ONLINE SUPPLEMENT Extra-Renal Atherosclerotic Disease Blunts
advertisement

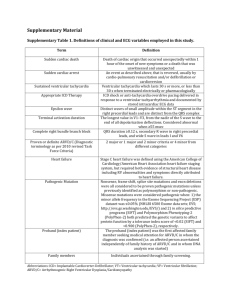
1 ONLINE SUPPLEMENT Extra-Renal Atherosclerotic Disease Blunts Renal Recovery in patients with Renovascular Hypertension 2 METHODS: Patient selection and data collection: Subjects with atherosclerotic renovascular disease (ARVD) were identified from Mayo Clinic Radiology database, which includes patients who had agreed to have their data used for research purposes. From this database, we selected ARVD patients who were seen at Mayo Clinic, Rochester, MN between January 1, 2004 and August 31, 2012 and had an echocardiogram done within a 2-year period. Imaging criteria for diagnosis of hemodynamically significant renal artery stenosis included renal artery Doppler ultrasound velocity acceleration (peak systolic velocity >200 cm/s), or magnetic resonance (MR) /computed tomography (CT) angiography with evident stenosis >60% and/or post-stenotic dilation (1). Individuals were excluded from study if they had: 1) End stage renal disease (ESRD), on chronic maintenance dialysis at the time of entry into the study 2) History of solid organ transplantation 3) Significant valvular heart disease 4) History of pregnancy in past 12 months and (5) If no follow up data was available post revascularization. Clinical parameters: The Modification in Diet in Renal Disease (MDRD) equation was used to calculate estimated glomerular filtration rate (eGFR, mL/min per 1.73 m2) as: 175 x SCr (exp[-1.154]) x Age (exp[0.203])x (0.742 if female) x (1.21 if black) (2). Cardiac outcomes were obtained from the echocardiography database. Echocardiographic parameters: Left ventricular mass index (LVMI) was determined using the American Society of Echocardiography-recommended formula (3) (4). LV relative wall thickness (RWT) was calculated as (2*PWTd)/LVIDd, where PWTd is the posterior wall thickness and LVIDd, the LV internal diameter at end diastole (5) (6). Cardiac geometry was classified as follows: i) Normal: LVMI ≤ 95 g/m2 in women or ≤ 115 g/m2 in men and RWT ≤ 0.42; ii) Concentric remodeling: LVMI ≤ 95 g/m2 in women or ≤ 115 g/m2 in men and RWT > 0.42; iii) Eccentric hypertrophy: 3 LVMI > 95 g/m2 in women or > 115 g/m2 in men and RWT ≤ 0.42; or iv) Concentric hypertrophy: LVMI > 95 g/m2 in women or > 115 g/m2 in men and RWT > 0.42 (5) (6). Left atrial volume was measured off-line using the biplane area-length method (5). All of the volume measurements were indexed to body surface area. Diastolic function was graded as normal; grade I (mild dysfunction): delayed relaxation mitral inflow pattern, mitral E/A ratio <0.8, predominant systolic flow in the pulmonary venous flow (S>D), annular e' <8 cm/s (septal and lateral), and E/e' ratio <8 (septal and lateral)); grade II (moderate dysfunction): pseudo-normal mitral inflow pattern, mitral E/A ratio ≥1, and average E/e' ratio (septal and lateral) is >10) or grade III (severe diastolic dysfunction): restrictive mitral inflow pattern, E/A ratio ≥2, deceleration times (DT) <160 ms, isovolumetric relaxation period (IVRT) ≤60 ms, systolic filling fraction ≤40 percent, and average E/e' ratio ≥13)(7-9). Statistical analysis: The Shapiro-Wilk test was used to test for deviation from normality. Normally distributed data are expressed as mean ± standard deviation. Median and interquartile range (IQR) are used for non-normally distributed data. Final outcomes were adjusted for gender, baseline blood pressure, HDL, LDL cholesterol levels, Diabetes Mellitus, peripheral artery disease, cerebrovascular disease, and family history of coronary artery disease, statin use, number of anti-hypertensive medications, baseline serum creatinine; and left ventricular ejection fraction (differences that were statistically significant among the groups). Results: In order to evaluate the effects of additional vascular diseases, we studied revascularization outcomes in ARVD patients with and without diabetes mellitus (Table-1s), cerebrovascular (Table-2s), or peripheral vascular disease (Table-3s). These comorbidities were also associated with negatives outcomes, suggesting involvement of diffuse atherosclerosis. A relatively small number of ARVD patients with diabetes mellitus may account for the greater decline in systolic blood pressure compared to ARVD patients without diabetes. 4 Figure legend: Figure-1s-One-year outcomes post-revascularization of ARVD based on (A) presence (ARVDDM) or absence (ARVD) of diabetes mellitus (B) presence (ARVD-PAD) or absence (ARVD) of peripheral arterial disease; (C) presence (ARVD-CVD) or absence (ARVD) of cerebrovascular disease. Psys, mean change in systolic blood pressure; Pdia, mean change in diastolic blood pressure; SCR, median change in serum creatinine; GFR,median change in eGFR; and Uprot, median change in proteinuria excretion. * P<0.05 after adjustment for clinically significant variables including gender, baseline blood pressure and renal function. Details are provided in the supplementary material (Table-1s-3s). 5 Table-1s. One-year outcomes post-revascularization of ARVD based on presence (ARVDDM) or absence (ARVD) of Diabetes. ARVD-DM ARVD (N=36) (N=95) Unadjusted P value Adjusted* P value 141±21** 140±15 0.76 0.0033 -9.8±23 -5±25 0.33 <.0001 66±14** 67±11** 0.91 0.016 -6.9±15 -6±15 0.73 <.0001 1.5(0.74.8)** 1.3(0.7-8.6) 0.16 <.0001 0.1(-1-+1.7) 0(-1.0-+7.1) 0.59 0.07 42(12-85) 46(4.5-82) 0.19 <.0001 -4.2(-29-+38) -0.4(-38+46.7) 0.10 0.077 180(281064) 124(213707) 0.79 0.13 -27(-1880+737) 6(-1000+2862) 0.12 0.46 Outcomes Systolic blood pressure (mmHg) Δchange(mmHg) Diastolic blood pressure (mmHg) Δchange(mmHg) Serum creatinine(mg/dl) Δchange(mg/dl) eGFR(ml/min/1.73m²) Δchange(ml/min/1.73m²) Proteinuria(mg/dl) Δchange(mg/dl) eGFR, estimated glomerular filtration rate.*after adjustment for gender, baseline blood pressure, HDL, LDL cholesterol levels, peripheral artery disease, cerebrovascular disease, Coronary artery disease (CAD), family history of CAD, statin use, number of anti-hypertensive medications, baseline serum creatinine; and left ventricular ejection fraction in a multivariate model. **P<0.05 vs. pre-revascularization. Data are presented as Median (range), N (%), or Mean ±SD; as appropriate. 6 Table-2s. One-year outcomes post-revascularization of ARVD based on presence (ARVDCVD) or absence (ARVD) of Cerebrovascular disease. ARVD-CVD ARVD (N=68) Systolic blood pressure (mmHg) Δchange(mmHg) (N=63) Unadjusted P value Adjusted* P value 142±16 140±18** 0.32 0.0025 -4.5±26 -8±23 0.39 <.0001 66±13** 66±11** 0.97 0.009 -4.1±14 -8±16 0.12 <.0001 1.4(0.78.6)** 1.2(0.7-4.4) 0.24 0.006 0.1(-0.7+7.1) 0(-1.2-+1.3) 0.10 0.03 43(4.5-83)** 46(13-85) 0.29 0.0044 -3.3(-29+29) -0.4(-38+46.7) 0.20 0.09 193(213707) 98(31-1381) 0.08 0.26 13(-1880+2862) -8(-729+194) 0.16 0.39 Outcomes Diastolic blood pressure (mmHg) Δchange(mmHg) Serum creatinine(mg/dl) Δchange(mg/dl) eGFR(ml/min/1.73m²) Δchange(ml/min/1.73m²) Proteinuria(mg/dl) Δchange(mg/dl) eGFR, estimated glomerular filtration rate.*after adjustment for gender, baseline blood pressure, HDL, LDL cholesterol levels, Diabetes Mellitus, peripheral artery disease, coronary artery disease (CAD), family history of CAD, statin use, number of anti-hypertensive medications, baseline serum creatinine; and left ventricular ejection fraction in a multivariate model. **P<0.05 vs. pre-revascularization. Data are presented as Median (range), N (%), or Mean ±SD; as appropriate. 7 Table-3s. One-year outcomes post-revascularization of ARVD based on presence (ARVDPAD) or absence (ARVD) of Peripheral artery disease. ARVD-PAD ARVD (N=45) Systolic blood pressure (mmHg) Δchange(mmHg) (N=86) Unadjusted P value Adjusted* P value 142±18 140±17** 0.64 0.0041 -4.7±28 -7±23 0.61 <.0001 66±14 67±11** 0.84 0.014 -4.6±15 -7±15 0.40 <.0001 1.4(0.98.6)** 1.2(0.7-4.4) 0.16 0.009 0.1(-1-+7.1) 0(-1.2-+2.1) 0.21 0.04 42(5-81) 47(11-85) 0.08 0.006 -3.2(-29+47) -0.6(-38+37.8) 0.78 0.12 226(371644) 106(213707) 0.48 0.33 12(-1880+1187) 0(-1000+2862) 0.68 0.43 Outcomes Diastolic blood pressure (mmHg) Δchange(mmHg) Serum creatinine(mg/dl) Δchange(mg/dl) eGFR(ml/min/1.73m²) Δchange(ml/min/1.73m²) Proteinuria(mg/dl) Δchange(mg/dl) eGFR, estimated glomerular filtration rate.*after adjustment for gender, baseline blood pressure, HDL, LDL cholesterol levels, Diabetes Mellitus, cerebrovascular disease, coronary artery disease (CAD), family history of CAD, statin use, number of anti-hypertensive medications, baseline serum creatinine; and left ventricular ejection fraction in a multivariate model. **P<0.05 vs. pre-revascularization. Data are presented as Median (range), N (%), or Mean ±SD; as appropriate. 8 References: 1. Murphy TP, Cooper CJ, Dworkin LD, Henrich WL, Rundback JH, Matsumoto AH, et al. The Cardiovascular Outcomes with Renal Atherosclerotic Lesions (CORAL) study: rationale and methods. J Vasc Interv Radiol. 2005 Oct;16(10):1295-300. 2. Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function--measured and estimated glomerular filtration rate. N Engl J Med. 2006 Jun 8;354(23):2473-83. 3. Matavelli LC, Huang J, Siragy HM. Angiotensin AT(2) receptor stimulation inhibits early renal inflammation in renovascular hypertension. Hypertension. 2011 Feb;57(2):308-13. 4. Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002 Jan 16;39(2):257-65. 5. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005 Dec;18(12):144063. 6. Lam CS, Grewal J, Borlaug BA, Ommen SR, Kane GC, McCully RB, Pellikka PA. Size, shape, and stamina: the impact of left ventricular geometry on exercise capacity. Hypertension. 2010 May;55(5):1143-9. 7. Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009 Mar;10(2):165-93. 9 8. Moller JE, Pellikka PA, Hillis GS, Oh JK. Prognostic importance of diastolic function and filling pressure in patients with acute myocardial infarction. Circulation. 2006 Aug 1;114(5):43844. 9. Gilman G, Nelson TA, Hansen WH, Khandheria BK, Ommen SR. Diastolic function: a sonographer's approach to the essential echocardiographic measurements of left ventricular diastolic function. J Am Soc Echocardiogr. 2007 Feb;20(2):199-209.