Summary - Washington State Pharmacy Association
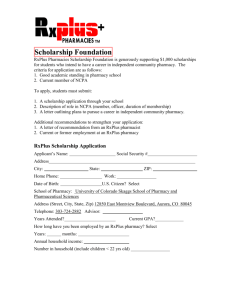
advertisement

Scope of Contemporary Pharmacy Practice: Roles, Responsibilities, and Functions of Pharmacists and Pharmacy Technicians-Executive Summary Nicole Paolini and Michael J. Rouse This is the executive summary of an article commissioned by the Council on Credentialing in Pharmacy (CCP), which provides an overview of current pharmacy practice, its range of services, and the role of pharmacy technicians. The complete article is available open access at www.pharmacycredentialing.org/ccp/Contemporary_Pharmacy_Practice.pdf. Pharmacy practice is evolving from primarily supervising medication distribution to providing medication therapy management and disease prevention services. The settings in which pharmacists now practice include community pharmacies, ambulatory care clinics, hospitals and health systems, long-term care facilities, home care agencies, and managed-care organizations. Other settings include the pharmaceutical industry, research, government, academia, professional associations, and poison information centers. This scope of practice and the complexity of the medications managed within each practice require a workforce that is diverse in knowledge, competently trained, and appropriately credentialed and that demonstrates professional judgment, values, and attitudes. Health care delivery in the United States In the United States, pharmacists constitute the third largest group of health professionals, after physicians and nurses, 1, 2 and have been rated the most trustworthy and accessible.3, 4 However, health-system resources are stretched and, overall, not efficiently utilized. The number of errors (including medication errors) increases as patients encounter multiple providers and multiple levels of care. In addition, many new therapies require intensive monitoring and are extremely individualized. Also, patients must be competent to access available pharmaceutical information. Also, patients from different backgrounds have different perceptions of their disease and medications, which affect their treatment outcomes. Medication therapy management is a partnership of the pharmacist, the patient or caregiver, and other health professionals to promote the optimal use of medications. As the pharmacist obtains accurate disease and medication histories, he or she achieves an understanding of the primary medical problem, co-morbidities, and pharmacologic effects of the patient's medication regimen. Training and credentialing Today, pharmacists' education revolves around three broad outcomes: patient care, systems management, and public health. Since 2000, Doctor of Pharmacy (PharmD) students are required to complete at least six years of postsecondary education, up from the five years required previously. This change allows increased clinical training, ensuring that pharmacists are appropriately prepared to collaborate with physicians, nurses, and other health care professionals. These three main outcomes align with the five core competencies identified by the Institute of Medicine: (1) delivering patient-centered care, (2) working as a part of interprofessional teams, (3) practicing evidence-based medicine, (4) focusing on quality improvement, and (5) using information technology. 5 To maintain and advance these outcomes and competencies, postlicensure training opportunities for pharmacists have expanded dramatically in the past few decades. Postlicensure training programs and credentials are (1) competency-based, (2) developed on the basis of comprehensive task analysis in the relevant areas, and (3) accredited by organizations to assure quality, validity, and integrity. Postgraduate year 1 residencies focus on managing medication use for a range of diseases. Postgraduate year 2 residencies focus on specialized practice and more in-depth training. Specialty board certification can be obtained in five areas: nuclear pharmacy, nutrition support pharmacy, oncology pharmacy, pharmacotherapy, and psychiatric pharmacy. Other pharmacyspecific and multidisciplinary credentials are offered to pharmacists, such as, Certified Geriatric Pharmacist (CGP), Certified Diabetes Educator (CDE), and Certified Anticoagulation Care Provider (CACP). Domains of pharmacy practice Most pharmacists work in patient care settings. The services provided by pharmacists in such settings - the focus of this paper can be further differentiated by the scope and complexity of care provided, reflecting different societal needs for pharmacy services. The majority of pharmacists in patient care roles can be described as "generalist practitioners;" they serve a wide variety of patients with medical needs ranging from minor ailments to more complex conditions. Their typical practice settings are community and hospital pharmacies.6-9 Pharmacists can also focus their practice on a specific therapeutic area (e.g., diabetes, thrombotic disease), patient population (e.g., pediatrics or geriatrics), or specialized practice (e.g., compounding pharmacy). Pharmacists with such additional training are competent in assessing medically complex patients, developing individualized regimens, and monitoring responses to optimize outcomes. Pharmacotherapy specialists, for example, are responsible for providing direct patient care at an advanced level, often in a multidisciplinary team. They serve specific patient populations and manage complex therapies, diagnostic agents, and technologies. Pharmacists practice in many nontraditional settings as well, including managed care organizations, patient call centers, hospice, drug and poison information services, as information technology specialists, in academia, health organization management, regulatory oversight, pharmacy organizations, and industry. Pharmacy technicians In recent years, states have expanded the scope of practice and responsibilities of pharmacy technicians and now require technicians to have more extensive training. Pharmacy technicians work in community pharmacies, hospitals, the armed forces, home health care, long-term-care facilities, prescription mail-order services, managed health care facilities, and educational or training programs. New responsibilities include handling restricted, investigational, and chemotherapy drugs and increased involvement in third-party payment. Summary The evolution in pharmacy practice has presented opportunities for pharmacists to perform nontraditional services. New postlicensure training and credentials support and enhance the competence of practitioners. New roles and responsibilities for pharmacy technicians allow them to better support pharmacists in the delivery of pharmacy services. CCP presents this material to describe where pharmacy is today and what pharmacy practice will look like in the future. Acknowledgments Nicole Paolini, Pharm.D., CDE, is Clinical Assistant Professor, School of Pharmacy and Pharmaceutical Sciences, University at Buffalo, Buffalo, NY. Michael J. Rouse, B.Pharm. (Hons), M.P.S., is Assistant Executive Director, International and Professional Affairs, Accreditation Council for Pharmacy Education, Chicago, IL. References 1. 2. 3. 4. 5. 6. 7. 8. 9. Bureau of Labor Statistics. Occupational employment statistics, 29-1051 pharmacists. www.bls.gov/oes/2007/may/oes291051.htm (accessed Dec 30, 2008). Bureau of Labor Statistics. Occupational outlook handbook, 2008-9 edition. www.bls.gov/oco/ocos079.htm (accessed Jan 22, 2008). Jones JM. Lobbyists debut at bottom of honesty and ethics list. www.gallup.com/poll/103123/Lobbyist-DebutBottom-Honesty-ethics-List.aspx (accessed Dec 30, 2008). Carter BL, Elliott WJ. The role of pharmacists in the detection, management, and control of hypertension: a national call to action. Pharmacotherapy. 2000;20:119-22. Greiner AC, Knebel E, eds. Health professions education: a bridge to quality. Washington, DC: National Academies Press. 2003:45-74. Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533543. Pharmacy: A report to the Nuffield Foundation. London: Nuffield Foundation 1986. Hawksworth GM, Chrystyn H. Clinical pharmacy in primary care. Br J Clin Pharmacol. 1998;46:415-420. Manasse, Jr. HR, Speedie MK. Pharmacists, pharmaceuticals, and policy issues shaping the workforce in pharmacy. Am J Health-Syst Pharm. 2007;64:e30-48. Address correspondence to Marissa Schlaifer, B.S.Pharm., M.S., Secretary/Treasurer, Council on Credentialing in Pharmacy, c/o Academy of Managed Care Pharmacy, 100 North Pitt Street, Suite 400, Alexandria, VA 22314. Curtis L. Mattson, B.A., M.Div., is acknowledged for his contribution to this document. Other contributions are noted in the full paper, available at www.pharmacycredentialing.org/ccp/Contemporary_Pharmacy_Practice.pdf. The authors have declared no potential conflicts of interest.