Dosimetry in Diagnostic Radiology for OPTIMA XR200 Mobile X
advertisement

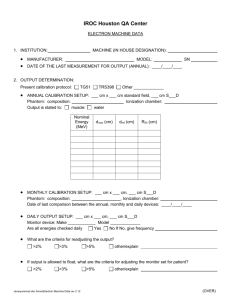
A RESEARCH PROPOSAL DOSIMETRY IN DIAGNOSTIC RADIOLOGY FOR OPTIMA XR 200 MOBILE X-RAY MACHINE BASED ON TRS 457 PROTOCOL BY NOR SHAZLEEN AN SHUKOR RESEARCH OFFICER Q41 MEDICAL RADIATION PROGRAMME PPSK TABLE OF CONTENTS Title : Dosimetry in Diagnostic Radiology for OPTIMA XR200 Mobile X-Ray Page Machine based on TRS 457 protocol 1.0 Research Overview 1.1 TRS 457: Dosimetry in Diagnostic Radiology: An International Code of Practice 1.2 Definition of Incident Air Kerma, Entrance Air Kerma dan Air Kerma Area Product based on TRS 457 2.0 Aims & Objectives 2.1 Aims 2.2 Objectives 3.0 Part 1 3.1 Measurement of backscatter factors, B of kilovoltage x-ray beam for OPTIMA XR200 mobile x-ray machine using Gafchromic XR-QA film, Gacfchromic EBT2 and Gafchromic EBT3 film. 3.1.1 Introduction 3.1.2. Materials 3.1.3 Methods 3.1.3.1 Determination of effective energy 3.1.3.1.1 Determination of Half Value Layer of an x-ray beam 3.1.3.1.2 Determination of Linear Attenuation Coefficient, µ from HVL Values. 3.1.3.2 Films calibration 3.1.3.3 Measurement of backscatter factor (B) 3.1.3.2.1 In-air measurement 3.1.3.2.2 Phantom measurement 3.1.3.4 Backscatter Factor Calculation 3.1.4 Expected Result & Findings 3.1.4.1 Determination of Effective Energy 3.1.4.1.1 Effective energy determined by using X-ray Form Factor, Attenuation and Scattering Table by Chantler,C.T et al 2003 (Tong ,N.K 2008). 3.1.4.1.2 Effective energy determined by using X-Ray Mass Attenuation Coefficient Table for Aluminium by NIST 3.1.4.2 Determination of Backscatter factor 3.1.4.2.1 The dose at the patient or phantom surface for a given field size (Dw,sur,fs) and the dose in air for the same field size with no phantom present (Dw,air,fs) for different tube voltages. 3.1.4.2.2 Backscatters data for different tube voltages (kVp) 3.1.4.2.3 Comparison of backscatter factors ( B) for water with the previous studies 4.0 PART 2 4.1 Measurements from diagnostic ionization chamber and films dosimeter for incident air kerma (Ki) 4.1.1 Introduction 4.1.2 Materials 4.1.3 Methods 4.1.3.1 HVL Measurement 4.1.3.2 Measurement of Incident Air Kerma (Ki) 4.1.3.3 Incident Air-Kerma Calculation 4.1.4 Expected Result 4.1.4.1 HVL Measurement 4.1.4.1.1 Chest Examination 4.1.4.1.2 Abdomen Examination 4.1.4.2 Incident Air Kerma (Ki) Measurement using ionization chamber 4.1.4.3 Incident Air kerma Measurement using Films Dosimeter 5.0 PART 3 5.1 Measurements of Entrance Air Kerma (Ke) for Indirect and Direct method 5.1.1 Introduction 5.1.2 Materials 5.1.3 Methods 5.1.3.1 TLD calibration 5.1.3.2 HVL Measurements 5.1.3.3 Entrance Surface Air Kerma (Ke) measurement using Indirect and Direct measurements 5.1.3.3.1 Indirect measurement 5.1.3.3.2 Direct measurement 5.1.3.4 Data Calculation Entrance Surface Air Kerma (Ke) 5.1.3.4.1 Indirect Measurement 5.1.3.4.2 Direct measurement using TLDs 5.1.3.4.3 Example of calculation for Indirect Measurement of entrance surface air kerma (Ke) . 5.1.3.4.3 Example of calculation for Direct Measurement of entrance surface air kerma (Ke) 5.1.3.5 Expected Results 5.1.3.5.1 Indirect Measurement of Entrance Surface Air Kerma (Ke) 5.1.3.5.1.1 Entrance surface Air Kerma (Ke) from ionization chamber 5.1.3.5.1.2 Entrance surface Air Kerma (Ke) from XR- QA film 5.1.3.5.1.3 Entrance surface Air Kerma (Ke) from EBT2 films 5.1.3.5.1.4 Entrance surface Air Kerma (Ke) from EBT3 films 5.1.3.5.2 Direct Measurement of Entrance Surface Air Kerma (Ke) using TLD 100 and TLD 100H 5.1.3.5.3 Comparison of Entrance Surface Air Kerma for Direct Measurement Between ionization chamber, Gafchromic XR-QA film , GAchromic EBT2 film and GAchromic EBT3 film. 5.1.3.5.4 Comparison of Entrance Surface Air Kerma for Indirect and Direct Measurement using ionization chamber 6.0 Expected Outcomes 7.0 References Dosimetry in Diagnostic Radiology for OPTIMA XR200 Mobile X-Ray Machine based on TRS 457 Protocol. 1.0 Research Overview Dosimetry in diagnostic radiology requires the use of specialized instrumentation, the design and performance of which must be matched to the needs of the clinical situation. In addition, there are special requirements for the calibration of such instruments so that the measurements are traceable to national or international standards. The main aim of dosimetry in with respect to the X-ray use in medical imaging is to determine dosimetric quantities for the establishment and use of guidance levels (diagnostic reference levels). The role of dosimetry is to determine the amount of radiation, i.e, dose received by a person from the radiological examination .The challenges in diagnostic radiology dosimery come from the diversity and complexity of the X-ray delivery from the modalities themselves, and the interaction these with the various sections of human anatomy (Ahmed et al, 2010).It is possible to measure organs dose directly with the use of suitable phantoms and dosimeters. The additional objective of dosimetry in diagnostic and interventional radiology is the assessment of equipment performance as a part of the quality assurance process. Kilovoltage x-ray beam dosimetry provides a number of challenges which are not present for megavoltage x-ray beams (Nahum 1996). Firstly, as most dosimeters have a relatively large dimension in the depth direction, the rapid fall off of dose with depth means there can be a significant dose gradient over the measuring volume of the dosimeter. Another issue is that dosimeter response is sensitive to the materials used in its construction. For low energy xray beams, the photoelectric effect is a dominant interaction process and the photoelectric cross section has a strong dependence on the atomic number of the material. The third challenge is that ionization chambers do not act as Bragg–Gray cavities in the kilovoltage x-ray energy range and so cavity theory cannot be used for reference dosimetry (Ma and Nahum 1991, Hill et al 2014).GafchromicR films were first introduced in medical applications for radiotherapy dose assessment (Sayeg and McLaughlin 1989, Chiu-Tsao et al 1994), but in the last few yearsnew models have been produced with increased sensitivity to lower doses and optimized energy dependence for use in radiology. GafchromicR XR type R and type T have been recently developed for the measurement of radiation doses in the range 0–10 Gy (Thomas et al 2003, Cheung and Butson 2004, Butson and Cheung 2004, Butson et al 2005, Cheung and Butson 2005, Dini and Koona 2005). These films are very useful for direct measurements of skin dose from fluoroscopical procedures (Giles and Murphy 2002). In diagnostic radiology, there is often the necessity of performing dose measurements in the range 0–100 mGy. In a previous study (Gorny et al 2005) the application of a prototype GafchromicR HXR film for the measurement of radiation dose profiles in computed tomography has been discussed. A new film model XR-QA with similar characteristics and specifically designed for kilovoltage dosimetry is currently under development by the manufacturer. The great sensitivity of this new film has been recently tested for radioisotopes sources in the range 21–6 MV (Chiu-Tsao et al 2005) 1.1 TRS 457: Dosimetry in Diagnostic Radiology: An International Code of Practice International standardization in dosimetry is essential for the successful exploitation of radiation technology. Soon after it was founded, the IAEA initiated a programme on the dosimetry of ionizing radiation, helping Member States develop the calibration and measurement capabilities necessary for the application of radiation in medicine, radiation protection, industry and other applications. The IAEA disseminates standards for radiation measurement, conducts dose audits and comparisons, develops and transfers dosimetry techniques, and provides training and guidance on radiation measurements. Much of this work is carried out through the IAEA/WHO Secondary Standards Dosimetry Laboratory (SSDL) network. For some time now there has been a growing awareness that radiation dose originating from medical diagnostic procedures in radiology is contributing an increasing proportion of the total population dose. This has been particularly evident for examinations using computed tomography equipment, where increasing usage with patient doses in excess of occupational safety limits is well established. However, diagnostic X ray imaging generally covers a diverse range of examination types, many of which are increasing in frequency and technical complexity. This has resulted in the development of new dosimetric measuring instruments, techniques and terminologies which present challenges to those working in the clinical environment and those supporting them in calibration facilities. In response to heightened awareness of the importance of patient dose contributed by radiology procedures, there has been a general trend to effect control of patient doses by applying the principles of optimization coupled with an increase in regulatory enforcement. This has been reflected by an increasing demand from Member States for the IAEA to provide assistance inestablishing programmes for quality assurance and quality control of X rays used in diagnostic radiology. A high level of dosimetry in radiology departments in Member States cannot be achieved without a systematic and consistent approach. Following the recommendations of the advisory committee for the IAEA/WHO SSDL network, known as the SSDL Scientific Committee, development of a new Code of Practice for Dosimetry in Diagnostic Radiology was started in 2000 with the appointment of a drafting group that included: G. Alm Carlsson (Sweden), D.R. Dance (United Kingdom), L. DeWerd (United States of America), H.-M. Kramer (Germany), K.-H. Ng (Malaysia), F. Pernicˇka (Czech Republic) and P. Ortiz Lopez (IAEA).This publication is seen as a continuation of the IAEA’s policy of providing guidance in the area of dosimetry of ionizing radiation for medical physics and follows on from Absorbed Dose Determination in External Beam Radiotherapy: An International Code of Practice for Dosimetry Based on Standards of Absorbed Dose to Water (Technical Reports Series No. 398), which was published in 2000. The Code of Practice for Dosimetry in Diagnostic Radiology addresses issues of dosimetry involving calibrations and measurements from the perspective of both the SSDLs and the clinical users.This Code of Practice has been endorsed by WHO and PAHO.The IAEA technical officers responsible for the preparation of this report were F. Pernička and I.D. McLean of the Division of Human Health. This study will focus at point 8.4 (chapter 4); Code of practice in Clinical Measurement in General Radiology. In this code of practice, the principal quantities to be measured for use in general radiography are the incident air kerma, the entrance surface air kerma and the air kerma area product. For phantoms, the incident air kerma is measured, the entrance air kerma is determine from measurement with TLD and the air kerma area product is measured using DAP meter. 1.2 Definition of Incident Air Kerma, Entrance Air Kerma dan Air Kerma Area Product based on TRS 457 1.2.1 Incident air kerma, Ki The incident air kerma, Ki, is the kerma to air from an incident X ray beam measured on the central beam axis at the position of the patient or phantom surface (Fig). Only the radiation incident on the patient or phantom and not the backscattered radiation is included. The unit for incident kerma is J/kg or Gray (Gy). 1.2.2 Entrance surface air kerma (Ke) The entrance surface air kerma, Ke, is the kerma to air measured on the central beam axis at the position of the patient or phantom surface (Fig. 3.2). The radiation incident on the patient or phantom and the backscattered radiation are included .The unit for incident kerma is J/kg or Gray (Gy). The entrance surface air kerma is related to the incident air kerma by the backscatter factor, B, thus: Ke = KiB 1.2.3 Air kerma–area product The air kerma–area product, PKA, is the integral of the air kerma over the area of the X ray beam in a plane perpendicular to the beam axis (Fig. 3.2), thus: Unit: J·kg–1·m2. If the special name gray is used, the unit of air kerma–area product is Gy·m2.The air kerma–area product has the useful property that it is approximately invariant with distance from the X ray tube focus (when interactions in air and extrafocal radiation can be neglected), as long as the planes of measurement and calculation are not so close to the patient or phantom that there is a significant contribution from backscattered radiation. Figure 1 : Diagram of measuring arrangement based on TRS 457 2.0 Aims and Objectives 2.1 Aims The aim of this research is to study the dosimetry in diagnostic radiology based on TRS 457 components. . The main aim of dosimetry in with respect to the X-ray use in medical imaging is to determine dosimetric quantities for the establishment and use of guidance levels (diagnostic reference levels). 2.2 Research objectives 1. To measure the backscatter factor, BSF for kilovoltage x-ray beam for OPTIMA XR200 mobile x-ray using ionisation chamber, Gacfchromic XR-QA, EBT2 and EBT3 films.. 2. To compare the measurement from diagnostic ionization chamber and film dosimetry for incident air kerma ( Ki) . 3. To compare the measurement of the Entrance Surface Air kerma ( Ke) using direct and indirect method using IC, films dosimeter, TLD100 and TLD 100H for OPTIMA XR200 Mobile x-ray machine 3.0 PART 1 3.1 Measurement of backscatter factors, B of kilovoltage x-ray beam for OPTIMA XR200 mobile x-ray machine using Gafchromic XR-QA film,Gacfchromic EBT2 and Gafchromic EBT3 film. 3.1.1 Introduction Kilovoltage X-rays are used extensively in the treatment of superficial tumors and so it is important to be able to determine the dose on a patient’s skin during treatment. Forthe X-ray energies relevant to kilovoltage X-ray therapy, the surface dose consists of both primary radiation and secondary radiation scattered back to the surface from deeper inside the patient. This scatter radiation is generated by the following interaction processes: Rayleigh scattering, Compton scattering, the photoelectric effect, and fluorescentor characteristic radiation. Backscatter factors in water (BW) are used to determine the contribution of scattered radiation to the total dose at the surface and are used in reference and relative dosimetry of kilovoltage voltage X-ray beams [2–4]. One definition of BW is given by: Where Dw,sur,fs is the dose (or dose rate) at the solid water phantom surface for a given field size, and Dw,air,fs is the dose (or dose rate) in air for the same field size with no patient or phantom present [5]. It has been shown that BW are influenced by a wide range of factors including beam quality, field size, source-to-surface distance (SSD), and properties of the phantom material. Study by L.Smith at el 2011 indicated that backscatter factors are essential in the determination of radiation dose for kilovoltage X-ray beams. The accurate measurement of backscatter factors in water (BW) is difficult and published values are based largely on Monte Carlo calculations. A number of studies have found that the measurement of BW in the energy range from 50 to 300 kVp is possible using Gafchromic EBT film, but this film is no longer commercially available. The results demonstrate that Gafchromic film is a suitable dosimeter for BW measurements for clinical kilovoltage X-ray beam. The experimental determination of Bw in the kilovoltage X-ray range is not straightforward as most dosimeters perturb the beam due to their size, cannot accurately measure the surface dose or have a significant energy response for low energy Xrays. Most of the previous works, Bw have been experimently determined using specially designed parallel-plate ionisation chambers or small thermoluminescent dosimeters .For these reasons, the BW in the reference dosimetry protocols has largely been determined via Monte Carlo simulations.( Smith et al 2011). However it has been noted that the use of generic published BW may increase the uncertainties involved in dosimetry, particularly for the higher-energy X-ray beams and may vary for different treatment units [7, 22]. Therefore equipment-specific experimental verification of tabulated values are desirable for clinical use and may increase the accuracy of both reference and relative dosimetry measurements [22] The radiochromic GafchromicTM films have several features making them attractive as a radiation dosimeter including very thin width, good spatial resolution, good dose ranges, selfdevelopment and ease of use [23–26]. In previous studies, the energy dependence of GafchromicTM EBT film has been measured for X-ray beams and has been found to be relatively energy independent [26]. For these reasons, EBT filmhas been used successfully as a dosimeter for low energy photon beams to determine both BW and depth doses. In this work, we investigated the suitability of Gafchromic EBT2 film and Gafchromic XR-QA film as a dosimeters for the measurement of BW in kilovoltage X-ray beam dosimetry. We determined which parameters in the irradiation and readout lead to greater uncertainties in the measured dose and we suggest methods to reduce these uncertainties. 3.1.2. Materials 1. XR200 Optimo mobile x-ray machine 2. Ionisation chamber & Electrometer 3. Gafchromic XR-QA film 4. Gafchromic EBT2 film 5. Gafchromic EBT3 film 6. Flatbed Film Scanner Epson Expression 10000XL with Verisoft Software 7. PTW SFD Diagnostic Ionization chamber 8. Semiconductor Diagnostic IC 9. PMMA DSA phantom 10. Solid water phantom 11. Polystrene 12. Al filter 3.1.3 Methods 3.1.3.1 Determination of effective energy 3.1.3.1.1 Determination of Half Value Layer of an x-ray beam The HVL of X-ray beam is determined by attenuation techniques using aluminium sheets (Al), ranging from 0.5 to 1.0mm in thickness by measuring the dose for different thickness of aluminum. From the measurement , the half value layer of the specific x-ray energy is determined by plotting semilog-graph of transmission percentage versus Aluminium sheets. Calibrated SFD diagnostic ionization chamber is connected to the electrometer and is perpendicularly positioned toward the x-ray tube. The distance from the focal spot of x-ray tube to the surfacr of IC is set to be 100cm. Tube is collimated to 10cm x10cm field size with the broad focus. Aluminium sheet is stacked by using the tape just under the tube collimator. First exposure is made without the aluminium sheet and is repeated for three times. Next exposure is given with 0.5mm aluminium is place under the collimator. This step is repated with addition step by step of 0.5mm Al sheet until the reading become half of the initial reading. Final exposure is made with removal of all the Al sheets. The final reading must not differ more than 2% from the initial reading without Al sheet. Same procedures are repeated at all beam energies. Each reading is divided by the initial reading to get the percentage of penetration. Graph of penetration percentage versus Al thickness are plot for all energies to get the values of HVL. 3.1.3.1.2 Determination of Linear Attenuation Coefficient, µ from HVL values Linear attenuation coefficient, µ of polyenergetic x-ray beam is determine by the equation : Ix= Ioe -µx Where; Ix/Io = 0.5 x : HVL By solving the equation, µ = 0.693/HVL µ for every energy is calculated and converted to the corresponding effective energy by using the X-ray form Factor, Attenuation and Scattering Table (Chantler,C.T et al 2003). Where µ/ρ for every energy is calculated and converted to the corresponding effective energy by using the X-Ray Mass Attenuation Coefficient Table for Aluminium by NIST. 3.1.3.2 Films calibration In order to characterize the Gafchromic XR-QA response small pieces of film (3 × 3 cm) were irradiated with diagnostic mobile x-ray machine Optimo XR200. The film section size was selected to ensure that the calibration x-ray field was uniform to better than 1% over the film area. The film sections were numbered and marked so that they could be placed on the scanner bed to match their positions and orientations in the original sheet. “Free-in-air” indicates that the calibration films were exposed to the primary x-ray beam with negligible x-ray scatter. For each exposure, one 3 cm x 3cm film section was randomly selected and placed at the center of 10 cm x 10 cm Styrofoam/ polystyrene block to avoid the backscatter effect .The distance from source to detector is 100cm. Each piece was exposed with simultaneous measurements of dose performed by Optimo XR200 Mobile X-Ray machine unit for tube voltage 50kVp with different mAs for generate the dose levels from 0 to around 100 mGy which is checked by using ionization chamber for diagnostic purpose. This process repeated for another tube voltages (70,80,100, 120 and 150kVps). Three film samples randomly extracted from three different film sheets were simultaneously exposed for every calibration point, in order to take into account the film response homogeneity. Before and after the exposures, the calibration films were stored in individual envelopes in a dark, environmentally controlled room. For the calibration films, the pixel value for each film was plotted against absorbed dose and a thirdorder polynomial fit was applied to each curve using the Verisoft software.These calibration curves were then used to determine the dose absorbed by each of the resultant films. These process is repeated for Gafchromic EBT2 and Gafchromic EBT3 films. 3.1.3.3 Measurement of backscatter factor (B) A minimum of three Gafchromic XR-QA film pieces were used in all measurements conducted in this study, and the mean dose absorbed by these film pieces was used for analysis purposes. Any film pairs that were irradiated under the same conditions whose measured doses differed by more than 5% were discarded and those measurements were repeated. The films sheets were cut into pieces of 3x3 cm pieces. Prior to irradiation, the optical density of each film piece was scanned using Epson Expression 10000xl flatbed film scanner .All irradiation measurements were carried out using a Optimo XR200 Mobile X-Ray machine unit with a tube potential ranging from 50 to 150 kVp. Beams with energies of 50, 100, and 150 kVp were used in this study. Backscatter factors in water (B) are used to determine the contribution of scattered radiation to the total dose at the surface and are used in reference and relative dosimetry of kilovoltage voltage X-ray beams .One definition of B is given by: B : Dw,sur,fs Dw,air,fs Where Dw,sur,fs : the dose (or dose rate) at the patient or phantom surface for a given field size Dw,air,fs: the dose (or dose rate) in air for the same field size with no patient or phantom present . It has been shown that B are influenced by a wide range of factors including beam quality, field size, source-to-surface distance (SSD), and properties of the phantom material. Three sets of measurements were taken to measure the backscatter: in-air ,on the surface of an solid water phantom and on the surface of PMMA phantom . 3.1.3.2 .1 In-air measurement In-air measurement, slices of polystyrene box with the thickness 15 cm were stacked and was placed on the couch table. The ionization chamber and films were place at the surface of polystyrene box with distance 82 cm and perpendicular to the beam direction of the diagnostic x-ray machine. This distance corresponds to approximately 1m from the x-ray tube target Polystyrene boxes is used in this study as the density is approximately similar to density of air. The thickness of polystyrene is 15cm to avoid scatter backscatter present form the table couch to prevent unwanted scattered radiation interacting with the film. Exposure measurements were carried out for field size of 10cm x10cm. All the readings were corrected for reference T and P.. Measurements were taken at 50,70 ,80,100,120 and 150 kVs. A light beam diaphragm was always present during the measurements. The 10 cm x10cm field measurements were taken for comparing the data with available published data; to check the method we adopted to derive the B.The condition is refer as the dose (or dose rate) in air for the same field size with no patient or phantom present (Dw,air,fs). 3.1.3.2 .2 Phantom measurement The solid water phantom with the thickness 15 cm were stacked together and was placed on the couch table. The ionization chamber and films were place at the surface of solid water phantom with distance 82 cm from surface of the light beam diaphragm of the diagnostic machine. This distance corresponds to approximately 1m from the x-ray tube target. Measurements on the phantom surface were performed in full scatter conditions with the thickness of at least 10 cm as specified in the AAPM TG-61 protocol. The thickness 15 cm is chosen so that the position of the films and IC is same with the position setup for in air measurement. This method is repeated with the PMMA phantom with the same position setup. The condition is refer as the dose (or dose rate) at the patient or phantom surface for a given field size (Dw,sur,fs). In order to ensure that film development had stabilized after irradiation, the film was left a total of 24 h before the optical density was measured. In order to minimise any possible darkening of the films by exposure to UV radiation,all films were stored in a light-proof environment when not being irradiated or read out. To minimise the effect of orientation in this investigation, all film pieces were consistently read out in the same orientation and with the same side facing upwards—that is with the active layer closer to the surface. The orientation of each film piece was determined by a small number written in the top right cover of each piece. Figure 2: Schematic diagram for the measuring backscatter set-up. 3.1.3.4 Backscatter Factor Calculation All the results from the IC and films were recorded. The doses result generate by the film dosimetry software (Verisoft) is used to calculate the backscatter factor (B) by using equation : B : Dw,sur,fs Dw,air,fs Which Dw,sur,fs : the dose (or dose rate) at the patient or phantom surface for a given field size Dw,air,fs: the dose (or dose rate) in air for the same field size with no patient or phantom present . 3.1.4 Expected Result & Findings 3.1.4.1 Determination of Effective Energy 3.1.4.1.1 Effective energy determined by using X-ray Form Factor, Attenuation and Scattering Table by Chantler,C.T et al 2003 ( Tong ,N.K 2008). kVp HVL (cm) µ Effective energy (ln2/HVL) (keV) 50 70 80 100 120 150 3.1.4.1.2 Effective energy determined by using X-Ray Mass Attenuation Coefficient Table for Aluminium by NIST kVp HVL (cm) Mass Attenuation Effective energy Coefficient (keV) µ/ρ ( g/cm²) 50 70 80 100 120 150 3.1.4.2 Determination of Backscatter factor 3.1.4.2.1 The dose at the patient or phantom surface for a given field size (Dw,sur,fs ) and the dose in air for the same field size with no phantom present (Dw,air,fs) for different tube voltages. Dw,sur,fs Tube HVL Voltage IC Solid Dw,air,fs PMMA IC water Solid PMMA water ( kVp) 50 70 80 100 120 150 3.1.4.2.2 Backscatters data for different tube voltages (kVp) Tube Effective Backscattor factor Voltage energy (B) ( kVp) (keV) = Dw,sur,fs/ Dw,air,fs IC 50 70 80 100 120 150 Solid water PMMA 3.1.4.2.3 Comparison of backscatter factors ( B) for water with the previous studies. B from measurements Effective Energy (keV) Eg : 50 This study Harrison Monte Carlo study M.Vijayan et al M.Vijayan et al Petoussi-Henss et al by 80 120 4.0 PART 2 4.1 Measurements from diagnostic ionization chamber and films dosimeter for incident air kerma (Ki) 4.1.1 Introduction Measurement of incident absorbed dose (or incident air kerma) are usually required for a specific type of radiograph (eg posterior-anterior ( PA) projection of the chest) . these ‘free in air” measurements are the best made with suitable designed ionization chamber dosimeters tof typically between 3cm3 and 60cm3 volume. The chambers should have ‘air equivalent” walls so that their energy response when calibrated in terms of air kerma is substantially uniform for all diagnostic energy spectra. If the exposure condition ( kVp,mAs) are known for the type of radiograph, measurements can be made of the x-ray tube output (air kerma) for a series of exposure conditions encompassing those used in practice. The incident air kerma for a particular radiograph taken under known exposure conditions can be derived by interpolation. Since the air kerma rate can differ appreciably for the same exposure conditions from one x-ray tube to another it is important that output measurements are made directly on the x-ray tube under study. If automatic exposure control ( AEC) is used and the exposure parameters( mAs, kVp) are not indicated it will be necessary to use a phantom to represent the patient. The phantom should provide the same amount of attenuation as an average patient and ideally should result in the same x-ray spectrum incident in image receptor. The air kerma measurement should be made at some distance from the phantom surface so as not to include backscatter radiation and corrected to FSD. 4.1.2 Materials XR200 Optimo Mobile x-ray machine Ionization chamber DUKE phantom Antromorphic phantom Gafchromic XR-QA film Gafchromic EBT2 film Gafchromic EBT3 film Al filter Retort stand 4.1.3 Methods 4.1.3.1 HVL Measurement 1. The equipment is set-up for examination of normal adult patient in manual probe. The tube voltage is select for chest examination normal adult patient. 2. Calibrated diagnostic ionization chamber is connected to the electrometer and is perpendicularly positioned toward the x-ray tube. 3. The distance from the focal spot of x-ray tube (dFTD) to the surface of IC is set to be 100cm. 4. Tube is collimated to 10cm x10cm field size with the broad focus. Aluminium sheet is stacked by using the tape just under the tube collimator. 5. First exposure is made without the aluminium sheet and is repeated for three times. Next exposure is given with 0.5mm Al sheet is place under the collimator. 6. This step is repeated with addition step by step of 0.5mm Al sheet until the reading become half of the initial reading. 7. Final exposure is made with removal of all the Al sheets. The final reading must not differ more than 2% from the initial reading without Al sheet. 8. Same procedures are repeated at all beam energies. Each reading is divided by the initial reading to get the percentage of penetration. Graph of penetration percentage versus Al thickness are plot for all energies to get the values of HVL. 4.1.3.2 Measurement of Incident Air Kerma (Ki) For the measurement of incident air kerma in general radiography, the DUKE or antrophormic human phantom is centred in the beam at the focus to film distance used clinically, with the beam size adjusted to the phantom edges. The exposure parameters (automatic exposure control (AEC) and tube voltage) chosen should be those used clinically for a postero–anterior chest, an antero–posterior abdomen or lumbar spine examination of an average sized adult human phantom. A detector of the diagnostic dosimeter is positioned at a sufficient distance from the entrance surface of the phantom to avoid backscatter and the incident air kerma is calculated from the measurement at the detector position using the inverse square law. Measured data and exposure parameters should be recorded using a worksheet. The HVL of the X ray beam is measured for the tube voltage and filtration used for the exposure. 1. Set up the X ray equipment for the chosen examination of a normal adult patient, including the selection of exposure parameters (AEC and tube voltage) and grid (or air gap), focus– skin distance and collimation. 2. Position the phantom so that it rests directly against the front plate of the vertical Bucky or the table top as appropriate. 3. Centre the phantom transversely (across the patient, left to right). 4. Position the phantom vertically (head to foot), such that all relevant AEC detectors are covered. The phantom may thus not be centered vertically, but shifted up slightly in order to cover the AEC detectors. 5. Measure and record the distance between the X ray tube focus and the vertical Bucky or table top, dFTD. Place the dosimeter in the probe holder. 6. The dosimeter should be sufficiently above the phantom surface to reduce backscatter and positioned outside the AEC detectors. A distance of about 240 mm is recommended for dosimeters that respond to backscattered radiation. 7. For dosimeters that are not sensitive to backscattered radiation (such as the many dosimeters based on a semiconductor detector) this distance could be smaller. The slightly off-axis arrangement enables the AEC detectors to function without any obstruction from the dosimeter. 8. The dosimeter should be placed as close to the central axis as possible to minimize the influence of the heel effect. 9. Measure and record the distance, dm, between the reference point of the dosimeter and the table couch. Expose the chamber three times under AEC, or manual control, and record the dosimeter readings, M1, M2 and M3, and exposure parameters used (tube voltage and tube loading or tube current and exposure time. 10. The step 1 to 9 is repeated with replacement the ionization chamber with film dosimeter ( Gafchromic XR QA , Gafchromic EBT2 film and Gafchromic EBT3 film ). Figure 3: Diagram for set-up arrangement for measurement of incident air kerma Where: dFTD : distance from tube focus to the table d : distance between detector and the tube focus dm : distance between detector and table dp : distance between the detector and phantom surface ( eg: 240mm) tp : thickness of phantom ( eg : DUKE :------cm . , Antromorhorphic :------cm ) 4.1.3.3 Incident Air-Kerma Calculation 1. The inverse square law is used to calculate the incident air kerma from air kerma at the position of the dosimeter for exposure of the standard posterior-anterior chest examination and abdomen chest examination. 2. The HVL of the beam is calculated from interpolation the measured signal for various thicknesses of attenuator. 3. The mean value, M from the dosimeter readings is calculated. 4. The Air kerma K(d) at the the measurement point (at a distance, d, from the X ray focus) is calculated from the mean value of dosimeter readings, M,using Eq: K(d) = M NK,Q0 kQ k TP Where ; kTP : correction factor for temperature and pressure = (273.2 + T ) (P0) (273.2 + T0)(P) Where; T : Temperature during measurement P : Pressure during measurement To : Reference temperature Po : Reference pressure NK,Q0 : dosimeter calibration coefficient( provided in dosimeter certificate) kQ : factor which corrects for differences in the response of the dosimeter at the calibration quality, Q0, and at the quality, Q, of the clinical X ray beam. This quality is indicated by the value of the HVL. 5. The inverse square law is used to calculate the incident air kerma, Ki to the standard exposure parameter used ( eg; chest or abdomen) Ki = K (d) ((dFTD- dm)/dFTD –tp ))² Where: dFTD ; measured tube focus to patient support distance in millimeters dm ; distance from table couch to the reference point of the chamber at the measurement position tp ; phantom thickness of standard chest /abdomen of patient Example of Incident Kerma calculation: 1. The recorded readings of the dosimeter for the repeat exposure of the standard chest phantom were: 0.293 mGy, 0.291 mGy and 0.290 mGy. The calculated mean value of the dosimeter reading M is therefore: M = (0.293 mGy + 0.291 mGy + 0.290 mGy)/3 = 0.291 mGy 2. The calibration coefficient, NK,Q0, for the dosimeter was 0.988 mGy/mGy, the beam quality correction factor, kQ, was 0.99 and the temperature and pressure correction, kTP, was 1.00. 3. The air kerma K(d) at the measurement point is therefore given by: K(d) = 0.291 mGy × 0.988 mGy/mGy × 0.99 × 1.00 = 0.285 mGy 4. The dosimeter was positioned at a distance dm = 509 mm from the wall Bucky and the focus to patient support distance, dFTD, was 1000mm (100cm). The incident air kerma is therefore: Ki = 0.285mGy ((1000-509)/1000-225))² = 0.285mGy ((491/775))² = 0.114mGy 4.1.4 Expected Result 4.1.4.1 HVL Measurement 4.1.4.1.1 Chest Examination Tube Voltage : _____kV_____mAs Filter thickness Dosimeter reading (M) Average dosimeter reading, M at (mmAl) zero thickness 0.00 ( Mo1 + Mo2)/2 = _____mGy 0.00 Interpolated HVL:_____mm Al 4.1.4.1.2 Abdomen Examination Tube Voltage : _____kV_____mAs Filter thickness Dosimeter reading (M) Average dosimeter reading, M at (mmAl) zero thickness 0.00 ( Mo1 + Mo2)/2 = _____mGy 0.00 Interpolated HVL:_____mm Al 4.1.4.2 Incident Air Kerma (Ki) Measurement using ionization chamber Projection Tube Tube Average HVL Incident air Type of Voltage Loading Dosimeter thickness Kerma (Ki) radiograph (kV) (mAs) reading (mmAl) ( mGy) Chest examination (DUKE phantom) Abdomen AP PA AP examination Antrophormic PA phantom 4.1.4.3 Incident Air kerma Measurement using Films Dosimeter Projection Tube Tube Type of Voltage Loading radiograph (kV) (mAs) Chest examination (DUKE AP PA phantom) Abdomen AP examination Antrophormic phantom PA Incident air Kerma (Ki) Film -QA EBT2 EBT3 5.0 PART 3 5.1 Measurements of Entrance Air Kerma (Ke) for Indirect and Direct method 5.1.1 Introduction Measurement Ke are required for a specific type of radiograph. Entrance air kerma can be measured indirectly from measurement of the incident absorbed dose by multiplying by the backscatter factor or directly by thermoluminescent (TLD) dosimeter. Thermoluminescent dosimetry presents some advantages: high sensitivity, which allows the use of small-sized dosimeters; response with a low dependence on photon energy and linear response for a wide dose interval; low cost and easy handle; high sensitivity, even for small doses; stable response, even under adverse environmental conditions; good reproducibility,even for small doses; and simple emission curve, with well defined peaks. Such dosimetry is based on the fact that materials will emit light when appropriately heated, after having been irradiated, with the amount of emitted light being proportional to the absorbed radiation energy. The following dosimetric materials were utilized in this present study: LiF:Mg,Ti (commercially known as TLD100),marketed by Thermo Scientific, Massachusetts, USA; LiF:Mg,Cu,P (commercially known as TLD-100H), also marketed by Thermo Scientific, Massachusetts, USA. 5.1.2 Materials XR200 Optimo Mobile x-ray machine Ionization chamber TLD 100 & 100H Gafchromic XR-QA film Gafchromic EBT2 film Gafchromic EBT3 film Antromorphic phantom Al filter TLD Reader TLD Oven Nitrogen gas 5.1.3 Methods 5.1.3.1 TLD calibration Initially a batch comprising 100 TLDs was gathered; the working batch was selected in such a way that, after five identical thermal treatment, irradiation and readout cycles, the maximum thermoluminescent response variation was lower than 3%. After this selection, the working batch comprised 50 TLD-100H samples and 50 TLD-100 samples. The thermoluminescent materials were characterized according to their main dosimetric characteristics. For this purpose, they were irradiated to X200 Optimo mobile x-ray machine with different tube voltage ( 50,70,80,100 and 150kVp). In all exposures to radiation, the samples were individually encapsulated in transparent plastic. This same procedure was utilized in all irradiations. The sensitivity factor for each dosimeter was obtained after five identical irradiation, readout and thermal treatment cycles, by calculating he ratio between each dosimeter’s mean response and the mean response of the dosimeter that presented the smallest reading variation after the five measurement cycles. The method of calibration coefficient for TLDs is following the TLD calibration method by TRS 457. In this study, the TLDs calibration measurement is carried out at a dose and with an x-ray spectrum typical of those to which the TLDs will be exposed during patient dose measurement. An absorbed dose during the chest and abdomen examination with the same kVp and mAs is used for calibration purpose. 5.1.3.2 HVL Measurements The methodology for the HVL measurement is the same as that described in indirect method with the exception that instead of measuring the HVL for a specific tube voltage, it is measured for a set of X ray tube voltages which adequately sample voltages used for the clinical examinations under consideration ( refer to 4.1.3.1). 5.1.3.3 Entrance Surface Air Kerma (Ke) measurement using Indirect and Direct measurements The entrance surface air kerma can be established indirectly from the incident air kerma using backscatter factors discussed in Part 1 or it can be measured directly using TLDs. 5.1.3.3 .1 Indirect measurement For the indirect method, the method is same as we discuss in chapter 4.1.3.2. The result is obtained from the Table 4.1.4.2) 5.1.3.3 .2 Direct measurement The entrance surface air kerma is directly measured using sachets of three TLDs taped to the phantom’s surface. One sachet of TLDs is retained so that a background correction may be made. The measurement is made as follows: 1. Set aside a three TLD sachets to provide a background reading. 2. Position the phantom and X ray equipment for the desired examination ( Chest /Abdomen) and select the appropriate exposure parameters. 3. Attach TLDs to the phantom surface. The sachet should be attached to the phantom surface as close as possible to the centre of the entrance beam. 4. Expose the phantom with the exposure parameter for desired examination. 5.1.3.4 Data Calculation Entrance Surface Air Kerma (Ke) 5.1.3.4.1 Indirect Measurement 1. Calculate the incident air kerma for exposure parameters recorded during patient examination ( from the direct measurement). 2. Calculate the entrance surface air kerma using below and the appropriate backscatter factor for water from part A study. Selection of the backscatter factor is based on the measured HVL and the field size used during the examination: Ke : KiB where Ki is the incident air kerma established for a given set of exposure parameters B is the backscatter factor for water and the selected field size. 5.1.3.4.2 Direct measurement using TLDs 1. Calculate the mean value of the background reading, M0 from background dosimeter readings M01, M02 and M03 (M0 = (M01 + M02 +M03)/3). 2. Calculate the average background corrected dosimeter reading, M from the exposed dosimeter readings M1, M2 and M3 as: Where factors fs,i are used to correct for the individual sensitivity of the i-th dosimeter. 3. Calculate the entrance surface air kerma, Ke, from the average background corrected dosimeter reading, M using the calibration coefficient, NK,Q0, of the dosimeter for the reference radiation quality, Q0, the correction factor, kQ, for the radiation quality used and the correction factor, kf, that corrects for the effect of fading of the thermoluminescence signal between irradiation of the dosimeter and its readout: 3. The process repeated for different examination exposure parameter (chest/abdomen). 5.1.3.4.3 Example of calculation for Indirect Measurement of entrance surface air kerma (Ke) . The abdomen examination of an adult 300 mm thick was done with the table at 1000 mm from the tube focus and the machine set to 84 kV and 60 mA·s. The beam HVL was measured as 3.5 mm Al and the X ray tube output at a distance, d, of 500 mm from the tube focus was measured as Y(d) = 0.075 mGy/mA·s. The incident air kerma is: Ki = 0.075mGy (mAs) ( 1000-500/1000-300)² 60mAs = 0.075mGy (mAs) (500/700)² 60mAs = 6.429 mGy The incident air kerma is: 6.43 mGy The X ray beam was collimated during examination to 200 mm × 400 mm. The backscatter factor does not vary too much with field size. It is thus reasonable to use the backscatter factor for the maximum field size of 250 mm × 250 mm. The interpolation gives, for an HVL of 3.5 mm Al, a value of the backscatter factor for water, B, of 1.43. The entrance surface air kerma can be written as: Ke: 6.43mGy x 1.43 = 9.19mGy 5.1.3.4.3 Example of calculation for Direct Measurement of entrance surface air kerma (Ke) . The three exposed TLDs and three background TLDs were read out after the chest examination of a patient. The average readings of the three exposed and three background dosimeters were 776.08 nC and 7.70 nC, respectively. The average background corrected reading is therefore: M= 776.08 nC – 7.70 nC = 768.38 nC The calibration coefficient, NK,Q0, for the TLD was 0.00035 mGy/nC and kQ for the same tube voltage and filtration setting was 1.0057. The entrance surface air kerma is therefore: Ke = 768.38 nC × 0.00035 mGy·nC–1 × 1.0057 = 0.270 mGy For an expanded standard uncertainty (k = 2) of 12%, the entrance surface air kerma measured by the TLDs is written as: Ke = (0.270 ± 0.032) mGy 5.1.3.5 Expected Results 5.1.3.5 .1 Indirect Measurement of Entrance Surface Air Kerma (Ke) 5.1.3.5 .1 .1 Entrance surface Air Kerma (Ke) from ionization chamber Projection Tube Tube Backscatter Incident Type of Voltage Loading factor air Kerma surface radiograph (kV) (mAs) ( B) from IC Air Kerma (Ki) (Ke=Ki B) Chest Entrance AP examination (DUKE PA phantom) Abdomen AP examination Antrophormic PA phantom 5.1.3.5 .1 .2 Entrance surface Air Kerma (Ke) from XR- QA film Projection Tube Tube Backscatte Incident air Entrance Type of Voltage Loading r factor Kerma radiograph (kV) (mAs) ( B) from surface XR- Air Kerma QA film (Ki) Chest AP examination (DUKE PA phantom) Abdomen AP examination Antrophormic phantom PA (Ke=Ki B) 5.1.3.5 .1.3 Entrance surface Air Kerma (Ke) from EBT2 films Projection Tube Tube Backscatt Incident air Entrance Type of Voltage Loading er factor Kerma radiograph (kV) (mAs) ( B) from EBT2 Air Kerma films surface (Ke=Ki B) (Ki) Chest AP examination (DUKE PA phantom) Abdomen AP examination Antrophormic PA phantom 5.1.3.5 .1.4 Entrance surface Air Kerma (Ke) from EBT3 films Projection Tube Tube Backscatt Incident air Entrance Type of Voltage Loading er factor Kerma radiograph (kV) (mAs) ( B) from EBT3 Air Kerma films (Ki) Chest AP examination (DUKE PA phantom) Abdomen AP examination Antrophormic phantom PA surface (Ke=Ki B) 5.1.3.5.2 Direct Measurement of Entrance Surface Air Kerma (Ke) using TLD 100 and TLD 100H Projection Tube Tube Average TLD Entrance Type of Voltage Loading Dosimeter reading Surface radiograph (kV) (mAs) (mGy) Air Kerma (Ke) TLD-100 Chest examination (DUKE TLD100-H AP PA phantom) Abdomen AP examination Antrophormic PA phantom 5.1.3.5.3 Comparison of Entrance Surface Air Kerma for Direct Measurement Between ionization chamber, Gafchromic XR-QA film , GAchromic EBT2 film and GAchromic EBT3 film. Projection Entrance Surface Air Kerma (Ke) Type of radiograph Ionization chamber Chest examination (DUKE AP PA phantom) Abdomen AP examination Antrophormic phantom PA XR-QA EBT2 EBT3 5.1.3.5.4 Comparison of Entrance Surface Air Kerma for Indirect and Direct Measurement using ionization chamber Projection Entrance Surface Air Kerma (Ke) Type of radiograph Chest examination (DUKE Indirect AP PA phantom) Abdomen AP examination Antrophormic phantom PA Direct 6.0 EXPECTED OUTCOMES 1. The dosimetric dosimetric quantities for the establishment and use of guidance levels (diagnostic reference levels) based on TRS 457 for X200 Optimo mobile x-ray machine is applied and can be use as reference for the next study. 2. The measurement the backscatter factor, BSF values for kilovoltage x-ray beam for OPTIMA XR200 mobile x-ray using ionisation chamber, Gacfchromic XR-QA, EBT2 and EBT3 films. 3. The measurement values from diagnostic ionization chamber and film dosimetry for incident air kerma ( Ki)will be obtained and agreed with each other . 3.Comparison result the measurement of the Entrance Surface Air kerma ( Ke) using direct and indirect method using films dosimeter, TLD100 and TLD 100H for OPTIMA XR200 Mobile x-ray machine will agreed to the reference dosimeter (IC)and will be used as reference for next study. 7.0 References 1. International Atomic Licensing Energy, Dosimetry in Diagnostic Radiology: An International Code of Practise , Technical Reports Series no.457, IAEA, 2007. 2. Robin H, Brendan H, Lois H et al ( 2014), Advances in kilovolatge x-ray beam dosimetry, Phys.Med.Biol,59: 183-231. 3. Ahmed M, David RD, Donald ML, Hans MK (2010) Dosimetry in diagnostic radiology. European Journal of Radiology 76 :11-14 4. Smith L, Hill R, Nakano M, Kim J ( 2011), The measurement of backscatter factors of kilovoltage x-ray beams using Gafchromic EBT2 film, Autralas Phys Eng Sci Med 34:261-266. 5. Ma CM, Coffey CW, Dewerld LA et al (2001), AAPM protocol for 40–300 kV x-ray beam dosimetry in radiotherapy and radiobiology, Med. Phys. 28 (6). 6. International Commision on Radiation Units and Measurements ( 2005) , Appendix A: Backscattor Factors, Journal of the ICRO Vol 5 No 2 ,Report 74. 7. Gotanda T, Katsuda T, Gotanda R, Tabuchi A, Kuwano T et al (2009), Half value layer measurement for effective energy, using Radiochromic film and step shaped aluminium filter, IFMBE Proceedings 25/III, 58-61. 8. Chris J, Howard RE and Micheal AS (2012), Measurement of loe-energy backscatter factors using Gafchromic film and OSLDs, Journal of Applied Medical Physics, Vol.13, no.6. 9. Zainon R, Abu Talib NS. Abu Bakar SN , Aziz A (2014), Assessment and optimization of radiation dosimetry and image quality in x-ray radiographic imaging, Proceedings of World Congress on Engineering and Computer Science, Vol 1. 10. Rampado O.Garelli E,Deagostini S and Ropolo R (2006), Dose and energy dependence of response of Gafchromic XR-QA film for kilovoltage x-ray beams, Phys.med Biol. 51: 2871-2881. 11. Bradley PM, Micheal AS and Tine LP (2011), Calibration of Gachromic XR-RV3 radiochromic film for skin dose measurement using standardized x-ray spectra and a commercial flatbed scanner, 1920-1930. 12. Oliviera ML, Maia AF, Nascimento NCES et al (2012), Influence of thermoluminescent dosimeters energy dependence on the measurement of entrance skin dose in radiographic procedures, Radiol Bras, 43(2): 113-118. 13. Petoussi et al (1998), Calculation of backscatter factors for diagnostic radiology using Monte Carlo methods, hys. Med. Biol. 43:22-37.