Course pre-reading and quiz
advertisement

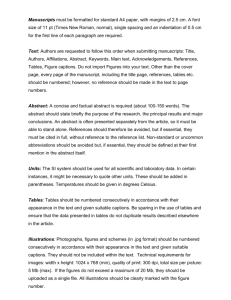
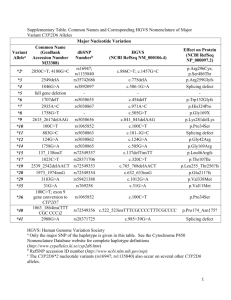
Drug interactions: a look at timing, genetic interplay and tips for recognizing and preventing them in clinical practice Presented by Brian Hocum, PharmD Personalized Prescribing Clinical Pharmacist, Genelex Corporation Washington State University College of Pharmacy Adjunct Faculty Member Learning Objectives 1. 2. 3. 4. Examine the time component involved in drug interactions Recognize the interplay between drugs and genetics Identify a drug interaction in a patient with a problem Predict a drug interaction in a patient that you want to prescribe for Commitment to change When I suspect drug interactions in my practice I will consider inter-individual variation of the CYP450 enzyme system and the timing involved when evaluating the patient. Pre-assessment Case Study: Drug Interaction-Induced Anxiety Chief Complaint: A 72-year-old male with no known drug allergies presented to the ER with a chief complaint of feeling “lightheaded, panicky and slight difficulty breathing.” The panic-like onset first developed three days earlier, reoccurred a couple of times throughout the day, and seemed to be getting more frequent. When the physician entered the exam room, the patient was pacing back and forth and in apparent discomfort. He had normal vital signs except slight tachycardia. The patient had no prior history of panic attacks. At the time of admittance, the patient was taking the following medications: Methadone 20 mg po q 6 hours prn Promethazine 25 mg po q 6 hours Trazodone 50 mg po QHS Zolpidem 10 mg po QHS Simvastatin 40 mg po QHS Lisinopril/HCTZ 20/12.5 mg po QAM ASA 81 mg po QAM Tamsulosin 0.4 mg po QAM History of Present Illness: Ten days earlier the patient was changed from hydrocodone/acetaminophen to methadone because hydrocodone was no longer working well. After several days on methadone, the patient requested medication for nausea and promethazine was prescribed. The patient began feeling “different” and stopped the promethazine for a day only to start again because stopping didn’t seem to help. Plan: After a complete history and exam, the physician diagnosed the patient with possible mild serotonin syndrome and akathisia as a result of an unknown drug interaction. Lorazepam IV was prescribed for acute panic relief and promethazine was discontinued. Discussion: The speaker, a clinical pharmacist who specializes in drug interactions discussed this case with the ER physician and used drug interaction software (YouScript®) to identify the suspected drug interaction. YouScript predicted that both methadone and promethazine inhibited the metabolism of trazodone’s metabolite, m-chlorophenylpiperazine (mcPP), through the CYP2D6 enzyme. mcPP is known to have hallucinogenic and dysphoric effects. 1,2,3 Image Source: www.youscript.net Questions 1. What drug interaction pattern is represented in this case? (circle one) a. Pharmacodynamic b. Pharmacokinetic: immediate c. Pharmacokinetic: 1 to 5 days d. Pharmacokinetic: Weeks 2. Inhibition based interactions present more quickly than induction based interactions? a. True b. False 3. Since mcPP is metabolized by CYP2D6, a patient with the CYP2D6 Poor Metabolizer phenotype may have similar problems with trazodone? a. True b. False References 1. Hocum MD, Brian (Emergency Medicine, St. Joseph Regional Hospital, Lewiston, Idaho). Conversation with: Brian Hocum, PharmD (Genelex, Seatte, WA). 2013 Spring. 2. Logan BK, Constantino AG, Rieders EF, Sanders D. Trazodone, metachlorophenylpiperazine (an hallucinogenic drug and trazodone metabolite), and the hallucinogen trifluoromethylphenylpiperazine crossreact with the EMIT®II ecstasy immunoassay in urine. J Anal Toxicol. 2010 Nov;34(9):587-9. PMID: 21073812. 3. Kast RE. Trazodone generates m-CPP: in 2008 risks from m-CPP might outweigh benefits of trazodone. World J Biol Psychiatry. 2009;10(4 Pt 2):682-5. PMID: 19384678. Answer key (pre-assessment) 1. C 2. A 3. A