NickBurgess_79_20130610185714
advertisement
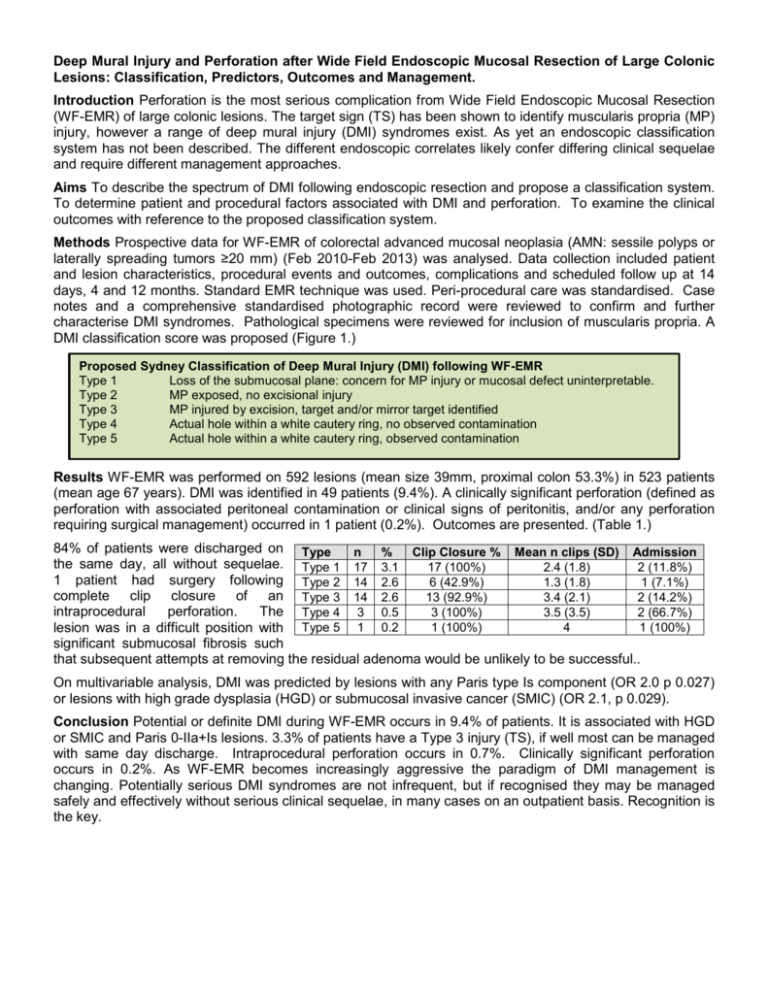
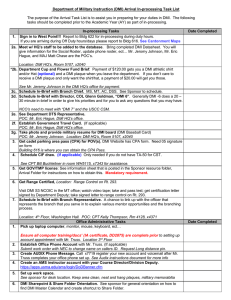
Deep Mural Injury and Perforation after Wide Field Endoscopic Mucosal Resection of Large Colonic Lesions: Classification, Predictors, Outcomes and Management. Introduction Perforation is the most serious complication from Wide Field Endoscopic Mucosal Resection (WF-EMR) of large colonic lesions. The target sign (TS) has been shown to identify muscularis propria (MP) injury, however a range of deep mural injury (DMI) syndromes exist. As yet an endoscopic classification system has not been described. The different endoscopic correlates likely confer differing clinical sequelae and require different management approaches. Aims To describe the spectrum of DMI following endoscopic resection and propose a classification system. To determine patient and procedural factors associated with DMI and perforation. To examine the clinical outcomes with reference to the proposed classification system. Methods Prospective data for WF-EMR of colorectal advanced mucosal neoplasia (AMN: sessile polyps or laterally spreading tumors ≥20 mm) (Feb 2010-Feb 2013) was analysed. Data collection included patient and lesion characteristics, procedural events and outcomes, complications and scheduled follow up at 14 days, 4 and 12 months. Standard EMR technique was used. Peri-procedural care was standardised. Case notes and a comprehensive standardised photographic record were reviewed to confirm and further characterise DMI syndromes. Pathological specimens were reviewed for inclusion of muscularis propria. A DMI classification score was proposed (Figure 1.) Proposed Sydney Classification of Deep Mural Injury (DMI) following WF-EMR Type 1 Loss of the submucosal plane: concern for MP injury or mucosal defect uninterpretable. Type 2 MP exposed, no excisional injury Type 3 MP injured by excision, target and/or mirror target identified Type 4 Actual hole within a white cautery ring, no observed contamination Type 5 Actual hole within a white cautery ring, observed contamination Results WF-EMR was performed on 592 lesions (mean size 39mm, proximal colon 53.3%) in 523 patients (mean age 67 years). DMI was identified in 49 patients (9.4%). A clinically significant perforation (defined as perforation with associated peritoneal contamination or clinical signs of peritonitis, and/or any perforation requiring surgical management) occurred in 1 patient (0.2%). Outcomes are presented. (Table 1.) 84% of patients were discharged on Type n % Clip Closure % Mean n clips (SD) Admission the same day, all without sequelae. Type 1 17 3.1 17 (100%) 2.4 (1.8) 2 (11.8%) 1 patient had surgery following Type 2 14 2.6 6 (42.9%) 1.3 (1.8) 1 (7.1%) complete clip closure of an Type 3 14 2.6 13 (92.9%) 3.4 (2.1) 2 (14.2%) intraprocedural perforation. The Type 4 3 0.5 3 (100%) 3.5 (3.5) 2 (66.7%) Type 5 1 0.2 1 (100%) 4 1 (100%) lesion was in a difficult position with significant submucosal fibrosis such that subsequent attempts at removing the residual adenoma would be unlikely to be successful.. On multivariable analysis, DMI was predicted by lesions with any Paris type Is component (OR 2.0 p 0.027) or lesions with high grade dysplasia (HGD) or submucosal invasive cancer (SMIC) (OR 2.1, p 0.029). Conclusion Potential or definite DMI during WF-EMR occurs in 9.4% of patients. It is associated with HGD or SMIC and Paris 0-IIa+Is lesions. 3.3% of patients have a Type 3 injury (TS), if well most can be managed with same day discharge. Intraprocedural perforation occurs in 0.7%. Clinically significant perforation occurs in 0.2%. As WF-EMR becomes increasingly aggressive the paradigm of DMI management is changing. Potentially serious DMI syndromes are not infrequent, but if recognised they may be managed safely and effectively without serious clinical sequelae, in many cases on an outpatient basis. Recognition is the key.