Burns Burns occur from heat, chemicals, electric current, radiation
advertisement
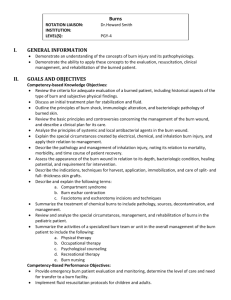
Burns Burns occur from heat, chemicals, electric current, radiation; effects are influenced by temp of the burning agent, duration of contact time, type of tissue injured Most burns are preventable Types of burns Thermal burns – flame, flash, scald, or contact with hot objects; most common type of burn injury Chemical burns – acids, alkalis, organic compounds; alkaline burns are worse than acid burns, they adhere to tissue and cause liquefaction; alkalines include oven/drain cleaners, fertilizers, heavy industrial cleaners Smoke/Inhalation injuries – usu. gases are cooled to body temp before they reach the lungs, get redness and airway swelling, major predictor of mortality in burn pts Carbon monoxide poisoning – cause the majority of deaths at the scene, displaces oxygen on the hemoglobin molecule causing carboxyhemoglobinemia and hypoxia, skin is “cherry red” Inhalation injury above the glottis (upper airway) – usu. heat produced; may have burns of the oropharynx and larynx with redness, blistering, edema; can cause mechanical obstruction quickly; symptoms suggesting this injury are facial burns, singed nasal hair, hoarseness, painful swallowing, carbon in the sputum, burn occurred in enclosed space, clothing burns around chest and neck Inhalation injury below the glottis (lower airway) – usu. chemically produced, pulmonary edema might not appear until 12-24 hours after the burn, symptoms of ARDS Electrical burns – can have direct damage to nerves and vessels, sparks can also ignite clothing, severity of injury is hard to tell as most damage is below the skin (“iceberg effect”), can cause muscle contractions strong enough to break bones, since falls often occur all pts with electrical burns should be assumed to have a cervical spine injury, also are at risk for dysrhythmias and cardiac arrest, myoglobinuria, acute tubular necrosis (ATN) and renal failure; delayed cardiac problems can happen in first 24 hours Classification of burn injuries Depth of burn – pg 475, Table 25-4 Partial thickness superficial (1st degree) – like a sunburn, no blisters (can blister after 24 hours) 1 Partial thickness deep (2nd degree) – has blisters that are red, shiny, wet, severe pain, mild to moderate edema, has viable skin that can regenerate Full thickness (3rd and 4th degree) – dry, waxy white, leathery or hard skin, no pain due to nerve destruction, needs skin grafts Extent of burn – rule of nines is okay for initial assessment of adult burns (know how to calculate this – pg 476), extent of burn is often revised after edema has subsided Location of burn – burns to face and neck and circumferential burns of chest/back lead to big risk to respiratory function; burns of hands, feet, joints, eyes lead to problems with self-care and future function; burns to ears and nose lead to big risk of infection due to lack of blood supply; burns to buttocks/perineum lead to high risk of infection; circumferential burns to extremities can lead to circulatory problems and compartment syndrome Patient risk factors – older adult heals more slowly, any preexisting CV, respiratory, or renal disease has poor recovery, also diabetes and peripheral vascular disease, alcoholism, drug abuse, malnutrition; also if additional injuries were incurred including fractures, head injuries, other trauma Phases of Burn Management Prehospital Remove the person from the burn source Stop the burning process If small burn (<10%) cooling with clean, cool tap water-dampened towels If large burn (> 10%) focus on ABCs – Airway (patency, soot, singed nasal hair), Breathing (ventilation), Circulation (pulses, elevate burned limbs above the heart) Prevent hypothermia by cooling large burns < 10 minutes or immerse Never cover with ice (causes vasoconstriction) Remove as much burned clothing as possible If chemical burn, remove chemical particles from the skin and flush with copious amounts of water If carbon monoxide is suspected, give 100% humidified oxygen Emergent (resuscitative) – time required to resolve the immediate, life-threatening problems, usu. lasts about 72 hours, primary concerns are hypovolemic shock and edema, this phase ends when diuresis begins Pathophysiology – massive shift of fluids out of the blood vessels and into the interstitial spaces, have third spacing (fluids moving to areas that normally have minimal or no fluid – exudate, blister, edema in nonburned areas), also have insensible losses from large, skinless body surfaces and respiratory 2 system; RBCs are hemolyzed causing hemoconcentration and an elevated hematocrit; major shifts in sodium and potassium S/S – hypovolemic shock (don’t really have fluid loss but the fluid gets sequestered), full thickness and deep-partial thickness burns don’t hurt due to nerve damage, adynamic ileus (body’s response to trauma and potassium shifts), shivering (b/c of heat loss, anxiety, pain); usu. alert and interactive (rarely are they unconscious unless they have hypoxia from smoke inhalation, head trauma, substance abuse, excessive sedation) Cx – most common organ systems affected are CV, respiratory, urinary o CV – dysrhythmias, hypovolemic shock, circulation impairment from circumferential burns/edema – may need escharotomy; sludging from increased blood viscosity – need adequate fluid replacement; risk for VTE especially with comorbidities o Resp – upper airway edema and airway obstruction, onset can be insidious, burns to neck and chest can be very dangerous due to inelastic eschar causing constriction; lower airways get interstitial edema, watch for agitation, restlessness, change in rate/character of respirations; initial chest xray may look normal but worsens in 24-48 hours, also watch ABGs o If they have preexisting cardiopulmonary disease can get heart failure, pulmonary edema, respiratory infection o Urinary – acute tubular necrosis (ATN) from hypovolemia, can lead to acute renal failure; also myoglobin and hemoglobin (from muscle cell and RBC breakdown) can occlude renal tubules – tx with adequate fluid replacement Nursing care – need rapid/thorough assessment and intervention, best to be at a burn center o Airway – early intubation to prevent need for emergency tracheostomy (within 1-2 hrs of a face/neck burn), extubate after edema resolves (3-6 days after burn unless severe inhalation injury), may need escharotomies of the chest wall if burns of neck/trunk; if smoke injury suspected do a fiberoptic bronchoscopy to look at the lower airway; if not intubated give 100% humidified oxygen, highFowler’s position, cough/deep breathe every hour, reposition every 12 hours, chest PT, suction as necessary; CO poisoning is treated by 100% oxygen until carboxyhemoglobin levels normalize o Fluids – need at least 2 large-bore IV lines, central line may be done for > 30% burns, may need an arterial line for blood gases/invasive BP monitoring, give LR or albumin or both; use the Parkland formula (pg 483) to calculate amount of fluids (based on pt’s weight and % surface area burned); adequate fluid volume is determined by urine output (check hourly) and MAP and BP by arterial line o Wound care – priority after airway, circulation, and fluid replacement; need cleansing and gentle debridement to remove necrotic skin; shower with tap water, twice a day dressing changes; infection is 3 biggest risk (usu. from own flora); use PPE (hats, masks, gowns, gloves); use nonsterile gloves to remove dressings and wash the wound, use sterile gloves to apply ointments and sterile dressings, keep the room warm (85 degrees), must change PPE between patients, clean and disinfect equipment/environment between patients, keeping the wound covered is important Open method – cover burn with topical antimicrobial and no dressing Closed method – sterile gauze dressings impregnated with antimicrobials (some can be left on for several days) o Other care – Face – very vascular, can get very edematous, use ointments and gauze but limit pressure on these delicate structures, may need eye ointments, may need artificial tears Ears – keep free of pressure due to poor circulation and big risk of infection, no pillows (pressure can cause chondritis, ear may stick to the pillow), elevate head using rolled towel under the shoulders (also for neck burns to prevent neck contractures) Hands/arms – extend and elevate on pillows to decrease edema, splints to keep them in functional position Perineum – keep as dry and clean as possible, need indwelling urinary catheter to get hourly urine outputs and keep perineal area clean Physical therapy – begun immediately, need early ROM exercises to move fluid, maintain function, prevent contractures o Drug therapy Analgesics/sedatives – IV pain meds only, no IM or oral meds b/c they are not absorbed properly, give opioids for pain control Tetanus immunization – for everyone Antimicrobial agents – used after the wound has been cleaned, systemic antibiotics are not used since it won’t get to the wound very well, silver sulfadiazine creams are used (assess for sulfa allergy) VTE prophylaxis – Lovenox and/or SCDs o Nutrition Early (within several hours of injury) and aggressive; enteral feedings, rarely use parenteral route, with large burns can get paralytic ileus within a few hours of the burn – insert NG and then begin feedings slowly; have a hypermetabolic state and usually need double the calories; give high calorie nutrition supplements, milkshakes, protein powder, vitamins 4 Acute (wound healing) – begins with fluid mobilization and diuresis, ends when the burned area is completely covered by skin grafts or the wounds are healed, can take weeks or months Pathophysiology – diuresis occurs decreasing edema, burn depth is more evident, wound healing begins S/S – partial thickness wounds form eschar which begins separately, once eschar is removed new skin tissue will appear, full-thickness wounds will need surgical debridement and skin grafting Lab values – the body is trying to achieve homeostasis so electrolyte levels have to be watched closely o Sodium – can be hyper or hypo; prevent water intoxication (hyponatremia) by drinking fluids other than water o Potassium – can by hyper or hypo; potassium is constantly lost through the burn wound Complications o Infection – have lost the body’s first line of defense; infection in the burn wound will have to be treated with systemic abx after cultures; at high risk for sepsis; remain immunosuppressed for awhile; if sepsis is suspected get cultures from wounds, blood, urine, sputum, oropharynx, perineum, IV sites o CV/Resp – same cx as in the emergent phase o Neuro – may have odd behaviors (ie.. disoriented, withdrawn, combative, hallucinations, delirium at night), transient state that isn’t well understood, may need psych services o Musculoskeletal – skin is less supple and pliant, ROM may be limited, contractures can occur, tend to assume a flexed position when in pain; need to stretch and move as much as possible, splint to prevent contractures o GI – can get paralytic ileus from sepsis, diarrhea from feedings/abx, constipation, Curling’s ulcer from stress (prevent this by feeding quickly after burn, giving antacids, histamine blockers, or proton pump inhibitors) o Endocrine – increase in blood glucose from stress also from the increased calorie intake (give IV insulin b/c they must eat) Nursing care o Wound care – prevent infection, clean and debride, promote wound healing and/or successful skin grafting; need daily observation, assessment, cleansing, debridement, and dressing reapplication o Excision and grafting – excision is usually done on day 1 or 2 in the OR, will cover the wounds with a biologic dressing or allograft for temporary coverage; big risk of bleeding so thrombin or epinephrine is applied topically; autograft is the patient’s own skin; early excision allows for function to be restored and scar tissue to be limited; donor skin areas create a new open wound; can grow their own skin from biopsy specimens; artificial skin is another option 5 o Pain management – have continuous pain but also has treatmentinduced pain; first line treatment is medications, can do opioids via PCA; if no IV can do slow-release, twice a day opioids (MS Contin); give around the clock oral analgesics; can also give anxiolytics to potentiate analgesics (ie. Ativan, Versed); give pre-meds before dressing changes; use nonpharmacologic strategies; give the patient as much control as possible o PT/OT – vigorous PT is needed, good time to exercise is during and after wound cleansing (skin is softer, bulky dressings are removed); if they have neck burns must sleep without pillows, need splints o Nutritional therapy – need enough calories and protein to promote healing, still in a hypermetabolic and highly catabolic state; don’t want them to lose more than 10% of preborn weight o Psychosocial care – patient and caregiver have many needs Rehabilitative (restorative) – begins when burn wounds have been healed and pt is able to resume some self-care, can be as early as 2 weeks after burn or up to 7-8 months Pathophysiology – in 4 -6 weeks new skin will be raised and red, if they don’t have good ROM the new tissue will shorten causing a contracture, takes 12 months for the suppleness to return; need gentle pressure with custom-fitted pressure garments, can only be worn over healed wounds and should be left on at all times except during bathing, also need to protect new skin from sunburn Complications – most common are skin/joint contractures and hypertrophic scarring; need to work on extension Nursing Care – encourage pt to actively participate in their care, keep morale up, address spiritual and cultural needs, emphasize what they can do not what they can’t 6