Counties Manukau Smokefree 2025 Initiative
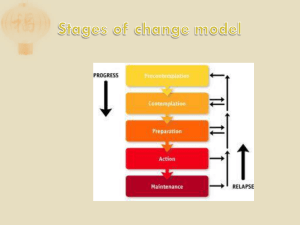
advertisement
Counties Manukau Smokefree 2025 Initiative 3 Year Plan (Years 3-5) July 2015 – June 2018 Final plan for submission to Ministry of Health, 27 May 2015. Plan is yet to be submitted for internal approval at CM Health. Linkages CM Health Annual Plan 2015/16 Maaori Health Plan 2015/16 ARPHS Annual Operating Plan 2015/16 Page 1 of 35 Contents Key Highlights....................................................................................................................................................... 3 Introduction ......................................................................................................................................................... 3 CM Health Smoking Population ........................................................................................................................... 4 Current Services ................................................................................................................................................. 10 Summary of achievements Years 1-2................................................................................................................. 20 Year 3-5 Plan ...................................................................................................................................................... 23 Reference Documents........................................................................................................................................ 33 Appendix One: Road Map - Smokefree Aotearoa 2025..................................................................................... 34 Page 2 of 35 Key Highlights This plan covers Years 3-5 of the Counties Manukau Smokefree 2025 Initiative, which is a five year initiative from 2013-18. There are an estimated 62,000 people who smoke in the Counties Manukau district. Approximately one-third are Maaori, and one-third are Pacific, with the remainder being NZ European/Other and Asian. Smoking disproportionately affects certain groups in Counties Manukau, and on this basis the following priority groups have been identified: o Maaori o Pacific o Pregnant women and their families o People with mental illness and/or other addictions o People with chronic conditions o Younger age groups (15-49 year olds overall, and 20-34 year olds specifically) o Manurewa, Papakura and Mangere/Otara localities. Years 1-2 have already seen a number of significant activities take place in line with our goal to achieve a Smokefree district by 2025, and to better meet the needs of the identified priority groups. These are based on the extensive needs analysis process that has taken place to date. Achieving the initiative’s interim target of 12% prevalence by 2018 (and 18% for Maaori) will require an additional 4,200 people to quit smoking and stay smokefree per year on top of the current steady state. This requires a dramatic shift in Smokefree activity, and necessitates that we identify effective new approaches that work to reduce smoking prevalence amongst our priority communities on a larger scale. In the short-term this has meant realigning our DHB resource to focus across the health system and community, working to strengthen our core business, such as improving access to cessation support within health target activity, identifying and responding to gaps such as provision for people with mental illness and/or addictions, and retendering our community-based smoking cessation services to identify innovative service delivery models with increased volumes and greater reach to priority populations. It has also meant identifying new ways of gathering insights into our smoking population, In the medium to long-term we need to continue to strengthen our core activity, as well as identify, test and evaluate new approaches that contribute to a reduction in smoking prevalence amongst priority communities. We must continually evaluate our progress and use this to inform ongoing activity. Introduction In late 2012 the Counties Manukau Health Executive Leadership Team and Board endorsed Smokefree as a key population health priority area for the next five years, and endorsed the strategic approach to achieve a Smokefree Counties Manukau by 2025. This is defined as 5% smoking prevalence or less, across all groups. A five year initiative was committed to with an interim target of achieving 12% prevalence or less by 2018, and a halving of prevalence for Maaori and Pacific communities1. Annual plans2 were developed and implemented for Year One and Year Two of this five year strategy, following extensive consultation within Counties Manukau Health and with our communities. This plan describes the approach CM Health intends to take for the remaining three years of the five year strategy (July 2015 to June 2018). Counties Manukau Health is committed to achieving a smokefree district by 2025. Therefore it is anticipated that a subsequent plan will be developed to cover the period 2018 to 2025. 1 Based on updated smoking prevalence from Census 2013 data, this now equates to 18% for Maaori and 12% for Pacific (which brings the Pacific target in line with that for the overall population). 2 Copies of these plans are available from the CM Health Smokefree Service. Page 3 of 35 CM Health Smoking Population Demographic characteristics Census data released in late 2013 demonstrated a significant reduction in smoking prevalence from 2006 levels for the overall Counties Manukau population, and for Maaori and Pacific peoples, who have the highest smoking rates in our rohe. Table One: Smoking prevalence in Counties Manukau (total response ethnicity) Census 2006 Census 2013 National 2013 Overall* 22.1% 15.9% 15.0% Maaori 46.8% 36.0% 32.7% Pacific 30.3% 23.2% 23.2% *NB. The overall column here avoids double counting, which is possible for people who report both Maaori and Pacific ethnic groups. As at Census 2013, Counties Manukau had an estimated currently smoking population of 62,000 people (15.9%). This figure is calculated from applying the census usually resident population prevalence of regular smoking to the absolute number of people who are estimated residents in CM Health in 2013. In order to achieve the 2018 target, an estimated 4,200 extra people need to quit and stay smokefree per year on top of those already quitting. Maaori and Pacific comprise almost one-third each of the smoking population, with NZ European/Other groups comprising almost onethird, and an estimated one-tenth identified as people of Asian ethnicities. CM Health has undertaken extensive demographic analysis of our currently smoking population. A high level overview of the key themes is presented below. Full details can be found by consulting Reference documents 9,15 and 16. Based on this analysis, we have prioritised the following groups and localities for our smokefree activity. Maaori whaanau/ communities 1/3rd of smoking population (est. 19,000) Pacific families/ communities 1/3rd of smoking population (est. 18,000) Pregnant women and whaanau Est. 1,700 per year 51% prevalence amongst Maaori women in 2013 People with mental illness and addictions Est. 8-15% of our smoking population (MH specialist services clients alone) Younger age groups (20-34 year olds particularly, and 15-49 year olds overall) Manurewa 21% of all CM smokers Mangere/Otara/Papatoetoe Highest proportion of Maaori that smoke Highest proportion of Pacific that smoke 33% of all CM smokers Other areas with high Maaori and/or Pacific populations and prevalence (e.g. Papakura) Note that due to availability of Census 2013 data we have used Local Board areas rather than DHB service localities for geographical priority areas. A further priority group are people with long-term (physical health) conditions, for whom it may be reasonable to assume a higher proportion smoke or are recent ex-smokers, due to the presence of a smoking-related condition. This group will also be important influencers for their family members, who may already smoke or be susceptible to starting. It will be important to reach this group in addition to the younger age groups identified above, both in order to achieve the Smokefree 2025 vision, and to contribute to both short and long-term impacts in the health system. Page 4 of 35 Smoking prevalence peaks between the ages of 25-29 for Maaori and Pacific, as well as the Counties Manukau population overall. 40% of Maaori and 45% of Pacific who smoke are aged 20-29. The large majority of Maaori and Pacific who smoke are aged 15-49 (82% and 83% respectively). Overall, Maaori women in Counties Manukau are more likely to smoke than men (37.7% compared to 33.7%). Whilst smoking prevalence peaks (over 40%) at age 25-29 for both Maaori women and men, this peak continues through to age 50-54 for women whereas it drops below 40% for men from the age of 35. The opposite is true for Pacific peoples, with Pacific men being more likely to smoke than Pacific women (26.3% compared to 19.1% overall). However, there are variances between different Pacific ethnicities, and both Cook Island women and men have high rates of smoking (30.5% and 30.1% respectively). The greatest number of Pacific people who smoke are Samoan (estimated 7,000 people), followed by Cook Island Maaori (estimated 4,350 people), Tongan (estimated 3,000) and Niuean (1,500 people). There are very small numbers of people who smoke from other Pacific ethnicities (Fijian, Tokelauan, Kiribati, Tuvaluan, Other; each less than an estimated 240 people). Smoking Prevalence by Ethnicity (Census 2013) The Manurewa, Mangere/Otara/Papatoetoe and Papakura localities have been identified as priority localities for all smokefree activity because they have: Page 5 of 35 Higher smoking prevalence overall, and higher smoking prevalence for Maaori and Pacific compared to other localities A high proportion of Maaori and/or Pacific people who smoke A high number of Maaori and/or Pacific people who smoke. Estimated Smoking Prevalence and Number of People Who Smoke by Local Board Table Two: Local board smoking prevalence by ethnic group Mangere 37% 23% 8% European/ Other 15% Otara-Papatoetoe 39% 23% 7% 16% 19% Manurewa 39% 23% 6% 15% 21% Papakura 40% 23% 5% 17% 21% Howick 22% 16% 6% 9% 9% Franklin 30% 18% 4% 12% 14% Table Three: Local board as % of ethnic group population in CM who smoke Maaori % of Maaori Pacific Asian % of Pacific % of Asian % of European/ Other Total 22% % Total Mangere 13% 34% 8% 4% 15% Otara-Papatoetoe 18% 32% 21% 8% 18% Manurewa 30% 23% 13% 14% 21% Papakura 19% 5% 4% 16% 13% Howick 6% 4% 47% 26% 17% Franklin 14% 2% 3% 31% 16% Page 6 of 35 Table Four: Local board estimated population who smoke by ethnicity 2013 Mangere Maaori Pacific Asian European/ Other Total 2,300 5,300 500 1,000 9,200 Otara-Papatoetoe 3,200 5,100 1,300 1,700 11,300 Manurewa 5,500 3,700 800 3,200 13,200 Papakura 3,400 800 200 3,500 8,000 Howick 1,100 600 2,800 5,800 10,300 Franklin 2,500 300 150 6,900 10,000 The priority groups identified above are not discrete groups, and there will be much overlap between them. This means there is considerable potential to reach people who belong to more than one of the identified priority groups (e.g. young pregnant Maaori women and their whaanau who live in Papakura or Pacific families who live in Mangere and have a range of health needs). This means we need to develop smart strategies that can cater to multiple groups at once. It also means that we need to work closely with our partners in the health system and with other stakeholders who already work with these groups. Smoking status by deprivation, nicotine replacement and secondary care use. An analysis was conducted of the health contact population (population recorded in health records, close to census estimates) in CM Health in 2013, aged 15 to 74 years, who were alive at the start of 2013, as part of an investigation into factors associated with receiving NRT cessation support in 2013. An NMDS hospital discharge record in the last 5 years consistent with current smoking identified 15.3% (55,946/366,662) of the health contact population as likely current smokers. The population who had smoked in the last 5 years (n=55,946) were further divided into those who had not used nicotine replacement therapy (NRT) in the last five years (n=41,679) and those who had used these treatments (n=14,267), since current NRT use was strongly (odds ratio ~6) related to past use of the drug. Of the larger group who had not used NRT in the past five years, 60% (n=24,498) were living in an address coded as the most deprived quintile (NZdep2013). This is compared to about 45% of the total CM Health population. In addition, 14.5% (n=6,057) of the 41,679 were also likely to have diabetes, based on their records of drug use, outpatient visits, and hospital diagnosis information. In the group who had not used NRT in the last 5 years (41,679), about 3% (1,513) used NRT sometime in 2013. In a regression analysis, low use of NRT was strongly associated with Pacific ethnic group (compared to NZ European and other), socioeconomic status and older age groups. Overall, living in an area of high socioeconomic deprivation (NZDep2013 deciles 7 to 10, compared to deciles 1 and 2) was responsible for the greatest burden of low NRT use (33%) in a population attributable risk analysis. Pacific ethnicity was associated with 16% of this burden. 3 Burden of disease and costs In New Zealand, tobacco use has been estimated to account for 9.1% of health loss from all causes between 2006 and 2014.4 It was further estimated that tobacco was associated with 40% of health loss from cancer (mainly lung) and 26% of the burden of vascular disorders and diabetes. Of all the district health boards in the country, CM Health has the third highest total number of adults (aged between 30 and 79 years, alive in 2009 and 2010, with a historic record of CVD event in the period 2000 to 2010), of all the DHBs (n=2,942).5 Given the high prevalence of smoking in CM Health, compared to the national average (Table one), the burden of disease and costs of healthcare in CM Health associated with smoking are likely to be higher than national estimates. 3 Thornley S. Characteristics of people using pharmaceutical aids to quit smoking in Counties Manukau Health, 2015. Unpublished manuscript. 4 Ministry of Health. 2013. Health Loss in New Zealand: A report from the New Zealand Burden of Diseases, Injuries and Risk Factors Study, 2006–2016. Wellington: Ministry of Health. 5 Webpage: http://www.hqsc.govt.nz/assets/Health-Quality-Evaluation/Atlas/CVD_standard/atlas.html; accessed 19/5/2015. Page 7 of 35 We have not directly calculated the financial costs of healthcare in CM Health, since this would be a very large project to undertake. Since smoking is associated with about 10% of premature death and disability, it is also likely to entail a similar proportion of healthcare costs. As an example of the estimated costs of a condition very strongly related to tobacco smoking, we refer to a publication which estimated, from hospital records in the 2012/13 financial year, the direct costs of chronic obstructive pulmonary disease, by DHB. 6 The annual costs were calculated at NZ$6.14 million for CM Health. This was second only to Canterbury, and higher than the costs estimated for Waitemata (NZ$5.76 million), which has a larger total adult population than CM Health. This is likely due to the age-standardised rate of hospital admission for Maaori and Pacific people being almost twice that for NZ European and other ethnic groups, and CM Health having a much higher proportion of our population identifying as Maaori and Pacific. Estimate of total numbers of smokers helped to quit smoking per annum. An analysis of 2013 NRT use showed that about 11,000 people per year are receiving cessation support which includes this medication, from all sources, in 2013. Using the Ministry’s estimate of 10% quit success, this suggests that, at present about 1,100 people are quitting long term in CM Health each year. The figure may be significantly higher, as some people will opt to quit cold turkey, after NRT is offered, and some smokers will quit unsupported. Quitgroup data. Quitgroup data shows that, in January to March 2015, a total of 1050 people were referred, with 674 referred from “person to person” sources and 376 from “self-service”. Assuming the rate of use of this service is stable over the year, this equates to about 4,000 people from CM Health per year using Quitline services. Use is similar by gender, with higher rates of use for Maaori and European smokers, compared to Pacific (e.g. Jan to March 2015: 33% Maaori, 35% European and 17% Pacific). This indicates a relatively low use of the service by Maaori and particularly Pacific people, after accounting for the prevalences of smoking in these ethnic groups, and comparing to European. Use of Quitline is highest in middle age (25 to 64 years), with lower use in younger people aged 15 to 24 and older people, aged 65 years and over. 6 Milne R, Beasley R. Hospital admissions for chronic obstructive pulmonary disease in New Zealand NZMJ 30 January 2015, Vol 128 No 1408; ISSN 1175-8716 Page 8 of 35 Insights CM Health has also made attempts to gather qualitative insights from smoking cessation practitioners who work with our priority populations7. In order to gain deeper insights into our Maaori and Pacific smoking populations, we have commenced a market research and segmentation project that will be completed by June 2015. This work seeks to improve our understanding of people’s motivation and behaviours around smoking and quitting, so that we may design and implement more effective smokefree messages and services, and use the most appropriate channels to reach people. The key insights from Stage One8 of this process, which involved interviews with smoking cessation practitioners and a research review, are presented below. These will be explored with consumers in depth in Stage Two: Social Social and identity Social and cultural Social and environmental Smoking is a ‘social norm’ in the family Smoking is a fundamental part of a person’s identity (individual and family) Family is the hub, the heart and the nucleus. Family is everything (relates to a family’s influence on smoking and quitting, as well as to our messaging and service delivery) Life circumstances make it significantly harder to want to stop smoking and meet commitments Behavioural Smoking is used as a ‘release’ and stress management tool Belief and knowledge People don’t understand the true nature of addiction Lack of health literacy = not understanding the risks Lack of knowledge of treatment options available, and trust that they will work Less likely to actively seek interventions; self-referrals are not the norm Culture Importance of being ‘real’, tailoring delivery style to the individual’s culture is make or break. Psychology Successfully quitting involves readiness to quit – finding a key motivator, to unlock the personal ‘why’ 7 8 These themes are summarised in Reference Document 14 Smokefree Research Stage 1 Finding. Richards Partners. January 2015. Page 9 of 35 Current Services What is the current mix of services in Counties Manukau and h ow well are they reaching our priority populations? Current Services: Tobacco Control Leadership, Health Targets, Smoking Cessation Services and Health Promotion Services (Counties Manukau Health) CM Health is currently funded by the Ministry of Health under three revenue streams for a range of core tobacco control activity, as set out in Table Five below. This funding is currently in place until June 2016. The Ministry of Health’s decision to retender smoking cessation services nationally may impact the revenue received by CM Health for Maaori and Pacific smoking cessation services (second and third lines of the table below). CM Health also receives Ministry of Health Pathway to Smokefree 2025 funding for three innovation projects, as set out in Table Six. Page 10 of 35 Table Five: CM Health funding for Core Tobacco Control Activity Revenue Stream Tobacco Control $679,920 p.a. to June 2016 Required Activity Tobacco Control Leadership Develop, implement and review progress against a DHB tobacco control plan Provide leadership related to tobacco control in CMDHB area Health Targets, Smoking Cessation Services and Health Promotion Services Support the Government’s Health Targets Monitor, plan, coordinate and develop local smoking cessation activity Monitor and analyse referrals and service uptake for priority populations Support and/or lead local health promotion activities Participate in national service development work and adhere to national specifications and guidelines Page 11 of 35 Current Activity CM Health currently employs a core team of 6.25FTE (the Smokefree Service) who collectively provide tobacco control leadership, planning and strategy, analysis, support to achieve health targets, delivery of a specialist smoking cessation and triage service, health promotion, and national service development work. This team is comprised of: 1FTE Portfolio Manager 1FTE Team Manager 1FTE Secondary Care Advisor 1FTE Primary Care Advisor 0.75FTE Maternity Advisor 1FTE Referrals Coordinator 0.5FTE Inpatient Advisor CM Health also contributes baseline primary care funding through the Long Term Conditions Portfolio Manager role and PHO contracts which is focused on sustaining the primary care target and improving cessation support. The Target Advisor roles were realigned with MOH priorities in 2014 to work across the health system, and have a specific focus on improving cessation support within target activity. Delivery of a specialist cessation service is through the Referrals Coordinator who manages over 2,000 referrals per year through the CM Health triage hub which provides one-off and intensive support, and also connects to all local services (and Quitline). The Target Advisors each carry a small caseload of clients requiring specialist support. The service coordinates and delivers group-based treatment within the district. The Inpatient Advisor provides a dedicated specialist smoking cessation service to inpatients in Middlemore Hospital and satellite sites. Demand for this service continues to increase, with 347 referrals in 2013, 866 in 2014, and projected 1,120 in 2015. As of April 2015 the service will employ a 0.8-1FTE Mental Health Advisor to provide a wide range of smokefree support within CM Health mental health services. The core service coordinates the local roll out of national campaigns such as Stoptober and World Smokefree Day. It also supports key sector and innovation initiatives e.g. Breakfree, Its About Our Tamariki. It contributes to regional planning and networks including the ARPHS/DHB Forum. It leads the local Smokefree Provider Network, and a Clinical Supervision Network for local cessation practitioners. CM Health also provides responses to national and regional tobacco control issues that affect our smoking population. This funding also covers other initiatives such as: Manawhenua Smokefree Leadership. Local communications activity designed to increase access to cessation support. Market research activity. Regional Mental Health NGO Smokefree Project (NRA). Maaori Services $135,374 June 2016 Pacific Services $202,190 June 2016 Cessation p.a. to Cessation p.a. to Planning and funding of additional Maaori cessation service/s within CMDHB Planning and funding of additional Pacific cessation service/s within CMDHB The Mangopare Smokefree Service at Raukura Hauora O Tainui is funded until May 2015. A tender process is currently underway to identify providers of Maaori and Pacific cessation service(s) for a period of up to 18 months from mid-2015. Supporting people with mental illness and addictions is an explicit priority area for the new service(s). The Pasifika Smokefree Service at South Seas Healthcare Trust is funded until May 2015. A tender process is currently underway to identify providers of Maaori and Pacific cessation service(s) for a period of up to 18 months from mid-2015. Supporting people with mental illness and addictions is an explicit priority area for the new service(s). Table Six: CM Health Pathway to Smokefree 2025 Innovation Funding Revenue Stream Quit Bus (currently funded until June 2016) Required Activity Plan, deliver and evaluate the regional Quit Bus project, a mobile smokefree service delivered via two vans Current Activity As stated. One of two vans predominantly services the Counties Manukau area. Priority groups are Maaori, Pacific, pregnant women and their families, and rangatahi (youth). Smokefree Together 2025 (Intersectoral Project) (currently funded until January 2017) Plan, deliver and evaluate the regional intersectoral project which aims to provide a comprehensive smokefree support programme in Government agencies and workplaces outside the health sector Pregnancy Incentives Project (currently funded until October 2016) Plan, deliver and evaluate the Pregnancy Incentives Project in three localities in Counties Manukau. Page 12 of 35 As stated. Currently, the project focuses on agencies within Counties Manukau, however will be expanded across the Auckland region. Priority groups are Maaori and Pacific. As stated. The project has been rolled out in two localities, and is planned to roll out in a third locality in late 2015. Priority groups are Maaori and Pacific pregnant women and their families. Current Services: Enforcement Services and Health Promotion Services (Auckland Regional Public Health Service) Auckland Regional Public Health Service (ARPHS) delivers tobacco enforcement and health promotion services for the metropolitan Auckland region. A copy of the draft ARPHS Annual Operating Plan for 2015/16 is included below. Note that this plan is in draft, and yet to be finalised. ARPHS will develop a strategic smokefree action plan in 2015/16 as part of its health promotion functions that contributes to regional outcomes for reducing tobacco related harm and supporting Smokefree Aotearoa 2025. It is expected that CM Health will have considerable input into the development of this plan to ensure that it aligns with regional priorities. Page 13 of 35 Table Seven: ARPHS Annual Operating Plan 2015/16 (draft) a. Enforcement Smoke-Free Environments Act Performance Accountability Core Func. Health Prot Short Term Outcome 1. Tobacco retailers and licensed premises have increased knowledge about the Smoke-free Environments (SFE) Act Activities Key Performance Measures Pro-active Controlled Purchase Operations (CPO)[1] Quantity Estimate / Target per year Number of CPOs conducted.[2] Baseline 13/14: 9 Number of retailers visited during the CPOs. Baseline 13/14: 227 Quality Summary of rationale for targeting tobacco premises Outcome of operation is recorded as per audit protocol Short Term Outcome Measures Number and percentage of tobacco retailers visited during Controlled Purchase Operations (CPOs) in which tobacco is sold to minors Baseline 13/14: 3% Number of positive[3] sales during CPOs. Baseline 13/14: 6 Process complaints as per the Smokefree Enforcement Officer Protocol Preparation of files for the Ministry of Health when prosecution possible Participation in hearings as required b. Number of complaints processed investigating suspected breaches of the Smokefree Environment Act. Baseline 13/14: 60 Number of files requesting infringement notices for sale of tobacco to minors sent to MoH. Estimate: 7 Number of hearings where ARPHS staff presented evidence Percentage of complaints which have an action completed within 5 days Estimate: 100% Summary of quality of files received by MoH six monthly Number and percentage of complaints closed Number and percentage of files requesting infringement notices for sale of tobacco to minors sent to MoH Brief narrative of outcomes of hearings participated in Tobacco: Health Promotion Performance Accountability Core Func. [1] Short Term Outcome Activities Key Performance Measures Quantity Estimate / Target per year Quality Short Term Outcome Measures All proactive tobacco retailer compliance checks and controlled purchase operations conducted within 1 km of transport hubs, malls and other areas where young people congregate with a deprivation index score of 6-10. These areas have the highest rate of Māori, Pacific and low socioeconomic children who are more susceptible to initiating smoking at a younger age [2] One CPO equals one total organised operation that targets a number of premises. [3] COPs CPOs where tobacco is sold to minors Page 14 of 35 Health Prom Health Prom 1. Contribute to regional outcomes for reducing tobacco related harm supporting Smokefree Aotearoa 2025 2. Strengthen strategic alliances and interagency networks Develop an ARPHS Smokefree Strategic Action Plan Smokefree Strategic Action Plan developed. Yes/No On-going health promotion activities to promote Smokefree awareness and support national tobacco initiatives (e.g., Pacifica Festival, Stoptober) Number and type of health promotion activities supported[4] Implementation proceeding as per plan Brief narrative will be provided Brief narrative of outcomes from activities Stakeholders participate in World Smokefree day Lead regional stakeholder coordination of World Smokefree Day Health Prom 3. Increase adoption of policies which support the reduction of tobacco related harm Leading the facilitation of: Regional Cessation Network Smokefree coordinator meetings for Auckland and Northland Brief narrative of outcomes from activities Support Alternative Education settings to become Smokefree Undertake advocacy activities other than formal submissions Brief narrative of outcomes from activities Summary of outcomes of advocacy activities other than formal submissions Number and type of engagement/advocacy activities Input into submissions relevant to Smokefree environments In collaboration with the Work Place Health team, deliver Smokefree awards to exemplar workplaces [4] ARPHS uses an opportunistic approach to work collaboratively with other agencies Page 15 of 35 See H1.1 Healthy Public Policy for formal submissions See Work Place Health section See H1.1 Healthy Public Policy for submissions ReducInq inequalities 4. Support high need populations to be Smokefree Continue to work with selected New Zealand Federated Family Budgeting Services branches and other social providers Continue to deliver ARPHS internal Quitcard Provider Project Māori Health Gain Page 16 of 35 Active engagement with Mana Whenua and Māori communities to develop Smokefree policies in prioritised settings Number of branches participating in project Number of trainings delivered Narrative on engagement with Mana Whenua and Māori Smokefree providers Summary of actions implemented by branches Ensure that only Ministry accredited trainers are used to provide the training. Yes/No Number (percentage) of staff trained 2015-18 focus ARPHS’ role centres around support and leadership for regional and national advocacy, and environmental and system change initiatives across supply, demand reduction and reducing opportunities to consume tobacco. ARPHS has proposed that priority areas will include initiatives or policies that support smokefree cars and homes, revitalising activities to support smokefree workforces, making tobacco less available, and protecting children from exposure to smoke. Activities that are currently anticipated (but yet to be confirmed) include: Strengthen Early Children Education (ECE) activities to support smokefree cars, homes and ECE workforce. Build off revitalised workplace health promotion strategy to encourage prioritised workplaces to work towards a smokefree workforce. Strengthen health promotion leverage achieved from Smokefree compliance activities to ensure tobacco is less available to young people, and to support or encourage the prevalence of smokefree outdoor dining in Tamaki Makaurau. Continue to work with Council and Council owned enterprises (i.e. ATEED) to support public venues, events and workforces are smokefree. Build on work with prioritised non public (i.e. not Council) venue owners and event organisers (including sports clubs as appropriate) to develop policies and approaches that support smokefree events and membership. Work with other national and regional providers to expand and develop a regional indicators for smokefree health promotion i.e. density of retailers with distribution by NZDep, proximity to schools and sites of significance, proportion of regional outdoor areas/spaces that are smokefree. Explore and trial the feasibility and impact of community action and development initiatives on the development of smokefree retailers, streets and neighbourhoods. Key themes and gaps in relation to current smoking cessation activity Ministry of Health Review of Tobacco Control Services Inequitable funding for the Counties Manukau smoking population A major gap for the Counties Manukau smoking population was identified in the Ministry of Health commissioned Review of Tobacco Control Services (2014). As the District Health Board with the largest number of people living in high deprivation, the largest Pacific population, and a large Maaori population, we have strong concerns that the total resource per smoker is the second lowest of all DHBs (Review, p 189). This issue becomes even more apparent when the calculations of the smoking population are made using estimated resident data (in accordance with Statistics NZ guidance), not usually resident data as included in the review. There is a major opportunity to provide equitable funding to Counties Manukau Health in accordance with a formula that takes into account the size and composition of the smoking population. CM Health has demonstrated strong leadership in developing new service models that are effective in engaging our Maaori and Pacific communities and supporting them to stop smoking, and the number of people accessing local smoking cessation support in the district has steadily increased in the last three years. There is strong and continued demand for smoking cessation support delivered by local services, and with additional capacity we could cater to a significantly greater number of people. How we would invest additional resource Should additional resource become available, our priorities are to increase access to smoking cessation support for our priority populations, diversify the type of support options on offer, and increase capacity to cater to a greater number of people. Areas that we would like to develop or expand upon are as follows: Develop new or enhance existing models of smoking cessation support (for example new models such as pharmacy based support, elective surgery pathway; existing models such as Quit Bus, Pregnancy Incentives) Expand the Inpatient Specialist Smoking Cessation service for which demand continues to increase due to the focus on the ‘C’ of ABC in secondary settings. The service is provided to inpatients in Middlemore Hospital and satellite sites. It has seen a significant increase in the past 2-3 years: 347 referrals in 2013, 866 in 2014, and a projected 1,120 in 2015. Page 17 of 35 Develop and grow the smoking cessation workforce to include casual/’bank’ practitioners who are prepared to work flexible hours, provide flexible group-based treatment options, support periods of increased demand e.g. during major campaigns, and grow a youth/community ‘army’ of people able to provide smokefree support and champion smokefree issues in their communities. Implementation of quarterly innovation initiatives aimed at encouraging access to and uptake of smoking cessation support amongst priority populations. Design and implementation of a communications and engagement strategy tailored to Counties Manukau communities, including implementation of market research recommendations. Development and implementation of a youth specific plan. CM Health Review In addition, CM Health completed a review9 in February 2015 that summarised the key themes and gaps in relation to current smoking cessation activity for the priority populations identified in this plan: Maaori Pacific peoples Younger age groups (20-34 year olds in particular, and 15-49 year olds overall) People with mental illness and addictions Pregnant women and their families/whaanau People with chronic health conditions Localities: Manurewa, Papakura and Mangere/Otara/Papatoetoe A high-level summary of these themes and gaps is provided below. Overall, services achieve a reasonable to high reach with Maaori Overall, Maaori-specific services have a high reach with Maaori clients (at least 70% of their clients identify as Maaori). Other services that are not solely focused on this priority group, still maintain a reasonable reach (at least one-third, and up to one half of all clients are Maaori). Quitline is the only exception to this, with one-fifth of clients from CMDHB being Maaori. Currently, almost half (48%) of the total referrals10 for support in Counties Manukau are for Maaori. Based on current service data we estimate 11-15% of Maaori in our district who smoke are accessing cessation support per annum. Overall, service reach for Pacific needs to improve The Pacific service has a high reach with Pacific clients (average 80% of their clients identify as Pacific). For all other services, Pacific consistently have lower access than Maaori (overall, an estimated 5-6% of Pacific who smoke accessed cessation support, compared to 11% for Maaori). Currently, almost one-third (29%) of the total referrals for support in Counties Manukau are for Pacific10. There is a need to focus efforts on increasing access to support for Pacific people, bearing in mind that there are approximately the same total number of Maaori and Pacific people who smoke, and that Maaori and Pacific are as likely as other groups to try to quit 11. Local services have better reach for Maaori and Pacific Historically local services have had considerably better reach for Maaori and Pacific than Quitline. We need to ensure that this is well communicated and reflected in referrals patterns, so that people have access to the best support to quit for their needs. Mixed reach amongst men and women Overall, services have mixed reach with men and women. This is an area we need to improve our monitoring of in future. Mental health and addictions, and chronic physical conditions People with mental illness and/or addictions other than smoking comprise a significant proportion of our total smoking population. This is not an additional group to other priority groups, but a priority group within the wider population 9 See Reference Document 12. Q2 2014/15 referrals data, total referrals in CMDHB district (all services). This data is being collated and monitored as of Q2. Excludes Quitline (if included, figures are: Maaori – 34% Pacific – 20%). 11 New Zealand Health Survey data, cited in The Population Who Smoke in Counties Manukau, May 2014 10 Page 18 of 35 who smoke. There has been an absence of dedicated support for this priority group until very recently and relatively poor data available for monitoring service provision for this group. There is limited information about the number of people who have a chronic physical condition (e.g. gout, diabetes, cardiovascular disease, chronic obstructive pulmonary disease and coronary heart failure) who smoke, however it may be reasonable to assume that a higher proportion of this cohort smoke or are a recent ex-smoker than the overall population, due to the presence of what may be a smoking-related condition. CM Health is well placed to engage with this group through both secondary and primary care target activity, and other health system initiatives. There is likely to be significant overlap between these two priority groups. CM Health analysis indicates that people who had received care for mental health unwellness had a higher prevalence of long-term conditions, and 12-18% of people with long term conditions are likely to have a severe mental health condition and/or addiction. Going forward, as well as improving mental health and addictions activity in particular, we also need to develop systems to monitor outcomes for both groups. Pregnant women and their families/whaanau The Pregnancy Incentives Service has demonstrated a highly effective approach to supporting pregnant women to stop smoking during pregnancy. Pregnancy cessation services have a strong focus on Maaori and Pacific women. Estimates indicate there are approximately 1,700 pregnant women who smoke in CM Health per year, and based on this, approximately one-third of these women are currently referred to a specialist service for support. This is likely to increase with the incentives service being rolled out in two additional localities in 2014 and 2015. Priority localities Whilst the innovation initiatives (particularly Quit Bus and Pregnancy Incentives Pilot) clearly prioritise these localities, locality data is not currently reported for other services. We need to build this into reporting requirements and data collection systems for cessation services going forward. The three localities have been identified as specific priority areas for the Maaori and Pacific services currently under tender. We need to design and deliver services with younger age groups in mind Community-based services appear to be reaching younger age groups overall. Smoking prevalence data is clear that our priority age group is 20-34 year olds, and 15-49 year olds more broadly. It is crucial that services and activity are designed with younger age groups in mind, and overall this will require a shift from the current way of doing things. We need smart strategies that cater to the needs of multiple groups Many of the identified priority groups overlap, and hence there is considerable potential to reach people who belong to more than one of these groups (e.g. young pregnant Maaori women living in Papakura, or Pacific people living in Mangere who have a chronic physical condition and mental illness, as well as their families). This also means we need smart strategies that cater to multiple groups at once. Increase use of NRT and cessation medications There is a significant opportunity to increase familiarity and use of stop smoking medications for approximately 80% of the smoking population. This is a very important area of action for primary and secondary care health target activities, where the emphasis needs to be strongly on the ‘C’ of ABC. Our analysis of NRT data indicates that once people have tried NRT once, they are more likely to try it again. Understanding barriers to initial use of NRT and supporting people to overcome those barriers are key activities. Further work is needed to fine-tune existing activity and set appropriate targets We need to sustain our efforts where we are already doing well, and understand why particular strategies work well, as well as focusing our efforts in those areas that we could improve upon. This applies both at a whole-programme level, as well as within individual activities and services. We need to work with the population health team to identify appropriate overall targets for access to cessation support for Maaori and Pacific (relative to prevalence). Page 19 of 35 The review process needs to be repeated annually in order to effectively assess progress with the identified priority groups. To enable this, we need to identify a set of key indicators 12 to be monitored each year, and set up the systems to support this. Coordinated regional approach to achieving Smokefree 2025 A further gap that has been identified, but that relates to Smokefree activity more broadly, is the need to take a more coordinated approach between key stakeholders towards achieving Smokefree 2025. This means working in a more coordinated manner with other DHBs (particularly Auckland and Waitemata), with the Auckland Regional Public Health Service, and with Ministry of Health in relating to planning and funding decisions. A strategic approach towards achieving Smokefree 2025 for the Auckland region would provide focus, direction and efficiencies in achieving our shared vision. Cost per Successful Quit It is not feasible to include an analysis of the cost per quitter for existing smoking cessation services in Counties Manukau due to data limitations. It is important to note that a cost per successful quit analysis was undertaken for the Counties Manukau Health Pregnancy Incentives Pilot 13, which demonstrated the pilot to be much more cost-effective than the other five pregnancy services nationally and equal to that of the best performing service. Table Eight: Comparison of cost per quitter between different services Approximate cost of per quitter 4 weeks after Quit Date CO validated* Self-report* National Provider 1 $7,000 $5,000 National Provider 2 $2,000 $1000 National Provider 3 $27,500 $5,000 National Provider 4 $22,500 $8,500 National Provider 5 $3,500 $2,000 National Provider 6 $8,500 $7,000 Previous Smokefree pregnancy service Unavailable $4,000 Previous DHB Smokefree pregnancy service Unavailable $3,500 $2,000 $2,000 Pilot * Figures rounded to nearest $500 Summary of achievements Years 1-2 The Ministry of Health Tobacco Control Planning and Funding Leadership process is aimed at taking a more collaborative and coordinated approach with DHBs in order to achieve the Smokefree 2025 goal. Counties Manukau Health commenced its Smokefree Counties Manukau 2025 Initiative prior to this process being initiated, and therefore has already undertaken significant needs analysis processes to inform planning to achieve Smokefree 2025, and as at June 2015 will have already delivered the first two years of its five-year Smokefree 2025 plan. The following is a summary of some of the significant achievements that have occurred to date, and which CM Health will continue to build on during Years 3-5: 12 13 This includes appropriate indicators for the CMDHB Triage service as one part of a ‘wider system’ (e.g. declines and UTC’s). Smokefree Pregnancy Incentives Project: Final Evaluation Report. Resonance Research. January 2015. Page 20 of 35 Organisational commitment to Smokefree as a major population health priority In 2012 the CM Health Executive Leadership Team and Board endorsed Smokefree as a key population health priority area for the next five years, and endorsed the strategic approach to achieve a Smokefree Counties Manukau by 2025 (defined as 5% smoking prevalence or less across all groups). There is strong support for Smokefree activity at the Executive Leadership level and across many areas of the organisation which ensures that it retains a high profile. CM Health is committed to preparing responses on behalf of the organisation to tobacco control issues that have an impact on our whole population, such as Plain Packaging, the Auckland Council Smokefree Policy, and implementation of the policy by Local Boards. Extensive needs analysis and market research Counties Manukau Health has undertaken an extensive needs analysis process which has included in-depth analysis of demographic data about our smoking population, attempting to quantify the number of people required to quit in order to achieve the Smokefree 2025 goal, ongoing community consultation, and reviews of current service provision. This process continually informs our planning at both project and whole of programme level. Most recently, we have contracted an agency that specialises in market research and design thinking to gain deeper insights into the Maaori and Pacific smoking population with a view to informing communications messages and channels, and service planning and delivery. This work will be completed by June 2015. Realignment of CM Health resource across the health system and community In late 2013, Ministry of Health advised the requirement for District Health Boards to shift Smokefree resource from secondary care to a broader focus across the health system, particularly primary care, and the wider community. In response to this, and to meet the needs of its Smokefree 2025 Initiative, CM Health implemented a new programme structure which was effective as of late 2014. The new structure provides targeted support across primary, secondary and maternity care, as well as within the community. This is supported by the range of community-based innovation initiatives led by CM Health, and its community-based smoking cessation contracts. Consistent achievement of primary and secondary targets The secondary care target has consistently been achieved since Quarter 4 2011/12, and the primary care target since Quarter 4 2013/14. This means that a large proportion of the currently smoking population are receiving brief advice and support to stop smoking through the health system. The maternity target has also been achieved since Quarter 1 2014/15; however the data source for this target is not representative of our total pregnant population because a substantially higher proportion of CM Health women are provided with AN care by DHB employed midwives than in other DHBs and the data source only captures information from self-employed midwives. Hence the maternity target results for our DHB need to be interpreted with caution. Improving access to cessation support through the health system Since the inception of the secondary care health target, CM Health has had a strong focus on the ‘C of ABC’; ensuring that people not only receive brief advice, but are connected with support to quit smoking. A major ‘improving the C’ campaign was implemented in secondary care in 2013/14, which resulted in an almost doubling of referrals (an increase of 1,000 from 1,145 in 2012/13 to 2,142 in 2013/14), and with high reach to Maaori (42% of referrals), Pacific (25%) and pregnant women (15%). This number has been sustained in 2014/15. This focus is also being translated to primary care as of early 2015, with CM Health providing dedicated support to PHO’s to improve the proportion of patients who smoke that receive appropriate cessation support. It is also the primary focus of the Maternity Health Target Action Plan, with specific referrals targets having been set for pregnant Maaori and Pacific women. A ‘one stop shop’ for support to stop smoking: connected cessation services Smoking cessation services in Counties Manukau are well connected to each other, with a good degree of cooperation and communication between services. This is supported by a well-established Provider Network that meets monthly and is open to all stop smoking services and other services involved in smokefree activity in the district. CM Health also provides a Clinical Supervision Network that is open to all stop smoking practitioners in the district. Key to this approach is a centralised triage service, which has been in place at the Counties Manukau Health Smokefree Service since March 2013. The service is increasingly promoted as a ‘one stop shop’ for anyone who wants support to stop smoking. It provides a first phone assessment for all referrals, and connects to all known cessation services in the Page 21 of 35 district as well as Quitline. It is staffed by a dedicated Referrals Coordinator and currently handles in excess of 2,200 client referrals per year, with the majority of referrals from secondary care and other health professionals such as midwives. With the increased focus on cessation support in primary care, referrals are expected to increase from this setting in future, as well as from other sources such as community and self-referrals. Improving the reach, volumes and performance of community-based stop smoking services CM Health’s needs analysis process has clearly indicated that stop smoking services need to support significantly more people to stop smoking than current service targets allow for. To achieve the intermediate goal by 2018, an extra 4,200 people will need to stop smoking and stay smokefree each year, on top of the current state. CM Health is therefore undergoing a tender process to purchase new Maaori and Pacific stop smoking services that demonstrate innovative approaches to supporting greater numbers of people who smoke to quit. The process is due to be completed in mid2015, with service implementation commencing in Year 3 (2015/16). Support for people with mental illness and other addictions Identifying a considerable gap in activity to support people with mental illness and other addictions who smoke, and responding by: Co-funding the Northern Regional Alliance Mental Health NGO Smokefree Project with Auckland and Waitemata DHBs Undertaking a needs analysis with our DHB mental health services and funding a dedicated Mental Health Smokefree Advisor and key initiatives as a result Identifying people with mental illness and other addictions who smoke as an explicit priority group for the Maaori and Pacific community smoking cessation services being tendered in early 2015. Trialling innovative approaches for Maaori and Pacific CM Health has led the development and implementation of three major innovation projects aimed at denormalising smoking and increasing quitting amongst Maaori and Pacific communities. The Pregnancy Incentives Pilot has demonstrated a highly effective approach to recruiting, engaging and supporting pregnant Maaori and Pacific women to quit smoking. Women enrolled in the pilot were almost three times more likely to stop smoking at 4 and 12 weeks post quit date compared to previous services 13. The Quit Bus has reached significant numbers of people who smoke from priority populations, particularly Maaori, and younger age groups. In its first 15 months, the Counties Manukau Quit Bus engaged 343 people for one-off support to quit, an additional 739 for intensive support, and had a brief conversation with 3,845 people (total reach 4,927). The Smokefree Together 2025 (intersectoral) project has engaged with a wide range of non-health sector settings to equip them to address smoking amongst staff, clients and within their settings. Agencies include Community Probation Services (7), Work and Income (9), Alternative Education (1), other social services (5), tertiary providers (2), and workplaces (7). CM Health led an enhanced version of the national Stoptober campaign that was specifically tailored for our local communities. Campaign activity, informed by engagement with the community, was widespread across the district and gained a lot of momentum and visibility. The evaluation showed mixed findings about the number of people accessing support to stop smoking as a result; however there have been a number of learnings that will inform future campaigns. Page 22 of 35 Year 3-5 Plan Logic model: Smokefree Counties Manukau 2025 Initiative (Years 3-5) CM Health strategic objectives to be confirmed SMOKEFREE COUNTIES MANUKAU 2025 5% smoking prevalence or less across all groups CM Health Strategic Objectives (TBC) Smokefree Aotearoa 2025 Whaanau Ora National Health Targets 2018 INTERMEDIATE GOAL 12% smoking prevalence overall Halving of 2013 smoking prevalence for Maaori (to 18%) and Pacific (to 12%) MOH Tobacco Control Review Fanau Ola INCREASE SUCCESSFUL QUITTING People who smoke are motivated and enabled to quit and stay smokefree. REDUCE INITIATION No-one, especially children and young people, starts smoking. WORKSTREAM ONE: CORE BUSINESS WORKSTREAM TWO: INNOVATIONS WORKSTREAM THREE: PIONEERING NEW FRONTIERS Improve the focus on cessation (the C of ABC) within the health system Trial and evaluate innovation initiatives (small and large scale) Expand the reach of smoking cessation support in other settings Adapt or adopt successful models into core business Identify new approaches that contribute to a reduction in smoking prevalence amongst priority groups Ensure core activity is targeted to priority groups, and that these groups receive consistent messaging and access to support Continually monitor initiatives to ensure reach to priority groups, adapting where required Demonstrate Smokefree leadership within and across the organisation Champion innovation initiatives led by others, ensuring a focus on CMH priority groups Increase engagement and uptake of smoking cessation support amongst priority groups, by improving our communications channels and messages Improve the reach and quality of DHB funded and delivered stop smoking services with a focus on testing new and innovative models Actively support key initiatives delivered by others in our district WORKSTREAM FOUR: EVALUATION AND MONITORING Effectively monitor the impact of both the wider Smokefree programme and individual projects (with a focus on increased successful quitting) Evaluate and monitor innovation trials to determine impact and add to the knowledge base for what works Share learnings within the programme and across the sector to inform future activity Page 23 of 35 Guiding Principles The following principles continue to underpin the CM Health Smokefree 2025 Initiative: A strong equity focus: CM Health will prioritise reducing smoking prevalence for Maaori and Pacific communities A dual focus on strengthening our core activity, whilst testing and trialling innovative approaches Increase consumer involvement at a programme and individual project level Collaborate with key stakeholders to inform service planning and implementation (including health and non-health stakeholders, regional stakeholders, and CM Health communities) Demonstrate organisational leadership towards Smokefree Aotearoa 2025 Thinking differently – beyond a ‘business as usual’ approach Continual evaluation and monitoring to inform programme development Page 24 of 35 HIGH-LEVEL ACTIONS 2015-18 Budget CM Health core tobacco control revenue currently runs until June 2016. Based on this, the plan includes detailed actions for Year 3 (July 2015 to June 2016), and proposed high-level actions for Years 4-5. The latter are subject to confirmation of revenue. Workstream One: Core Business The focus of this workstream is to: - - Improve the focus on cessation (the ‘C’ of ABC) within the health system (including DHB funded and contracted services) Expand the reach of smoking cessation support in other settings Ensure core activity is targeted to priority groups, and that these groups receive consistent messaging and access to support Demonstrate Smokefree leadership within and across the organisation Improve the reach and quality of DHB funded and delivered smoking cessation services with a focus on testing new and innovative models Actively support key initiatives delivered by others in our district. To achieve this we will focus on the following key areas: Note: secondary, primary and maternity target actions are yet to be finalised within the CM Health Annual Plan. Secondary Care Continue to employ a dedicated Secondary Care Advisor to support sustained achievement of the secondary care target and a continual improvement in the proportion of patients receiving smoking cessation support. Overall target 95 percent of patients who smoke and are seen by a health practitioner in public hospitals will be offered brief advice and support to quit smoking. Local target A minimum of one-third of inpatient, and one-third of other hospital services referrals will be for Maaori, and one-third for Pacific. Page 25 of 35 Year 3 actions: - Providing, and/or resourcing Nurse Educators, Smokefree Champions and other clinical staff to provide ongoing best practice training, orientation training and refreshers Formalising the Smokefree Champions programme, and ensuring there is an identified Champion in all secondary care services Supporting and resourcing Smokefree Champions to promote commitment to Smokefree Best Practice Ensuring there is an identified Smokefree lead in all secondary care services Audit and feedback processes including monthly target and referrals reporting and coordination about missed interventions Acknowledgement of top referrer of the month across secondary care services Continuing to provider the three Annual Awards acknowledging Smokefree Best Practice Continuing to roll out support for Manukau Super Clinic modules and other satellite sites to implement Smokefree Best Practice Trialling an ‘opt-out’ referrals system for all patients who smoke in at least one additional hospital ward Identify additional DHB Provider services for roll out of Smokefree Best Practice 2015/16 Baseline: Inpatient referrals: estimated 700 (230 Maaori, 230 Pacific) Other hospital services referrals: estimated 1,000 referrals (330 Maaori, 330 Pacific) Primary Care Support PHO’s to sustain achievement of the target, and continue to employ a dedicated Primary Care Advisor to support a continual improvement in the proportion of patients receiving smoking cessation support. Overall target 90 percent of PHO enrolled patients who smoke have been offered help to quit smoking within the past 15 months. - Implement the Stop Smoking project for people with Long Term Conditions within the organisation’s Manaaki Hauora – Supporting Wellness campaign. Determine feasibility of establishing a smokefree support pathway for elective surgery patients Trial new initiatives in secondary services aimed at increasing access to smokefree support for patients and whaanau, visitors and staff Provide a quarterly e-newsletter that includes key messages and updates across the three target areas and mental health and addictions Long-term actions (Y3-5): - All DHB Provider services to consistently deliver Smokefree Best Practice Year 3 actions: Focused on sustaining target performance: - Meet with PHO partners monthly to support the PHOs to achieve target by assessing performance and sharing best practice ideas and issues with other PHOs and the Clinical Champions for IPIF - Continue the smoking cessation e-module training - Ensure that patient dashboards and prompts are used when patients attend practice visits - Produce reports and undertake audits that enable practices to help them track progress against MOH targets - Produce weekly graphs showing performance against the target to all practices - Provide support to practices with regular staff visits to discuss progress to date and share best practice with other practices - Ensure practices have champions for smoking cessation who will provide ongoing coaching and support to patients and staff - Support practices to call appropriate patients to offer referrals to cessation support services - Utilise existing resources e.g. VLCA nurses, He Puna Oranga nurses to assist practice to achieve targets - Work with Care Coordinators for ARI patients to assist and support them to provide cessation support and referrals to cessation services - Ensure that appropriate self-management support for smoking cessation is in place within all CM Health localities Focused on improving the rate of cessation support: - IPIF Clinical Champions to support CM Health and PHO’s with guidance and advice to increase the rate of smoking cessation - Dedicated Smokefree Advisor (Primary Care) is employed by CM Health to support PHO’s to improve the rate of cessation support, with a focus on Maaori and Pacific. Activities include: - Analyse PHO/practice performance in relation to cessation support and provide tailored support to prioritised practices - Work with CM Health and PHO’s to build referral relationships with local smoking cessation services - Coordinate and/or deliver Smokefree Best Practice training and other relevant education opportunities Page 26 of 35 - Maternity Achieve and sustain the maternity target, with a focus on improving access to cessation support in pregnancy, particularly for Maaori women. Long-term actions (Y3-5): - Develop a regional training strategy for allied health (starting with Dentists and Radiographers) Year 3 actions: - Overall targets 90 percent of pregnant women who identify as smokers upon registration with a DHB employed midwife or Lead Maternity Carer are offered brief advice and support to quit smoking. Percentage of pregnant Maaori wahine who are smokefree at 2 weeks postnatal. Local target 50 percent of pregnant women who smoke are referred to cessation services (and 60 percent of Maaori women). - - Page 27 of 35 Undertake a stocktake of current activity in relation to patients ‘given or referred to cessation support’ (indicator four) to understand current performance and identify areas for improvement Coordination of agreed pilot projects to increase access to cessation support Improve primary care follow-up and coordination for patients receiving smokefree support in hospital Ensure primary care records reflect patient access to smoking cessation support by linking with external Smokefree initiatives and services Support Smokefree initiatives in general practice such as Stoptober, World Smokefree Day and Quit Bus Coordinate with other screening activity to deliver smokefree messages (e.g. CVD risk assessments, cervical screening) Investigate the development of a pilot project aimed at increasing reach to smoking cessation support via Pharmacies in priority localities Governance Group continues to guide implementation and monitoring of Maternity Target Action Plan Implement Maternity Target Action Plan. Activities to include: Continue to promote proactive referrals by Midwives to specialist Smokefree services Review strategies and resources implemented in 2014/15 that increased referrals and continue those that were effective Promote the importance of reducing smoking prevalence in pregnancy, particularly for Maaori, via newsletters, monthly meetings with self-employed midwives and internal communications Support training opportunities for Midwives and monitor training uptake (Te Hapu Ora and e-learning tool) Showcase successful quitting stories with a focus on Maaori and Pacific Support a smokefree focus within key maternity initiatives including the SUDI Action Plan and the Maternity Services campaign Implement Year 3 of the Pregnancy Incentives Project, which includes: Continuing to deliver the project in the Manurewa and Mangere/Otara localities Rolling-out the pilot in a third locality planned for Papakura Scoping the addition of incentives after delivery to support postnatal smoking abstinence Trial and evaluate a QuickMist promotion to increase self-referrals to specialist services Collaborate with providers and community settings with high reach to pregnant women to increase delivery of Smokefree messages and referrals to specialist services Take a targeted approach to addressing low referral rates within existing DHB and community services Investigate incentivising referrers for referrals of pregnant women who smoke Work with Smokefree Advisor (Primary Care) and PHOs to trial an opt-out referral system in general practice for pregnant women in priority localities - Work collaboratively with Well Child Tamariki Ora and other providers to deliver smokefree interventions with whaanau Implement recommendations of market research activity completed in mid-2015 in relation to pregnant women and whaanau Additional actions to support postnatal Maaori wahine to be smokefree: - Address inconsistencies in referrals rates and promote proactive referring by midwives - Explore Maaori specific training to upskill midwives in delivering smoking cessation messages with Maaori clients - Introduce referral intervention at time of delivery for all women who smoke - Collaborate with Maaori providers to deliver smokefree messages and increase referrals to specialist services - Ensure specialist smoking cessation services actively promote to Maaori communities and generate selfreferrals - Showcase whaanau quitting stories - Work collaboratively with Well Child Tamariki Ora providers to support postnatal and whaanau smoking abstinence Mental Health and Addictions Support mental health and addictions services to consistently address Smokefree so that service users receive consistent smokefree messaging and consistent Smokefree care. This activity aligns to the Review of Tobacco Control Services recommendation to increase focus on smoking cessation for people with mental health issues Year 3 actions: - With Auckland and Waitemata DHBs, continue to fund and support the Northern Region Mental Health NGO Smokefree Project - Continue to fund the dedicated local smokefree mental health resource with a focus on DHB mental health and addictions services. Key activities to include: Work with services to establish a consistent approach to Smokefree brief interventions Provide Smokefree best practice and refresher training for staff, champions, and peer support specialists Coordinate Smokefree activity across inpatient, community and NGO services Improve access to local stop smoking services for service users, whaanau and staff Develop resources to assist in the implementation of Smokefree activity Implement key initiatives aimed at promoting quitting amongst service users/staff - Monitor performance of the new community stop smoking services, of which people with mental illness and/or addictions are an identified priority group - Facilitate access to appropriate mental health and addictions and smoking cessation training for smoking cessation practitioners in the CM district - Champion the ‘Breakfree’ innovation project which provides access to smoking cessation support for people with mental illness and addictions - Investigate the development of a regional plan to reduce smoking prevalence amongst this priority group. Long-term actions (Y3-5): - Investigate a specific project addressing smoking rates amongst youth within this priority group. Page 28 of 35 Funding and Delivering Smoking Cessation Services Year 3 actions: - Smokefree Leadership Implement and monitor the new Maaori and Pacific intensive stop smoking service(s) following a two-stage tender process in early 2015, with a focus on improved reach, quality and effectiveness. Continue to deliver the DHB Triage and Specialist Smoking Cessation Service with a continued focus on improving the number of referrals Trial new promotional strategies to increase self-referrals to the DHB Triage Service Lead and coordinate the district-wide clinical supervision network for intensive stop smoking practitioners Develop a plan to implement the recommendations of the 2015 smoking cessation needs and gap analysis Long-term actions (Y3-5): - Continued implementation and monitoring of the community-based smoking cessation services. - Increase the delivery of group-based treatment in coordination with local providers and identify new strategies to increase recruitment. Year 3 actions: - - Lead and coordinate the district-wide Smokefree Provider network Support the implementation of Auckland Council’s Smokefree Policy (aligns to the local cross-sector initiatives recommendation of the Review of Tobacco Control Services) Continue to participate on the Cancer Society’s ‘Its About Our Tamariki’ steering group and champion the initiative within CM Health networks (aligns to the local cross-sector initiatives recommendation of the Review of Tobacco Control Services) Incorporate smokefree requirements within the service specification for Maaori Health Integrated Service Agreements Develop an enhanced Smokefree clause for inclusion in all DHB contracts Support a strong Smokefree focus within key organisational initiatives Continue to identify and trial new initiatives aimed at enabling more CM Health staff and their families to become smokefree Provide a quarterly e-newsletter to registered local Quit Card providers Support the local implementation of national campaigns including World Smokefree Day and Stoptober Long-term actions (Y3-5): - Support a Smokefree focus within Te Rapunga Paeora (Maaori health) and Pacific health DHB services - Work with HR, Recruitment and Occupational Health to develop a project aimed at supporting a smokefree workforce. Investigate feasibility of regional initiative. - Enhance the role of local Quit Card providers - Support the smokefree component of the Healthy Families initiative - Improve coordination with existing DHB programmes and services to extend the reach of smokefree support Page 29 of 35 Young people Long-term actions (Y3-5): - Develop a plan that specifically addresses smoking amongst younger age groups - Collaborate with Maaori and Pacific workforce development initiatives to grow young Smokefree champions and identify smoking cessation training opportunities Workstream Two: Innovations The focus of this workstream is to: - Trial and evaluate innovation initiatives (small and large scale) Adapt or adopt successful models into core business Continually monitor initiatives to ensure reach to priority groups, adapting where required Champion innovation initiatives led by others, ensuring a focus on CM Health priority groups. To achieve this we will focus on the following key areas: Quit Bus Deliver the final year of the Quit Bus innovation pilot and identify ongoing funding to continue the service beyond June 2016. Year 3 actions: - Identify sustainable funding - Implement Year 3 of the Quit Bus innovation project, including: Undertake an evaluation of the initiative Improve access to Quit Bus support for Pacific people who smoke Collaborate with Maaori and Pacific workforce development initiatives to provide development opportunities and increase service capacity Design and deliver initiatives aimed at developing Community Champions Long-term actions Y3-5: - Identify sustainable funding to continue the service beyond June 2016. Pregnancy Incentives Project Roll out and evaluate the project in the third locality of Papakura and identify options for ongoing funding beyond June 2016. Year 3 actions See ‘Pregnancy Incentives Project’ actions within Workstream One (Maternity). Smokefree Together 2025 (Intersectoral Project) Deliver the second year of the project and commence project evaluation. Year 3 actions - Implement Year 2 of the initiative, enabling non-health agencies and workplaces to address Smokefree, with a focus on the following settings: Page 30 of 35 prioritised settings TBC number of agencies TBC cessation KPIs 28 single sessions /7 intensives/week This initiative aligns to the Government Cross-Sector activity, Local Cross-Sector initiatives, and non-health sector brief advice recommendations of the Review of Tobacco Control Services. Long-term actions Y3-5: - Implement project until January 2017 and evaluate impact to determine future requirements. In addition, CM Health will continue to champion and support other innovation initiatives such as Stoptober, Breakfree and Its About Our Tamariki. Workstream Three: Pioneering New Frontiers The focus of this workstream is to: - Identify new approaches that contribute to a reduction in smoking prevalence amongst priority groups Increase engagement and uptake of smoking cessation support amongst priority groups, by improving our communications channels and messages. To achieve this we will focus on the following key areas: Innovation trials Long-term actions Y3-5: - Identify and implement new innovation initiatives based on market research findings and 2015 needs/gap analysis. - Where resource permits, trial and evaluate one small scale initiative per quarter, with a view to adopting effective initiatives into core activity. Communications and engagement Long-term actions Y3-5: - Develop and implement a communications and engagement strategy, based on needs analysis and market research findings. Page 31 of 35 Workstream Four: Evaluation and Monitoring The focus of this workstream is to: - Effectively monitor the impact of both the wider Smokefree programme and individual projects (with a focus on increased successful quitting) Evaluate and monitor innovation trials to determine impact and add to the knowledge base for what works Share learnings within the programme and across the sector to inform future activity. We will focus on the following key areas in Year 3: Evaluation and Monitoring Year 3 actions: - Page 32 of 35 Determine a set of key indicators to monitor access to smoking cessation support across the district, as per the 2015 needs and gap analysis. Establish relevant systems to enable capture of this data. Use a simple framework to evaluate the impact of new innovation trials. Reference Documents 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Modelling for smokefree service planning. Doone Winnard, CM Health. October 2012. CMDHB Smokefree 2025 project brief. CM Health. February 2013. Thornley S. Characteristics of people using pharmaceutical aids to quit smoking in Counties Manukau Health, 2015. Unpublished manuscript. Ministry of Health. 2013. Health Loss in New Zealand: A report from the New Zealand Burden of Diseases, Injuries and Risk Factors Study, 2006–2016. Wellington: Ministry of Health. Webpage: http://www.hqsc.govt.nz/assets/Health-Quality-Evaluation/Atlas/CVD_standard/atlas.html; accessed 19/5/2015. Milne R, Beasley R. Hospital admissions for chronic obstructive pulmonary disease in New Zealand NZMJ 30 January 2015, Vol 128 No 1408; ISSN 1175-8716 Planning to inform cessation upscaling for 2014/15. Doone Winnard, Vicki Evans; CM Health. September 2013. Smokefree Research Stage 1 Finding. Richards Partners. January 2015. The population who smoke in Counties Manukau: A draft paper for discussion. Doone Winnard, CM Health. May 2014. Q2 2014/15 referrals data, total referrals in CMDHB district (all services). This data is being collated and monitored as of Q2. Excludes Quitline (if included, figures are: Maaori – 34% Pacific – 20%). New Zealand Health Survey data, cited in The Population Who Smoke in Counties Manukau, May 2014 Priority groups and current service provision, to inform gap analysis. Vicki Evans, CM Health. February 2015. Smokefree Pregnancy Incentives Project: Final Evaluation Report. Resonance Research. January 2015. Key themes and qualitative feedback – understanding our smoking population. Collated from internal planning workshop with smoking cessation practitioners. 2014. Smoking prevalence for the population of Counties Manukau: Early results from Census 2013. Doone Winnard, Wing Cheuk Chan, Vicki Evans; CM Health. December 2013. The population who smoke in Counties Manukau. Presentation at internal planning workshop. May 2014. Page 33 of 35 Appendix One: Road Map - Smokefree Aotearoa 2025 Government Goal Healthier New Zealanders Fewer deaths and harm from tobacco use with focus on maximizing benefit for Māori and Pacific people SMOKEFREE AOTEAROA/NEW ZEALAND 2025 Objectives More Support for Quitting Effective Policy Reduced Initiation All current smokers to quit Control of tobacco supply, price and availability No one, especially children, become addicted to smoking Increase in Quitting Outcomes Current smokers are motivated and enabled to quit and remain smokefree. Cessation Impacts of Tobacco Control Sector Activities Increased tobacco control mass media. Comprehensive cessation services tailored to community needs Best cessation technologies and services used Policy response to electronic nicotine delivery systems Demand & Supply Reduction Protection of Children Tobacco is difficult to supply and to purchase. Children and young people are not exposed to smoking or to tobacco marketing. Legislation & Regulation Public Support Plain packaging Increase price of tobacco products Effective product warnings Restrict and reduce tobacco supply Control tobacco product content Full FCTC implementation Expansion of smokefree settings, including smokefree cars New Zealanders know about and support 2025 goal Smokefree support increases New Zealanders completely mistrust the tobacco industry WORKING TOGETHER Cessation Tobacco Control Sector Activities Interventions in primary, secondary and public health care All services evidence based Existing and emerging effective treatments funded Whānau ora Services to priority populations Innovative cessation methods are encouraged Research and Evaluation Monitoring of tobacco use Monitoring of quitting behaviours and attitudes Evaluation of interventions Monitoring of industry Academic research Page 34 of 35 Policy Engage national decision makers Engage national influencers Review relevant existing and overseas laws Advise and inform policy processes Community Engagement Local activities to make communities smokefree and protect children from exposure to tobacco Engagement with decision makers and media Raise local awareness of Smokefree 2025 goal Monitoring and Enforcement Monitoring of retail outlets Enforcement of smokefree laws and regulations Monitoring of tobacco industry practices, incl. marketing Marketing Unpaid Media/PR Paid Media Communications Signage Branding Events RESEARCH AND EVIDENCE Comprehensive research and evaluation to underpin policy, advocacy and programme development. Page 35 of 35