers for the checking process. However, they should be encouraged to be the administrator of the drug under direct supervision provided they have received the appropriate training as to use, dosage and methods of administration (NMC 2007 Rule 17 pg 33) (NOT INCLUDING CONTROLLED DRUGS ADMINSTERED UNDER MIDWIVES EXEMPTIONS). As stated previously, students are not permitted to administer medicines under a PGD but can be involved with the administration of drugs covered under MIDWIVES EXEMPTIONS (not including controlled drugs) and a drug prescription written by a doctor but only if supervised by a Sign-off Mentor. Drug administration should include:35 IV Fluids. IV Additives. Blood and blood products. Injections (IV drugs = simulation) Drugs administered to neonates. Epidural top-up. Two trained midwives/nurses are required to check the above list; however, one trained midwife/nurse may be substituted by a pre-registration student midwife who is in the final year of the programme and has: Successfully passed the numeracy test. Attended all the pharmacology lectures for year 1 and 2. Achieved all the skills related to the administration of drugs in the practice assessment document for year 3. This will always be at the discretion of the ward manager/senior midwife on duty. At all times the student will remain under the supervision of a registered midwife, who remains accountable for the correct administration of the drug as prescribed on these occasions. At no stage during the programme is it expected that 3 year student midwives will administer drugs without direct supervision. References NMC (2012) Midwives Rules and Standards. NMC. London NMC (2007) Standards for Medicines Management. NMC. London NMC (2009) Standards for Pre-registration Midwifery Education. NMC. London NMC Circular 05/2009 Supply and/or administration of medicine by student nurses and student midwives in relation to Patient Group Directives (PGD’s) NMC Circular 07/2011 Changes to Midwives Exemptions. NMC. London Issue date: 17 June 2011 36 4. Key Faculty Staff Key faculty Staff Pro-Vice Chancellor and Executive Dean - Helen Langton Head of Department - Sarah Green Sarah.Green@uwe.ac.uk Field specific AHoD - Teresa Shalofsky Field Specific Programme Manager - Geraldine Lucas Practice Placement Office field specific allocation officer - Annie Pearce Roles within the Department of Nursing and Midwifery Head of Nursing and Midwifery: The Head of Nursing and Midwifery has ultimate responsibility for the course curriculum. They are required to keep abreast of strategic and political developments within the health sector, and encourage academics to thread these changes through the curriculum. They work in close partnership with practice colleagues to deliver a high quality educational experience. They maintain an overview on key performance indicators. They support academic staff to deliver the vision of UWE Bristol. Associate Heads of Department: The Associate Head of Department acts as a link between the Head of Department and the academic team, supporting both to deliver high quality education. Associate heads also have responsibility for overseeing projects within the department which enhance learning and teaching and develop the curriculum. Programme Manager: At UWE Bristol the programme manager is a core member of the team. They are responsible for overseeing the quality of the relevant courses. They will work closely with academics and practice colleague to achieve this. An important role of the programme manager is to support their team to design and deliver innovative and creative curriculums. This can be achieved in a number of ways, including the use of technology and service users. Programme managers take an active role in the revalidation process ensuring that students are fit to practice upon qualification. Programme managers will also work in close collaboration with academic personal tutors to ensure that students are being supported, and receive guidance with their training. The programme manager in midwifery is supported by a co programme manager for quality of placements . Academic Personal Tutor (APT): 37 All UWE Bristol students will be allocated to a personal tutor at the start of their programme. The tutor is an academic member of the team. The student will be given opportunities to meet with their academic personal tutor during the course of their studies. There will be opportunities to discuss academic and pastoral support needs. The tutor will be able to sign post the student to additional support needs, should this be needed. The academic support tutor will be keen to support the student to achieve their maximum potential whilst studying at UWE. Practice Associate lecturer in midwifery (PALM) These lecturers spend a proportion of their time in clinical practice supporting students and mentors. They work alongside students who are not achieving and have been referred or failed in practice. PALMS can support the student and mentor with development of action plans, and how students can achieve formulated goals. If students have additional health needs, PALMS s can provide advice, support and referral. WHO’S WHO IN THE DEPARTMENT OF NURSING AND MIDWIFERY Midwifery Team - Roles and Responsibilities, Pre-registration Programmes Teresa Shalofsky Geraldine Lucas Sue Davis Jo Jones Caroline Rutter Jenny Hall Andrew Yelland Sian Mclaughin Rona Early Lead Midwife for Education and Professional Lead PALM: Gloucestershire NHS Trust Programme Manager BSc (Hons) 3yr Midwifery Senior Lecturer in Midwifery PALM: UHB NHS Foundation Trust Co Programme Manager: Senior Lecturer in Midwifery Module Leader: Preparation of Supervisors of Midwives PALM: Gloucestershire NHS Trust Admissions Tutor Senior Lecturer in Midwifery Module Leader: Professional Development in Midwifery PALM: Gloucestershire NHS Trust Senior Lecturer in Midwifery Module Leader: Introducing Midwifery Practice PALM: GWH NHS Foundation Trust Senior Lecturer in Midwifery Module Leader: Fundamentals in Midwifery Care PALM: North Bristol NHS Trust Midwifery Lecturer Module Leader: Complexities of Midwifery Care PALM: UHB NHS Foundation Trust Midwifery Lecturer Module leader: Developing Midwifery practice PALM: UHB NHS Foundation Trust Senior Lecturer in Midwifery Module leader: Meeting Contemporary 38 Mary Mitchell Marian Bailey Jane Pilston Gillian Ottley Challenges in Midwifery Co-module leader: Evidence based Practice For Nursing and Midwifery PALM: North Bristol NHS Trust Senior Lecturer in Midwifery Module Leader :Nursing and Midwifery Dissertation PALM: RUH Bath NHS Trust Senior Lecturer in Midwifery Module Leader: Consolidating Midwifery Practice PALM: North Bristol NHS Trust Lecturer in midwifery (Secondment) PALM: RUH Bath NHS Trust Midwifery Lecturer PALM: GWH NHS Foundation Trust All the above Midwifery Lecturers will have input into your course. Only the responsibilities of the Midwife Lecturers relevant to your course have been included. 5. Communication The main communication channel used by the University and the Faculty is the UWE student portal, myUWE. The myUWE link appears at the top of the University staff and student intranet home page alongside that of the library and gives you access to the portal, where much of the information relevant to you will appear, including important announcements. myUWE gives you access to a wide range of course information, including links to Blackboard for modules you are currently studying. Blackboard provides the main communication channel for module specific information and should be checked regularly for new content and announcements. Also from myUWE you can access your UWE student email account, which you are expected to check regularly (at least twice a week) as this is the email address that the University will use to contact you. If you do not activate this account, or chose to automatically forward emails to a different email account, then the University will not be responsible if you miss important information such as details about classes, assessments, examinations, fees, registration etc. Please see http://info.uwe.ac.uk/myUWE/guidance/ for further information on all aspects of your myUWE portal. 6. Regulations/Policies 39 The University regulations are designed to ensure consistency and equity for students and to provide clarity in how they will be treated by the University in any given situation; Regulations: http://www1.uwe.ac.uk/students/academicadvice/assessments/regulationsandproced ures.aspx Assessment Offences In order to ensure that all students are assessed fairly and equitably, it is important that markers are able to be sure it is your own work which is being assessed and that all your assessed work is done within the University rules and regulations. If a marker or invigilator believes that you have committed an assessment offence this will be reported and the allegation will have to be investigated. The University take the committing of assessment offences very seriously. Action is always taken to investigate and follow through any such cases that are reported. The process and consequences can be found within the UWE Academic Regulations. An assessment offence is defined by the University as ‘Passing off the work of others as one’s own including copying (reproducing or imitating), cheating, collusion (agreement to deceive, using words or ideas of colleagues or other students and passing them off as your own), plagiarism (stealing someone’s words or ideas and passing them off as your own) and other breaches of assessment or other examination regulations or procedures. Cheating, collusion and plagiarism are the use of unfair means of presenting work for assessment or of aiding another student to do so. Plagiarism – Demonstrating that you have read a wide range of material (books, journals or other sources) in writing a piece of coursework is essential, but so is ensuring that you acknowledge that work properly through correct referencing i.e. the naming of authors/sources and the use of paraphrasing, quotation marks or indented paragraphs. Collusion – You may be asked to work with other students on a project, in class or analysing data, it is essential that any work you hand in for assessment purposes is written up by you on an individual basis. The text and diagrams / pictures etc. you use must be your own. You must be particularly careful if you are sharing a computer with another student or passing information between yourself and others in an electronic format such as by disc or email that you do not use someone else’s words – or that they use your words. Non-compliance – it is important that you follow the instructions given to you by staff and adhere to the regulations of the University. For example, non-compliance could 40 include taking unauthorised papers or items into an examination room or falsely claiming extenuating circumstances or late work. http://www1.uwe.ac.uk/students/academicadvice/assessments/assessmentoffences. aspx In addition to the academic regulations, students should pay particular attention to the IT Acceptable Use Policy as this defines what you can or cannot do for the protection of systems and of individual users. Word count policy http://www1.uwe.ac.uk/aboutus/policies Referencing guide Referencing is the technique used to direct readers of a piece of written work to the sources of information that have been used in the preparation of the written work. If you wish to refer to something you have read you MUST give a reference for this material. The University Library provides advice on managing references, see: http://www1.uwe.ac.uk/students/studysupport/studyskills/referencing.aspx Marking criteria Year one Midwifery Modules HASS Marking Guidance 2012-13 (version 180712).pdf Feedback You are asked to pay particular attention to assessment dates and ensure you check with your academic team if you are unsure when assessments are due. Students are expected to be available during these periods and absence from scheduled assessments may have a significant impact on your studies. Please take care to avoid these dates when planning any holidays. Health and Safety Mandatory health and safety sessions are programmed through the course there is an expectation that you will attend unless you have exceptional circumstances. Dress Code and Uniform Policy 2011 This policy should be read in conjunction with: 41 UWE Academic and Professional Standards of Behaviour Guide http://hsc.uwe.ac.uk/net/student/academicandprofessionalstandardsandbehaviour.as px Nursing and Midwifery Council Guidance on Professional Conduct for Nursing and Midwifery Students (NMC, 2009) http://www.nmcuk.org/Documents/Guidance/Guidance-on-professional-conduct-for-nursing-andmidwifery-students.pdf The relevant policy or guidance from the placement provider, as well as local policies pertaining to certain practice areas. This includes Infection Control Policies. As a nursing or midwifery student your conduct is bound by the four principles of the Nursing and Midwifery Code (NMC, 2008). This dress code / uniform policy is intended to help you in your efforts to: Safeguard the health and wellbeing of the public. Maintain clear professional boundaries in the relationships you have with others, especially with vulnerable adults and children. Maintain clear sexual boundaries at all times with the people for whom you provide care, their families and carers. Uphold the reputation of your chosen profession at all times. It is your responsibility to check the uniform requirement when you first make contact with your placement. If uniform is not required, your dress should reflect your professional position and support the development of therapeutic relationships with patients, carers and families. All uniform or non-uniform dress should be safe, hygienic and modest. The list below, gives the some general points on developing and maintaining your professional appearance / identity. Where there are religious or cultural issues that affect adherence to this policy, or you have any other questions about your own appearance/dress not covered in this information, please discuss with your Programme Manager prior to commencing placement. Review Date July 2013 General Appearance All clothes worn whilst on placement should be well laundered and maintained. Whether in uniform or your own clothes your appearance must be modest. Where uniform is not required, jeans; short skirts; shorts; revealing clothing or clothing with slogans which may be considered offensive or provocative, are not permitted. Where 42 make-up or body scents are used these should be discreet. Tattoos should be covered as far as possible. False eye lashes must not be worn. UWE Uniform and Student Identification Student Identification should be worn at all times whilst on placement. Do not wear your UWE Uniform or Student Identification when undertaking work for Bank or Agency. Hair All hair should be clean and worn neatly and should be of a well groomed appearance. Long hair should be securely tied back so that it does not require frequent readjusting. Where hair bands or tiebacks are used they must be discreet. For Infection Control reasons hair-extensions are not appropriate. If you wear your hair / head covered for religious or cultural reasons please refer to the local health organisation’s policy for the correct wearing of headscarves. Beards and moustaches should be clean and neatly clipped. Finger Nails Nails need to be clean, short and undamaged. False nails; nail extensions, nail varnish or decorations are not permitted. Shoes Flat, non-slip, black shoes should be worn. The shoes should cover the whole of the foot including the toes and heels. Footwear should be of a protective material that can be wiped clean and must be in good repair. Students should wear black or flesh toned / neutral coloured tights or socks. Jewellery/Watches Jewellery and wrist watches must not be worn if you are in uniform or when you are performing physical care, however, a plain wedding band is acceptable in 43 most clinical areas. In areas where jewellery is permitted these should be discrete, and consideration should be paid to personal safety (e.g. necklace). If you have pierced ears only one pair of ‘stud’ earrings should be worn. You will be required to cover or remove piercings in certain clinical environments. When travelling to and from as well as during placement When travelling to and from placement, it is preferable to travel in your own clothes and change into your uniform when you arrive. If this is not possible, uniform should be completely covered and worn for the minimum amount of time outside your placement. It is a good idea to purchase a dark (e.g. blue/black) coloured full-length coat or raincoat which will completely cover your uniform whilst travelling. This is particularly useful when undertaking community-based placements It is inadvisable to be seen in public in uniform as members of the public may mistake you for registered staff and seek assistance inappropriate to your status. Wearing your uniform in places such as shops, restaurants and bars whilst offduty, is not only an infection control risk, it may also undermine the idea that you are safeguarding the health and wellbeing of the public. 7. Advice and Support Academic Support is provided through a number of roles and students should seek advice from academic staff on specific matters relating to teaching and learning. 44 Programme Manager – programme related issues, issues impacting on a number of modules within the programme, programme specific activities happening outside modules Module Leader – module related issues, issues that affect that module only Academic personal tutor – broader issues relating to teaching and learning at the University – http://www1.uwe.ac.uk/students/studysupport/academicpersonaltutor Online resources and learning support, together with advice from Library Services on managing references and improving your learning, writing and research skills are available, see: http://www1.uwe.ac.uk/students/studysupport/studyskills.aspx If you need help with a particular mathematical or statistical problem, then just pop along to an espressoMaths session, sit down at the espressoMaths table, and have a chat with one of the staff on duty; this person will be able to provide you with free user-friendly advice concerning your problem see: http://www.cems.uwe.ac.uk/mslc/ The University also provides support to students relating to a range of matters through the Information Points see: http://www1.uwe.ac.uk/students/informationpoints.aspx and specialist advisers. Advice on study-related issues including assessments can be found at http://www1.uwe.ac.uk/students/academicadvice/academicappeals.aspx and http://www1.uwe.ac.uk/students/academicadvice/assessments/extenuatingcircumsta nces.aspx affecting your ability to study Advice on transferring courses, taking time out or withdrawing from study can be found at http://www1.uwe.ac.uk/students/academicadvice/changingdirection.aspx Preparing for your final year? Information can be found at http://www1.uwe.ac.uk/students/inyourfinalyear.aspx Prepare for life after university with advice and support from UWE. http://www1.uwe.ac.uk/students/careersandemployability.aspx Careers advice and guidance before, during and after your studies. Preparing to go on placement whilst at UWE: http://www1.uwe.ac.uk/students/careersandemployability/placements/findingaplacem ent.aspx - Advice on opportunities for placements or finding placements. Explore and practice faith and spirituality at UWE http://www1.uwe.ac.uk/students/healthandwellbeing/faithandspirituality.aspx 45 Tuition fees and information on bursaries and scholarships. http://www1.uwe.ac.uk/students/feesandfunding.aspx Residents’ guides and accommodation options. http://www1.uwe.ac.uk/students/accommodation.aspx Wellbeing advice, from staying healthy to counselling. http://www1.uwe.ac.uk/students/healthandwellbeing.aspx Advice and guidance for international students at UWE. http://www1.uwe.ac.uk/comingtouwe/internationalstudents/internationalstudentsuppo rt.aspx Information on student feedback and surveys. http://www1.uwe.ac.uk/students/studentexperience.aspx Link for information for the student Union and how to become a student representative. http://www.uwesu.org/representation/ Equality and Diversity http://www.uwe.ac.uk/groups/equalityanddiversity/ Preganancy In the event of a student pregnancy a risk assessment will need to be undertaken please inform your personal tutor and programme manager. If in clinical practice the trust will need to complete a risk assessment of practice. Social media The NMC Code of Practice states that registrants must uphold the reputation of the profession in their daily lives and inappropriate behaviour outside of work may be considered potential misconduct. http://www.nmc-uk.org/Nurses-and-midwives/The-code/The-code-in-full/ 8. Insurance Guidelines The University has a range of insurance policies which provide cover to both the University, it’s employees and to students. The following guidelines provide information on the operation of the policies in the context of University activities. If you required further information please contact J Elliott, Insurance and Data Protection Compliance Officer in Financial Services, or click on the following link for the University’s Insurance Guidelines: http://www.uwe.ac.uk/finance/sec/insurance/intranet/docs/InsGuide.pdf 46 Student on University Premises Indemnification of the University The University has arranged insurance which provides indemnity in respect of the University’s legal liabilities, which it may incur as a result of injury to students on its premises. There is no cover for accidents which are nobody’s fault. Assistance in emergencies to students with a disability A Student will be indemnified against the University’s legal liability when assisting a student with a disability during emergency evacuations, or drills for them, in the following circumstances: a) Where he/she has acted under the supervision of, or following instructions given by a member of the University’s staff. b) Where he/she has acted in a voluntary capacity and in a reasonable manner in the absence of instructions from authorised persons. Extra mural activities Insurance protection is in place where an accident occurs during the course of an event and where the University is legally liable. In the case of events such as those organised by the Students’ Union or by outside bodies where an accident occurs as a result of negligence on the part of the organisers, any claim would normally be brought against them as it would be unlikely that the University would be held legally liable. Personal accident Although an element of Personal Accident insurance is included in the University’s Overseas Travel policy the University does not provide general Personal Accident Insurance for students. It is the student’s responsibility to arrange their own cover should they wish to do so. However, Personal Accident Insurance is available for students belonging to the various Students’ Union sports clubs. For further details please contact the Students’ Unions Finance Manager. Students visits to outside organisations When visits are made to exhibitions and places open to the general public, no application for insurance should be made. Many firms, particularly the larger ones, encourage visits by the public in organised parties and although the premises may include workshops and laboratories the majority of host organisations will not require to be indemnified. 47 Should firms require a written indemnity they should be asked to indicate precisely what they wish to be indemnified against. The Administrative/Advisory Officer must then be asked to provide the appropriate statement of indemnity. Student Overseas Travel General The University has automatic travel insurance cover for employees and students. This policy provides cover for employees travelling overseas on official University business and students who travel overseas as part of their UWE course. Employees are defined as persons with a contract of employment with the University. Our Insurers have confirmed that the cover will also apply to external examiners if travelling on University business and being paid by the University for their services. However it will not apply to other persons who are sub-contracting their services to the University No cover applies for holidays or other personal travel. Staff/students should make alternative insurance arrangements for that part of their travel which is not University business. How to arrange cover Cover is automatic for UWE staff and students who travel overseas on designated University activities. There is no requirement to complete a proposal form or pay a premium. Summary of insurance cover and pre travel advice, please click on the following link: http://www.uwe.ac.uk/finance/sec/insurance/intranet/docs/btravel2.pdf How to make claims Claim forms can be accessed via the Financial Services (insurance) web page http://www.uwe.ac.uk/finance/sec/insurance/. Students will be expected to settle their own claims directly with Insurers. However, you may contact the Administrative/Advisory Officer on ext. 82607 for advice. The contact number for the Insurers, U.M. Association Ltd. Is 0207 847 8681. The Global Security Centre Security & Incident Management Support Service This support service is provided as part of the travel cover to assist travellers caught up in any security or other major incidents whilst overseas on University business. The Global Security Centre also provides online destination advice, e.g. Country Risk Forecasts and City Briefs, to travellers prior to starting their journey. Please see the summary of cover for details of this service by clicking on the following link: http://www.uwe.ac.uk/finance/sec/insurance/intranet/docs/btravel2.pdf Students travelling by private, public or University transport 48 Where students drive private cars or are passengers in private cares, whether they are travelling to or from the University for the purpose of attending classes, or from the University in connection with visits arranged by teaching staff, the University has no insurance responsibility. Any motor claims would be processed under the insurance policy covering the motor vehicle. Similarly, where students travel in a party by coach or train, claims would be dealt with through the carrier’s insurance. Students are not regarded as being in the University’s employment so their cars do not need to be insured for business use. Any passengers will be covered by the normal third party insurance (part of the Motor policy) effected by the student. Where students are passengers in a car driven by a member of staff and are on University business, they should check that the driver’s insurance permits the use of the car on the employer’s business. In practice, insurance companies prefer to extend cover to include business use and this may have been done on a standard basis but, if this is not the case, the driver may not be covered by insurance while carrying students. Overseas visits or study periods Travel insurance cover is provided for students who are required to travel overseas for part of their course. Claims Details of any occurrence from which a claim may result must be sent immediately to John Elliott, Insurance and Data Protection Compliance Officer who must be kept fully informed of all developments. This is particularly important concerning possible liability claims (e.g. following accidents on UWE premises). Any intimation of claim or other correspondence must be forwarded to John Elliott, Insurance and Data Protection Compliance Officer immediately and without acknowledgement to the other party. An appropriate acknowledgement will be sent by him. Study Days (Conferences) It is not possible to undertake study days, or attend conferences when they occur at the same time as clinical placement, or university lectures. The exception to this would be the RCM conference. In the first instance, please liaise with your personal tutor. 49 50