Mental Health Needs Council
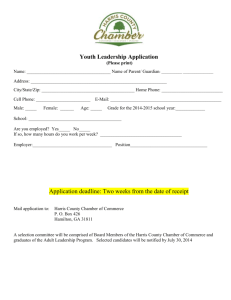
advertisement

Harris County’s population continues to increase and is projected to reach 4.5 million residents by 2020. Mental Illness In Harris County Prevalence Issues of Concern Recommendations Simultaneously, poverty level is estimated to increase from 12.5 percent up to 16 percent. Texas has the highest rate of medically uninsured citizens among the states. Harris County has the second highest rate of uninsured citizens among Texas counties. Texas is rated last in per capita mental health funding compared to other states. A Report of the Mental Health Needs Council, Inc. 2013 Mental Health Needs Council, Inc. P.O. Box 270205 Houston, Texas 77277-0205 (281) 575-9001 mhneedcl@hal-pc.org Harris County is ranked 30th out of 34 among local mental health authorities in per capita mental health funding. The shortfall in available mental health services for Harris County residents will only worsen as the population grows. PREVALENCE OF MENTAL ILLNESS IN CHILDREN AND ADOLESCENTS Of the 750,000 children and adolescents in Harris County between 6 and 18 years old (2010 Census), nearly 150,000 have a mental illness. Of those, 89,162 have a serious emotional disturbance. Approximately 19,300 children and adolescents with serious emotional disturbance needed services from the public mental health system in 2012, yet 74 percent (14,335) received none. Almost 69 percent of the 9,100 children referred to the Harris County Juvenile Probation Department have a diagnosable mental illness. Of those, 70 percent report cooccurring behavioral health problems of substance abuse and mental illness. About 41 percent have a history of trauma exposure, often having witnessed or experienced family or community violence. PREVALENCE OF MENTAL ILLNESS IN ADULTS Of the 2.9 million adults in Harris County (2010 Census), 496,358 have mental illness. Of those, 137,219 have severe and persistent mental illness (Major Depressive Disorder, Bipolar Disorder, or Schizophrenia). Of those with severe mental illness, 86,000 have no public (Medicaid or Medicare) or private health insurance and are totally dependent on the public mental health service system for treatment. In 2012, approximately 69,800 adults with severe mental illness were unable to access treatment from the public or private mental health systems. Of the Harris County citizens in jail, 24.1 percent have a current or past mental illness diagnosis. An estimated 15 percent of individuals with severe mental illness will be homeless at some point within the year. In the 2012 Point in Time Count of homeless persons in Harris County, 66 percent reported prior psychiatric hospitalization, needing mental health treatment, or having to leave their homes due to mental illness issues. In Harris County, 38,421 or 28 percent of adults with a severe mental illness report co-occurring substance abuse. ISSUES OF CONCERN Consequences of untreated mental illness may include school failure or dropout, juvenile or criminal justice involvement, victimization, acute psychiatric crises, unemployment, homelessness, or suicide. The limitations in the Harris County mental health service capability, especially outpatient services, have resulted in a dependence on crisis services. The Mental Health and Mental Retardation Authority (MHMRA) NeuroPsychiatric Center (NPC) currently treats over 13,000 crisis episodes per year. Demand for crisis services at NPC has frequently exceeded capacity, forcing the facility to close its doors to new admissions more than 75 times in 2012. Ben Taub General Hospital Emergency Room treated over 4000 with mental illnesses each year in 2011 and 2012. In 2012, around 250 were seen each month for psychiatric consultations. In 2012, almost 870 were admitted to psychiatric inpatient services at Ben Taub, up from about 850 in 2011. The number of mental illness-related calls received by the Houston Police Department Crisis Intervention Team increased from 10,800 in 2003, to 25,105 in 2010, to 24,771 in 2011, and over 27,000 calls in 2012. Of those individuals hospitalized in The University of Texas Harris County Psychiatric Center (UTHCPC), 22.6 percent were readmitted to inpatient services within one year. In 2012, about 70 children and 237 adults entered MHMRA services for the first time each month. An increasing number of children and adults, previously unknown to the public mental health system, request services each year. MHMRA’s waiting list for outpatient mental health services exceeds 1,600 adults each month. About 15 percent of those waiting for services deteriorate into crisis and require intervention at psychiatric emergency centers, inpatient hospitals, or in jail. At any given time, MHMRA provides services to 2,400 children and adolescents, 50 percent above its contracted, state-funded capacity. On average, 168 children and 326 adults were readmitted to MHMRA services each month in 2012. The Mental Health Needs Council is especially concerned with the following issues: Insufficient Funding for the Medically Uninsured More children and adults with severe mental illness reside in Harris County than any other Texas county, yet per capita funding is below the state average for public outpatient services. Reimbursement rates for public health care programs are so low that few private providers are willing to participate. The private and public sectors must collaborate in order to provide an adequate array of services and supports to address these needs. Limited Service Capacity Each month nearly 270 more individuals apply for public mental health services than can be served. As the population increases, there will be more. Access to service is even more limited to people without public or private insurance. Crisis Oriented System Due to significant funding limitations, children and adults without insurance receive few or no services, often resulting in decompensation into crises or incarceration. Emergency services can meet immediate needs, but cannot support long-term community stabilization. A larger, better funded, more responsive, and more accessible outpatient system would help to break the crisis-to-crisis cycle. Increasing numbers of children and adults with mental illness, whose illnesses are not severe enough to warrant inpatient or crisis care, are forced to wait for services until they are in crisis. Michael E. DeBakey Veterans Administration (VA) Medical Center Mental Health Services About half of the eligible returning Iraq and Afghanistan Veterans in America and the aging veteran population access mental health services from the VA. Suicide rates among active military and veterans have risen 80 percent since the start of the Iraq War. Fully 20 percent of US suicides are attributed to veterans. Support is lacking for spouses and children of veterans or active military. Federal budgetary support has so far funded the rising demand, although a collaborative public/private system may offer a better response in the future. Loss of Access to State Funded Inpatient Care Harris County has fewer than 10 psychiatric hospital beds per 100,000 residents, less than the national average of 17 per 100,000. Experts recommend adequate capacity at more than seven times current Harris County levels. Poor access to voluntary public psychiatric hospitalization causes increases in involuntary commitments. UTHCPC continues to be insufficiently funded to operate its 250 beds, thus curtailing capacity for more people to receive timely inpatient care. About 70 percent of Harris County’s allocated state hospital capacity goes to forensic cases. As a result, Harris County is pressured to provide inpatient services for voluntary and civil commitment cases. Less Access to Private Care At least 16 of Harris County’s private inpatient facilities have closed within the last 10 years, in part, due to restricted access to care for insured patients and failure to receive appropriate, timely reimbursement for insurance claims. Private psychiatric hospitals have suffered from an increasing burden of indigent care. Private hospitals often care for the medically indigent and should be commended for their contributions to the community. Children and adults who have psychiatric insurance benefits have difficulty accessing needed services due to shrinking provider rolls and professional workforce shortages. Lack of Access to Integrated Care Many children and adults with severe mental illnesses may abuse substances. Appropriate behavioral health care requires coordinated treatment for both problems, yet this is rarely available. People with serious mental illnesses have significantly shortened life expectancies and higher rates of metabolic disorders (e.g., diabetes, hypertension, or high cholesterol). Although coordinated health, mental health, and substance abuse services produce better health outcomes, these services are rarely available due to economic barriers for integrated care. Lack of Access to Residential Treatment and Housing Supports Many people with severe mental illnesses lose their jobs, family ties, and homes. At least 14,000 Harris County adults with a mental illness lack appropriate housing. Residential treatment services for children and adults with mental illness are in short supply. These are vital components of the mental health service continuum. Mental Health Workforce Portions of Harris County are designated as federal Mental Health (Professionals) Shortage Areas. Due to reductions in the capacity of training programs and continuing population growth, there are fewer psychiatrists, psychiatric nurses, social workers, and marriage and family therapists relative to the county population. The supply ratio of psychologists is only 60 percent of the national average. RECOMMENDATIONS The Governor of Texas, members of the Legislature, Harris County Commissioners Court, and the Health and Human Services Commission should: 1. Enhance Funding Under the Affordable Care Act, create coverage for the uninsured with adequate service packages and reimbursement rates. Expand the range of services and the reimbursement rates for an adequate array of supports to address clinical needs. Maintain a ‘safety net’ for those who need psychiatric services and are not covered by other funding sources. Establish mechanisms and procedures that promote, expedite, and maintain enrollment in CHIP and Medicaid programs. Align resources with the prevalence rates for mental disorders. 2. Expand Service Capacity Support a cost-effective public mental health system by sufficiently funding community-based Resiliency and Disease Management. Support the use of Medicaid 1115 Waiver projects to expand mental health services. Oppose supplanting current funding with Medicaid 1115 Waiver revenues. Authorize legislation to allow Local Mental Health Authorities to utilize state funds in support of uncompensated care and Medicaid 1115 Waiver projects, provided that contract performance targets are met. Expand public mental health capacity to serve all those with functional impairments due to a mental illness. Insure prompt, adequate Medicaid reimbursement. 3. Balance Resources Between Crisis Services and Ongoing Care Direct all additional mental health General Revenue dollars for outpatient services to minimize the need for crisis and inpatient care. Fund restoration and expansion of behavioral health services in public schools. Sufficiently fund Harris County's programs to divert people with mental illness from the juvenile and adult criminal justice systems. 4. Ensure Adequate Care for Iraq and Afghanistan Veterans Enhance and supplement federal (VA) initiatives to provide ongoing mental health support to returning veterans and their families. Explore public and private collaboration possibilities. 5. Expand Current Psychiatric Hospital Capacity Sufficiently fund public psychiatric hospitals for care of voluntary and civil commitments, as well as forensic cases. Sufficiently fund UTHCPC to operate at its full 250-bed capacity to locally treat Harris County citizens. 6. Support Indigent Care by Private Providers Support continuation of the STAR and STAR PLUS programs offering integrated medical and behavioral health to program participants. 7. Support Integrated Care for Individuals with Behavioral Disorders End discrimination for behavioral health (mental health and substance abuse) insurance coverage. Sufficiently fund collaborative and holistic rehabilitation services to address social, vocational, psychiatric, and health care needs. Fund electronic health records and health information exchanges to improve integrated health care, promote coordination of care, and reduce duplication of services. Support policies that promote collaborative health care and medical homes. 8. Prioritize Housing and Residential Services Sufficiently fund appropriate living options with supports tailored to clinical needs. 9. Support Professional Workforce Development Fund higher education programs that will increase the number of mental health professionals in the Texas workforce. Sufficiently fund mental health professional training programs, including psychiatry, psychology, social work, marriage and family therapists, and psychiatric nursing. Expand Medicaid reimbursement for mental health services provided by advanced professional trainees. Offer tuition forgiveness in return for public health service. 10. Support Local Control and Accountability for Public Mental Health Services Support accountability in service delivery to reduce costs, improve patient satisfaction, and produce improved patient outcomes.