diabetes breathing
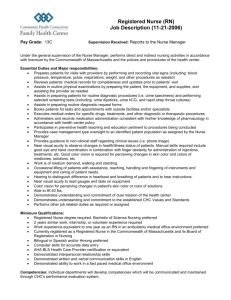
advertisement

Medical Surgical Questions From Lippincott's_Review_for_NCLEX Nursing Care of Clients with Disorders of the Pituitary Gland After suffering head trauma, a client develops signs and symptoms of diabetes insipidus. 1. Which characteristic symptom of the client’s disorder would the nurse expect to fi nd during an assessment? [ ] 1. Polyphagia [ ] 2. Polyuria [ ] 3. Glycosuria [ ] 4. Hyperglycemia 2. How does the nurse expect the urine that is collected for a routine urinalysis to appear? [ ] 1. Tea-colored [ ] 2. Pale yellow [ ] 3. Colorless [ ] 4. Light pink 3. Which nursing intervention is essential for monitoring the client’s condition? [ ] 1. Measuring intake and output [ ] 2. Analyzing blood glucose levels [ ] 3. Inserting a Foley catheter [ ] 4. Sending urine samples to the laboratory The nursing care plan indicates that the client must be weighed each day. 4. When directing the nursing assistant to weigh the client, which instruction is most important for obtaining accurate data? [ ] 1. Have the client stand on a bedside scale. [ ] 2. Weigh the client at the same time each day. [ ] 3. Ask that slippers be removed when being weighed. [ ] 4. Ask about the client’s pre-disease weight. The client is treated with intranasal lypressin (Diapid), 2 sprays q.i.d. and as needed. 5. The nurse observes the client self-administering the medication. Which action indicates that the client is using the medication correctly? [ ] 1. The client shakes the medication vigorously [ ] 2. The client’s head is tilted to the side. [ ] 3. The client inverts the drug container. [ ] 4. The client inhales with each spray. 6. Before the client is discharged, the physician orders lypressin (Diapid) to be administered p.r.n. When instructing the client about how to take this drug at home, the nurse tells the client to administer the drug when experiencing which sign or symptom? [ ] 1. Increased thirst [ ] 2. Onset of a headache [ ] 3. Dark yellow urine [ ] 4. A runny nose The nurse is assessing a client who is experiencing signs and symptoms related to a diagnosis of acromegaly. 7. During the physical assessment of this client, which fi nding is the nurse most likely to observe? [ ] 1. Shortened height [ ] 2. Enlarged hands [ ] 3. Gonadal atrophy [ ] 4. Loss of teeth 8. Which nursing diagnosis should the nursing team consider when developing this client’s care plan? [ ] 1. Activity intolerance [ ] 2. Self-care defi cit [ ] 3. Ineffective breathing [ ] 4. Impaired swallowing Because medical treatment was unsuccessful, the client with acromegaly is scheduled for a trans-sphenoidal hypophysectomy. The night before surgery, the nurse provides the client with information about what to expect during the postoperative period. 9. Which statement by the client indicates a misunderstanding of the expected surgical outcome? [ ] 1. “My appearance will gradually become normal.” [ ] 2. “I’ll need to take replacement hormones.” [ ] 3. “I’ll need to see my physician regularly.” [ ] 4. “The surgical incision will be inconspicuous.” 10. Immediately after surgery, the nurse assesses the client for bleeding. Where is the best location to assess for bleeding? [ ] 1. The skull [ ] 2. The nose [ ] 3. The ear canal [ ] 4. The tongue Nursing Care of Clients with Disorders of the Thyroid Gland A 35-year-old seeks medical attention to determine the reason menstruation has ceased. The physician orders a radioactive iodine uptake test. 11. After the test, the nurse provides the client with instructions. Which statement of the nurse is most accurate? [ ] 1. “You must remain isolated until the radiation level decreases suffi ciently.” [ ] 2. “You’re free to go without further precautionary instructions.” [ ] 3. “You must follow special precautions for a short period of time.” [ ] 4. “You’ll be given an antidote to reduce the radioactivity level.” The results of the diagnostic tests confi rm that the client has myxedema. 12. In addition to amenorrhea, which other signs of myxedema is the nurse likely to observe in this client? Select all that apply. [ ] 1. Hoarse, raspy voice [ ] 2. Oily skin with large pores [ ] 3. Thin trunk and extremities [ ] 4. Extreme restlessness [ ] 5. Low body temperature [ ] 6. Decreased blood pressure 13. When the nurse conducts an admission history, which subjective symptom is the client likely to describe? [ ] 1. Diffi culty urinating [ ] 2. Intolerance to cold [ ] 3. Profuse perspiration [ ] 4. Excessive appetite The client with myxedema is treated with levothyroxine (Synthroid), one tablet P.O. every day. 14. Which statement provides the best evidence that the client understands the prescribed drug therapy? [ ] 1. “I must take this drug after meals.” [ ] 2. “I should avoid driving when sleepy.” [ ] 3. “I’ll need to take this drug life-long.” [ ] 4. “I can skip a dose if I’m nauseated.” 15. Because the client is receiving levothyroxine (Synthroid) for the fi rst time, the nurse recognizes the need to observe the client for adverse effects related to thyroid replacement therapy. For which signs and symptoms should the nurse assess? Select all that apply. [ ] 1. Dyspnea [ ] 2. Palpitations [ ] 3. Excessive bruising [ ] 4. Raised, red rash [ ] 5. Hyperactivity [ ] 6. Insomnia A client seeks medical attention after noticing fullness in the neck. After several diagnostic tests, a large endemic goiter is diagnosed. 16. As the nurse provides care for the client newly diagnosed with a large goiter, which interventions should be implemented? Select all that apply. [ ] 1. Observe the client’s respiratory status [ ] 2. Elevate the head of the client’s bed [ ] 3. Provide a diet high in iodized salt [ ] 4. Obtain an order for a soft diet [ ] 5. Assess for high fever [ ] 6. Administer prescribed antibiotics A client is undergoing treatment for Graves’ disease. 17. Which characteristic facial feature would the nurse expect to note during a physical examination of this client? [ ] 1. Bulging eyes [ ] 2. Bulbous nose [ ] 3. Thick lips [ ] 4. Large tongue The physician prescribes propylthiouracil (Propyl-Thyracil) to treat the client’s condition. 18. Before administering this medication, what is essential for the nurse to ask the client? [ ] 1. “Do you have trouble swallowing?” [ ] 2. “Do you prefer a liquid form of medication?” [ ] 3. “Have you had digestive disorders in the past?” [ ] 4. “Is there a possibility you could be pregnant?” 19. Because propylthiouracil (Propyl-Thyracil) can cause agranulocytosis, the nurse advises the client to notify the physician if which problem occurs? [ ] 1. Persistent sore throat [ ] 2. Occasional heart palpitations [ ] 3. Fatigue on exertion [ ] 4. Prolonged bleeding with trauma After diagnostic testing, a client with Graves’ disease is informed that it is necessary to undergo a subtotal thyroidectomy. The physician prescribes potassium iodide (Lugol’s solution) 4 gtt P.O. to be taken for 10 days before the scheduled surgery. 20. When the nurse teaches the client how to self-administer potassium iodide (Lugol’s solution), which instruction is most appropriate? [ ] 1. Swallow the drug quickly. [ ] 2. Take the drug before meals. [ ] 3. Dilute the drug in fruit juice. [ ] 4. Chill the drug before taking it. The client asks the nurse to explain the purpose of the preoperative drug therapy. 21. Which response by the nurse about potassium iodide (Lugol’s solution) is correct? [ ] 1. It fi rms the gland so it is easily removed. [ ] 2. It decreases the postoperative recovery time. [ ] 3. It decreases the risk of postoperative bleeding. [ ] 4. It eliminates the need for hormone replacement. 22. Preoperatively, which information is most important to teach the client before the subtotal thyroidectomy? [ ] 1. Techniques for changing positions [ ] 2. Reasons for performing leg exercises [ ] 3. The necessity for daily dressing changes [ ] 4. Postoperative use of the incentive spirometer 23. To prepare for potential postoperative complications related to the thyroidectomy, which item is necessary to keep at the client’s bedside? [ ] 1. Dressing change kit [ ] 2. Tracheostomy tray [ ] 3. Ampule of epinephrine [ ] 4. Mechanical ventilator After surgery, the client is returned to the nursing unit in stable condition. 24. In which position should the client be maintained after the subtotal thyroidectomy? [ ] 1. Supine [ ] 2. Sims’ [ ] 3. Semi-Fowler’s [ ] 4. Recumbent 25. Postoperatively, the nurse should consult the physician before encouraging the client who has undergone a subtotal thyroidectomy to perform which activity? [ ] 1. Forced coughing [ ] 2. Deep breathing [ ] 3. Ambulating [ ] 4. Dangling legs 26. Which intervention is most appropriate to add to the client’s care plan when monitoring for incisional bleeding after a subtotal thyroidectomy? [ ] 1. Observe for signs of hypovolemic shock. [ ] 2. Assess for dampness at the back of the client’s neck. [ ] 3. Remove the dressing to directly inspect the wound. [ ] 4. Weigh all gauze dressings before and after changing. 27. Which assessment technique is most appropriate when checking for laryngeal nerve damage in a client who has had a thyroidectomy? [ ] 1. Turning the client’s head from side to side [ ] 2. Observing the client swallowing [ ] 3. Looking for tracheal deviation [ ] 4. Asking the client to say “Ah” 28. The nurse should assess for hypocalcemia based on which client statements after a subtotal thyroidectomy? Select all that apply. [ ] 1. “I feel like I could vomit.” [ ] 2. “My lips feel numb and tingly.” [ ] 3. “Light seems to bother my eyes.” [ ] 4. “I feel weak when I walk.” [ ] 5. “I have cramps in my legs.” [ ] 6. “I feel like my throat is constricting.” Because the client is exhibiting signs and symptoms of hypocalcemia after surgery, the nurse assesses for Chvostek’s sign. 29. Place an X in the area of the head that the nurse should assess to determine a positive or negative Chvostek’s sign. A day after a client undergoes subtotal thyroidectomy, the nurse suspects that the client is developing clinical manifestations related to thyroid crisis. 30. Which signs and symptoms related to thyroid crisis require immediate notifi cation of the physician? Select all that apply. [ ] 1. High fever [ ] 2. Falling blood pressure [ ] 3. Regular noisy respirations [ ] 4. Hand spasms [ ] 5. Heart palpitations [ ] 6. Decreased urine output Based on the client’s clinical presentation, a diagnosis of thyroid crisis is made. 31. Which nursing interventions are most appropriate at this time? Select all that apply. [ ] 1. Take the client’s vital signs at least every hour. [ ] 2. Assess Trousseau’s sign every shift. [ ] 3. Limit the client’s activity. [ ] 4. Administer antipyretics per order. [ ] 5. Encourage a diet high in iodized salt. [ ] 6. Make sure I.V. calcium gluconate is available. 32. At the beginning of thyroid replacement therapy after a thyroidectomy, the nurse must monitor the client closely for side effects. Which fi ndings would the nurse expect to detect if the client is receiving more thyroid hormone replacement than required? Select all that apply. [ ] 1. Hyperglycemia [ ] 2. Tachycardia [ ] 3. Insomnia [ ] 4. Hirsutism [ ] 5. Tremors [ ] 6. Hypertension Nursing Care of Clients with Disorders of the Parathyroid Glands A client who develops a benign parathyroid tumor manifests signs of hyperparathyroidism. 33. When the nurse reviews the client’s history, which assessment fi nding is closely associated with the client’s diagnosis? [ ] 1. Nightly leg cramps [ ] 2. Recurrent kidney stones [ ] 3. Loose bowel movements [ ] 4. Excessive energy level The nursing assistant assigned to this client asks why the care plan indicates that the client is at risk for falls and injury. 34. Which is the best explanation by the nurse concerning an effect of hyperparathyroidism? [ ] 1. The inability to maintain balance [ ] 2. The risk of developing seizures [ ] 3. Fainting when changing positions [ ] 4. Pathologic bone fractures The client has three of the four lobes of the parathyroid gland surgically removed. 35. After the client returns from surgery and resumes eating, the nurse should encourage the client to eat foods from which food group? [ ] 1. Bread and cereals [ ] 2. Milk and cheese [ ] 3. Meat and seafood [ ] 4. Fruit and vegetables A client diagnosed with hypoparathyroidism develops tetany and comes to the emergency department for treatment. 36. Which I.V. medication can the nurse expect the physician to order to treat the client’s condition? [ ] 1. Calcium gluconate [ ] 2. Ferrous sulfate [ ] 3. Potassium chloride [ ] 4. Sodium bicarbonate Nursing Care of Clients with Disorders of the Adrenal Glands The nurse is caring for a client with a disorder of the adrenal glands. 37. Place an X where the adrenal glands are located in the diagram below. The nurse cares for a client with Addison’s disease. 38. Which characteristic fi ndings would the nurse expect to assess in a client with Addison’s disease? Select all that apply. [ ] 1. Salt craving [ ] 2. Skin blemishes [ ] 3. Moon-shaped face [ ] 4. Bronzed skin [ ] 5. Hypoglycemia [ ] 6. Weight loss 39. Which nursing assessment is most helpful in evaluating the status of a client with Addison’s disease? [ ] 1. Blood pressure [ ] 2. Bowel sounds [ ] 3. Breath sounds [ ] 4. Heart sounds The client’s care plan indicates that the nurse should assist the client in selecting foods that are good sources of sodium as part of the treatment for Addison’s disease. 40. If the following foods are available, which one should the nurse recommend? [ ] 1. Graham crackers [ ] 2. Cheddar cheese [ ] 3. Raw carrots [ ] 4. Canned fruit The nurse documents that the client has recurrent episodes of hypoglycemia. 41. If a regular diet is ordered, which between-meal snack should the nurse offer to help regulate the client’s blood glucose level? [ ] 1. Lemonade and peanuts [ ] 2. Cola and potato chips [ ] 3. Coffee and a muffi n [ ] 4. Milk and crackers 42. Because this client is at risk for developing addisonian crisis, which is also known as acute adrenal insuffi ciency and adrenal crisis, a life-threatening condition, what should the nurse instruct the client to avoid? [ ] 1. Stress-producing situations [ ] 2. Consuming alcoholic beverages [ ] 3. Eating complex carbohydrates [ ] 4. Getting too little sleep 43. A client with Addison’s disease is admitted to the hospital with a history of nausea and vomiting for the past 3 days. The registered nurse (RN) administers methylprednisolone (Solu-Medrol), a glucocorticoid, intravenously. Which nursing action is most important for the licensed practical nurse (LPN) to implement in the client’s plan of care? [ ] 1. Glucometer measurements [ ] 2. Intake and output volumes [ ] 3. Daily weights [ ] 4. Frequent oral care A 38-year-old client is hospitalized after developing symptoms that resemble those of Cushing’s syndrome. The nurse completes admission documentation. 44. Based on the client’s condition, which fi ndings will the nurse most likely document after completing the initial physical assessment? Select all that apply. [ ] 1. The client has very thin legs. [ ] 2. The client looks emaciated. [ ] 3. The client has bulging eyes. [ ] 4. The client’s skin is pale. [ ] 5. The client has bruising. [ ] 6. The client’s scalp hair is thin. The nurse develops the care plan and documents an expected outcome that states, “The client will be free of infection during the hospital stay.” 45. Based on the nurse’s understanding of this disease process, for what reasons is the expected outcome justifi ed? Select all that apply. [ ] 1. The client is at risk for skin breakdown related to thinning of the skin and edema. [ ] 2. Wound healing is prolonged in clients with this disorder. [ ] 3. The immunosuppressive effects of the disorder mask symptoms of infection. [ ] 4. The client is at risk for aspiration pneumonia related to laryngeal nerve damage. [ ] 5. The client’s admission white blood cell count is elevated. [ ] 6. The client’s admission temperature is within normal limits. The physician orders a 24-hour urine collection to aid in the diagnosis of Cushing’s syndrome. 46. The nurse is most accurate in telling the client that the urine collection will begin when? [ ] 1. With the client’s next voiding [ ] 2. After the client’s next voiding [ ] 3. After drinking a pitcher of water [ ] 4. With the fi rst voiding in the morning 47. Which statement is correct concerning the collection of urine for a 24-hour specimen? [ ] 1. The volume of each voiding is measured and recorded. [ ] 2. The urine is placed in a container of preservative. [ ] 3. Each voiding is taken immediately to the laboratory. [ ] 4. The client voids directly into the specimen container. After the health care team meets to discuss the client’s nursing needs, the nursing diagnosis “Disturbed body image” is added to the care plan. 48. The best rationale for adding this nursing diagnosis to the care plan in the case of a female is that females with Cushing’s syndrome typically experience which physiologic effect? [ ] 1. Masculine characteristics [ ] 2. Heavy menstrual fl ow [ ] 3. Extreme weight loss [ ] 4. Large, pendulous breasts Diagnostic tests confi rm that the client’s adrenal glands are producing excessive amounts of adrenocortical hormones. 49. When the nurse explains the disorder to the client’s spouse, it is accurate to stress that the client is also likely to experience which effect? [ ] 1. Anxiety and occasional panic attacks [ ] 2. Depression and suicidal tendencies [ ] 3. Impulsiveness and poor self-control [ ] 4. Forgetfulness and memory changes The physician orders a low-sodium diet to help treat the client’s Cushing’s syndrome. 50. Which action by the nurse provides the best data for monitoring the client’s therapeutic response to sodium restriction? [ ] 1. Monitoring sodium intake [ ] 2. Measuring pedal edema [ ] 3. Assessing skin turgor [ ] 4. Weighing the client 51. Which nursing interventions are most appropriate for managing the basic needs of a client with Cushing’s syndrome? Select all that apply. [ ] 1. Have the client sleep on a convoluted (egg-crate) foam mattress. [ ] 2. Ambulate the client at frequent intervals. [ ] 3. Advise the client to ask for assistance when getting up. [ ] 4. Offer high-carbohydrate nourishment. [ ] 5. Check the client frequently for suicidal ideation. [ ] 6. Instruct the client to wear loose-fi tting clothing. Eventually, the client undergoes a bilateral adrenalectomy to correct Cushing’s syndrome. 52. To detect complications of surgery in the immediate postoperative period, which assessment component is most important for the nurse to monitor? [ ] 1. Blood pressure [ ] 2. Urine output [ ] 3. Temperature [ ] 4. Specifi c gravity 53. Which documentation fi nding provides the best indication that the client has successfully avoided an adrenal (addisonian) crisis after surgery? [ ] 1. Urine output is approximately 2,000 mL/day. [ ] 2. The client’s pedal edema has lessened. [ ] 3. Capillary blood glucose level is within normal limits. [ ] 4. Vital signs are within preoperative ranges. 54. Based on the knowledge that clients with Cushing’s syndrome heal slowly, which nursing measure is most appropriate during the client’s postoperative period? [ ] 1. Monitoring infusion of I.V. antibiotics [ ] 2. Removing tape toward the incision site [ ] 3. Increasing the client’s dietary protein intake [ ] 4. Covering the wound with gauze 55. Which statement provides the best evidence that the client who has undergone a bilateral adrenalectomy understands the postoperative course? [ ] 1. “I should avoid people with infectious diseases.” [ ] 2. “I need to limit my fl uid intake to 1 quart per day.” [ ] 3. “My appearance will never be the same as it was before.” [ ] 4. “No other treatment is necessary after I recover from surgery.” Nursing Care of Clients with Pancreatic Endocrine Disorders A 23-year-old client manifests symptoms of hyperinsulinism. 56. In response to a question about timing of symptoms during the nursing history, when is the client most likely to describe that symptoms typically occur? [ ] 1. After fasting more than 6 hours [ ] 2. About 2 hours after eating a meal [ ] 3. Late in the evening, before bedtime [ ] 4. Early in the morning, before breakfast A glucose tolerance test is ordered to determine if the client has functional hypoglycemia. 57. Which instruction by the nurse concerning the test procedure is most accurate? [ ] 1. “You need to eat a large meal just before the test.” [ ] 2. “Bring a voided urine specimen to the laboratory.” [ ] 3. “You can drink coffee or tea in the morning before the test.” [ ] 4. “You will be given a sweetened drink before the test.” 58. To reduce or eliminate the symptoms that a client with functional hypoglycemia experiences, it is best for the nurse to recommend eating fi ve or six small meals containing which nutrient? [ ] 1. Simple sugars [ ] 2. Complete proteins [ ] 3. Complex carbohydrates [ ] 4. Unsaturated fats 59. Which of the following provides the best evidence that the dietary measures to control functional hypoglycemia are therapeutic? [ ] 1. The client experiences fewer incidences of weakness and tremors. [ ] 2. The client experiences fewer incidences of thirst and dry mouth. [ ] 3. The client experiences fewer incidences of muscle spasms and fatigue. [ ] 4. The client experiences fewer incidences of hunger and abdominal cramps. A nurse participates in a community-wide screening to identify adults who may have undiagnosed diabetes mellitus. 60. If the screening includes a measurement of postprandial blood glucose, the nurse is correct in explaining that blood will be drawn at which time? [ ] 1. Approximately 2 hours before breakfast [ ] 2. Approximately 2 hours after a meal [ ] 3. Approximately 2 hours before bedtime [ ] 4. Approximately 2 hours after fasting 61. Which statement indicates that a client with an elevated 2-hour postprandial blood glucose level understands the signifi cance of the screening test? [ ] 1. “I need to eat less frequently.” [ ] 2. “I need to stop eating candy.” [ ] 3. “I need to consult my physician.” [ ] 4. “I need to begin taking insulin.” 62. Which signs and symptoms are most appropriate for the nurse to investigate when screening adults who have come to have their blood glucose tested? [ ] 1. Diarrhea, anorexia, and weight gain [ ] 2. Constipation, weight loss, and thirst [ ] 3. Polycholia, polyemia, and polyplegia [ ] 4. Polyuria, polydipsia, and polyphagia After the screening test, one client is referred to a physician for additional follow-up. Further diagnostic tests confi rm that the client has type 2 diabetes mellitus. 63. When given the news, the client denies the diagnosis and becomes angry, stating there has been a mistake in the tests. Which nursing action is most appropriate at this time? [ ] 1. Emphasizing the importance of treatment [ ] 2. Reassuring the client that the disease is easily managed [ ] 3. Explaining that many people live with diabetes [ ] 4. Listening as the client expresses current feelings The client with newly diagnosed type 2 diabetes mellitus is referred to the diabetes clinic for teaching. 64. When the client asks the nurse why regular exercise is recommended for diabetic clients, the best answer is that exercise tends to facilitate which positive outcome? [ ] 1. Regular exercise helps to control weight. [ ] 2. Regular exercise helps to decrease appetite. [ ] 3. Regular exercise helps to reduce blood glucose levels. [ ] 4. Regular exercise helps to improve circulation to the feet. A dietitian explains how to use the American Diabetes Association exchange list. 65. Which statement by the client provides the best evidence that the client understands the principle of an exchange list for meal planning? [ ] 1. “I can eat one serving from each category on the exchange list per day.” [ ] 2. “Measured amounts of food in each category are equal to one another.” [ ] 3. “The number of servings from the exchange list is unlimited.” [ ] 4. “I need to use the exchange list to determine the nutrition in food.” 66. The nurse knows the diabetic client understands what “free” foods on the exchange list means if the client excludes which one of the following from a meal plan? [ ] 1. Iced tea [ ] 2. Flavored water [ ] 3. Light beer [ ] 4. Club soda The physician prescribes glyburide (DiaBeta) orally for the client to treat diabetes. 68. When the client asks why a diabetic relative cannot take insulin orally, what is the best answer? [ ] 1. Insulin is inactivated by digestive enzymes. [ ] 2. Insulin is absorbed too quickly in the stomach. [ ] 3. Insulin is irritating to the gastric mucosa. [ ] 4. Insulin is incompatible with many foods. 69. The diabetic client tells the nurse that breakfast is always skipped. Which response by the nurse is most appropriate? [ ] 1. “If you drink a glass of milk and eat a breakfast bar, that will be suffi cient for breakfast.” [ ] 2. “You should eat each meal and snack at the same time each day.” [ ] 3. “If you skip breakfast, eat a high-calorie snack at midmorning.” [ ] 4. “Wait to take your medication until you eat your fi rst meal of the day.” After the client is discharged from the hospital, the physician wants the client to continue to self-monitor the response to the diet and medication management. 70. Which monitoring approach is best for the nurse to recommend? [ ] 1. Testing the urine with a chemical reagent strip [ ] 2. Using a glucometer to check capillary blood glucose levels [ ] 3. Having laboratory personnel draw venous blood samples [ ] 4. Arranging for testing by a home health agency Nurse Emergency medical personnel bring a client who is lethargic and confused to the emergency department. A tentative diagnosis of type 1 diabetes mellitus and diabetic ketoacidosis (DKA) is made. 71. Which assessment fi ndings would the nurse expect to document if the client has DKA? Select all that apply. [ ] 1. The client is hypertensive and tachycardic. [ ] 2. The client is dyspneic and hypotensive. [ ] 3. The client breathes noisily and smells of acetone. [ ] 4. The client stares blankly and smells of alcohol. [ ] 5. The client has warm, fl ushed skin and has vomited. [ ] 6. The client complains of abdominal pain and is thirsty. The nurse documents that Kussmaul’s respirations were detected during the initial assessment. 72. Which respiratory pattern is the best description of the client’s breathing? [ ] 1. Fast, deep, labored respirations [ ] 2. Shallow respirations, alternating with apnea [ ] 3. Slow inhalation and exhalation through pursed lips [ ] 4. Shortness of breath with pauses The nurse plans to monitor the client’s response to insulin therapy closely with an electronic glucometer and instructs the emergency department technician to take periodic capillary blood glucose measurements. 73. Which techniques are correct when using an electronic glucometer to monitor the client’s capillary blood glucose level? Select all that apply. [ ] 1. Clean the client’s fi nger with povidone-iodine (Betadine). [ ] 2. Take a set of vital signs before the test. [ ] 3. Pierce the central pad of the client’s fi nger. [ ] 4. Apply a large drop of blood to a test strip or area. [ ] 5. Don gloves before piercing the client’s fi nger. [ ] 6. Perform a quality control before the test. After using the glucometer, the emergency department technician reports to the nurse that the client’s capillary blood glucose measures 498 mg/dL. 74. Based on the client’s blood glucose measurement, the nurse immediately reevaluates the client. Which physician orders should the nurse anticipate? Select all that apply. [ ] 1. STAT serum blood glucose [ ] 2. Intravenous regular insulin [ ] 3. Vital signs every 2 hours [ ] 4. A diet of six small, frequent meals [ ] 5. Electronic glucometer measurements before meals and at bedtime [ ] 6. Continuous cardiac monitoring After stabilization in the emergency department, the client with diabetic ketoacidosis (DKA) is admitted to a stepdown unit for further observation and treatment. After several episodes of hyperglycemia, the physician orders sliding-scale regular insulin administered subcutaneously for the client. 75. How soon after administering the client’s dose of regular insulin subcutaneously should the nurse assess for signs of hypoglycemia? [ ] 1. 5 minutes later [ ] 2. 30 minutes later [ ] 3. 6 hours later [ ] 4. 10 hours later 76. The nurse teaches the client with newly diagnosed diabetes mellitus about the signs and symptoms of hypoglycemia. Which of the following should the nurse stress in teaching? Select all that apply. [ ] 1. Sleepiness [ ] 2. Shakiness [ ] 3. Thirst [ ] 4. Hunger [ ] 5. Diaphoresis [ ] 6. Confusion During the midmorning after receiving insulin, the client reports feeling weak, shaky, and dizzy. The nurse asks the nursing assistant to obtain a capillary blood glucose measurement with a glucometer. 77. The nursing assistant reports to the nurse that the client’s blood glucose reading is 58 mg/dL. What is the most appropriate nursing action at this time? [ ] 1. Administer the next scheduled dose of insulin. [ ] 2. Give the client ¼ cup of sweet fruit juice. [ ] 3. Report the client’s symptoms to the physician. [ ] 4. Perform a complete head-to-toe assessment. The client with type 1 diabetes mellitus must learn to combine two insulins—regular and intermediate-acting—and self-administer the injection before being discharged. 78. Which action is the best indication that the client needs more practice in combining two insulins in one syringe? [ ] 1. The client rolls the vial of intermediate-acting insulin to mix it with its additive. [ ] 2. The client instills air into both the fast-acting and intermediate-acting insulin vials. [ ] 3. The client instills the intermediate-acting insulin into the vial of rapid-acting insulin. [ ] 4. The client inverts each vial before withdrawing the specifi ed amount of insulin. 79. When the client practices self-administration of the insulin, which action is correct? [ ] 1. Piercing the skin at a 30-degree angle [ ] 2. Using a syringe calibrated in minims [ ] 3. Using a 29-gauge needle on the syringe [ ] 4. Rotating abdominal sites for each injection The nurse implements a diabetes teaching plan in anticipation of the client’s discharge. 81. Which statement indicates that the client has misunderstood the nurse’s teaching? [ ] 1. “I may need more insulin during times of stress.” [ ] 2. “I may need more food when exercising strenuously.” [ ] 3. “My insulin needs may change as I get older.” [ ] 4. “My dependence on insulin may stop eventually.” 82. The nurse discusses the long-term effects of diabetes mellitus with the client and realizes that the client needs further teaching when the client identifi es which occurrence as a complication of this disease? [ ] 1. Blindness [ ] 2. Stroke [ ] 3. Renal failure [ ] 4. Liver failure 83. When the client asks how to store an opened vial of insulin, which answer by the nurse offers the most correct instruction? [ ] 1. The best place for storing insulin is in the bathroom, close to the shower. [ ] 2. The best place to store insulin is in the refrigerator. [ ] 3. The best way to store insulin is at room temperature. [ ] 4. The best place for storing insulin is in a warm location but out of sunlight. The nurse includes foot care as a component of diabetes teaching. 84. Which statement by the client about foot care indicates a need for further teaching? [ ] 1. “I need to inspect my feet daily.” [ ] 2. “I should soak my feet each day.” [ ] 3. “I need to wear shoes whenever I’m not sleeping.” [ ] 4. “I need to schedule regular appointments with the podiatrist.” After 3 months, the client returns for a follow-up appointment with the physician to evaluate the progress of s elf-care. 85. Which information is most important for the nurse to elicit from the client to effectively evaluate compliance with the prescribed therapy? [ ] 1. The dosage and frequency of insulin administration [ ] 2. The client’s glucose monitoring records for the past week [ ] 3. The client’s weight and vital signs before the offi ce interview [ ] 4. The symptoms experienced in the past month 86. Which laboratory test is most important for the nurse to monitor to determine how effectively the client’s diabetes is being managed? [ ] 1. Fasting blood glucose [ ] 2. Blood chemistry profi le [ ] 3. Complete blood count [ ] 4. Glycosylated hemoglobin (HbA1c) During the physician’s visit, the client reports researching the use of insulin pumps on the Internet and wants to know the possibility of being a candidate. After evaluating the client and discussing the request, the physician asks the nurse to provide instructions about management of the client’s diabetes using a continuous insulin infusion pump. 87. The nurse teaches the client how the infusion pump operates and correctly points out that the infusion is typically administered in which location? [ ] 1. In a vein within the nondominant hand [ ] 2. In the muscular tissue of the thigh [ ] 3. In the subcutaneous tissue of the abdomen below the belt line [ ] 4. In an implanted I.V. catheter threaded into the neck The nurse cares for an older client who is insulin dependent and lives in a long-term care facility. 88. When developing the client’s care plan, which intervention is most appropriate to add? [ ] 1. Encourage the client to use an electric razor. [ ] 2. Tell the client to fi le rather than cut toenails. [ ] 3. Make sure that the client receives mouth care twice per day. [ ] 4. Advise the client to use deodorant soap when bathing 89. The nurse has prepared 24 units of Humulin N insulin for subcutaneous administration. Identify with an X the preferred location for insulin administration to facilitate rapid absorption. 90. Which sign is most suggestive that a client with type 2 diabetes is developing hyperosmolar hyperglycemic nonketotic syndrome (HHNS)? [ ] 1. The client’s serum glucose level is 650 mg/dL. [ ] 2. The client’s urinary output is 3,000 mL/24 hours. [ ] 3. The client’s skin is cool and moist. [ ] 4. The client’s urine contains acetone. A client with type 1 diabetes mellitus comes to the clinic complaining of persistent bouts of nausea, vomiting, and diarrhea for the past 4 days. The client has skipped insulin injections because of not being able to eat or keep anything down. 91. Which instruction should the nurse give the client about insulin administration during periods of illness? [ ] 1. Monitor blood glucose levels every 2 to 4 hours. [ ] 2. Eat candy or sugar frequently. [ ] 3. Attempt to drink a high-calorie beverage every hour. [ ] 4. Test urine daily for protein. 92. During change of shifts, a nurse discovers that a hospitalized client with diabetes received two doses of insulin. After notifying the physician, which nursing action is most appropriate? [ ] 1. Completing an incident report [ ] 2. Calling the intensive care unit (ICU) [ ] 3. Performing frequent neurologic checks [ ] 4. Monitoring the client’s blood glucose ******************************************************************* From 1Saunders_Comprehensive_Review Practice Questions 571. A client is brought to the emergency department in an unresponsive state, and a diagnosis of hyperglycemic hyperosmolar nonketotic syndrome is made. The nurse would immediately prepare to initiate which of the following anticipated physician’s prescriptions? 1. Endotracheal intubation 2. 100 units of NPH insulin 3. Intravenous infusion of normal saline 4. Intravenous infusion of sodium bicarbonate 572. An external insulin pump is prescribed for a client with diabetes mellitus and the client asks the nurse about the functioning of the pump. The nurse bases the response on the information that the pump: 1. Is timed to release programmed doses of regular or NPH insulin into the bloodstream at specific intervals 2. Continuously infuses small amounts of NPH insulin into the bloodstream while regularly monitoring blood glucose levels 3. Is surgically attached to the pancreas and infuses regular insulin into the pancreas, which in turn releases the insulin into the bloodstream 4. Gives a small continuous dose of regular insulin subcutaneously, and the client can selfadminister a bolus with an additional dose from the pump before each meal 573. A client with a diagnosis of diabetic ketoacidosis (DKA) is being treated in an emergency department. Which finding would a nurse expect to note as confirming this diagnosis? 1. Comatose state 2. Decreased urine output 3. Increased respirations and an increase in pH 4. Elevated blood glucose level and low plasma bicarbonate level 574. A nurse teaches a client with diabetes mellitus about differentiating between hypoglycemia and ketoacidosis. The client demonstrates an understanding of the teaching by stating that a form of glucose should be taken if which of the following symptoms develops? 1. Polyuria 2. Shakiness 3. Blurred vision 4. Fruity breath odor 575. A client with diabetes mellitus demonstrates acute anxiety when first admitted for the treatment of hyperglycemia. The appropriate intervention to decrease the client’s anxiety is to: 1. Administer a sedative. 2. Convey empathy, trust, and respect toward the client. 3. Ignore the signs and symptoms of anxiety so that they will soon disappear. 4. Make sure that the client knows all the correct medical terms to understand what is happening. 576. A nurse provides instructions to a client newly diagnosed with type 1 diabetes mellitus. The nurse recognizes accurate understanding of measures to prevent diabetic ketoacidosis when the client states: 1. “I will stop taking my insulin if I’m too sick to eat.” 2. “I will decrease my insulin dose during times of illness.” 3. “I will adjust my insulin dose according to the level of glucose in my urine.” 4. “I will notify my physician if my blood glucose level is higher than 250 mg/dL.” 577. A client is admitted to a hospital with a diagnosis of diabetic ketoacidosis (DKA). The initial blood glucose level was 950 mg/dL. A continuous intravenous infusion of regular insulin is initiated, along with intravenous rehydration with normal saline. The serum glucose level is now 240 mg/dL. The nurse would next prepare to administer which of the following? 1. Ampule of 50% dextrose 2. NPH insulin subcutaneously 3. Intravenous fluids containing 5% dextrose 4. Phenytoin (Dilantin) for the prevention of seizures 578. A nurse is monitoring a client newly diagnosed with diabetes mellitus for signs of complications. Which of the following, if exhibited in the client, would indicate hyperglycemia and warrant physician notification? 1. Polyuria 2. Diaphoresis 3. Hypertension 4. Increased pulse rate 579. A nurse is preparing a plan of care for a client with diabetes mellitus who has hyperglycemia. The priority nursing diagnosis would be: 1. Deficient knowledge 2. Deficient fluid volume 3. Compromised family coping 4. Imbalanced nutrition, less than body requirements 580. A home health nurse visits a client with a diagnosis of type 1 diabetes mellitus. The client relates a history of vomiting and diarrhea and tells the nurse that no food has been consumed for the last 24 hours. Which additional statement by the client indicates a need for further teaching? 1. “I need to stop my insulin.” 2. “I need to increase my fluid intake.” 3. “I need to monitor my blood glucose every 3 to 4 hours.” 4. “I need to call the physician because of these symptoms.” 581. A nurse is caring for a client after hypophysectomy. The nurse notices clear nasal drainage from the client’s nostril. The initial nursing action would be to: 1. Lower the head of the bed. 2. Test the drainage for glucose. 3. Obtain a culture of the drainage. 4. Continue to observe the drainage. 582. After several diagnostic tests, a client is diagnosed with diabetes insipidus. A nurse performs an assessment on the client, knowing that which symptom is most indicative of this disorder? 1. Fatigue 2. Diarrhea 3. Polydipsia 4. Weight gain 583. A client is admitted to an emergency department, and a diagnosis of myxedema coma is made. Which action would the nurse prepare to carry out initially? 1. Warm the client. 2. Maintain a patent airway. 3. Administer thyroid hormone. 4. Administer fluid replacement. 584. A nurse is caring for a client admitted to the emergency department with diabetic ketoacidosis (DKA). In the acute phase, the priority nursing action is to prepare to: 1. Correct the acidosis. 2. Administer 5% dextrose intravenously. 3. Administer regular insulin intravenously. 4. Apply a monitor for an electrocardiogram. 585. A client with type 1 diabetes mellitus calls the nurse to report recurrent episodes of hypoglycemia with exercising. Which statement by the client indicates an inadequate understanding of the peak action of NPH insulin and exercise? 1. “The best time for me to exercise is after I eat.” 2. “The best time for me to exercise is after breakfast.” 3. “The best time for me to exercise is mid- to late afternoon.” 4. “The best time for me to exercise is after my morning snack.” 586. A nurse is completing an assessment on a client who is being admitted for a diagnostic workup for primary hyperparathyroidism. Which client complaint would be characteristic of this disorder? 1. Diarrhea 2. Polyuria 3. Polyphagia 4. Weight gain 587. A nurse is caring for a postoperative parathyroidectomy client. Which client complaint would indicate that a serious, life-threatening complication may be developing, requiring immediate notification of the physician? 1. Laryngeal stridor 2. Abdominal cramps 3. Difficulty in voiding 4. Mild to moderate incisional pain 588. A client is diagnosed with pheochromocytoma. A nurse prepares a plan of care for the client; while planning, the nurse understands that pheochromocytoma is a condition that: 1. Causes profound hypotension 2. Is manifested by severe hypoglycemia 3. Is not curable and is treated symptomatically 4. Causes the release of excessive amounts of catecholamines 589. A nurse is caring for a client with pheochromocytoma who is scheduled for adrenalectomy. In the preoperative period, the priority nursing action would be to monitor: 1. Vital signs 2. Intake and output 3. Blood urea nitrogen results 4. Urine for glucose and ketones 590. A nurse is performing an assessment on a client with pheochromocytoma. Which of the following assessment data would indicate a potential complication associated with this disorder? 1. A coagulation time of 5 minutes 2. A urinary output of 50 mL per hour 3. A blood urea nitrogen level of 20 mg/dL 4. A heart rate that is 90 beats/min and irregular 591. A nursing instructor asks a student to describe the pathophysiology that occurs in Cushing’s disease. Which statement by the student indicates an accurate understanding of this disorder? 1. “Cushing’s disease results from an oversecretion of insulin.” 2. “Cushing’s disease results from an undersecretion of corticotropic hormones.” 3. “Cushing’s disease results from an undersecretion of mineralocorticoid hormones.” 4. “Cushing’s disease results from an increased pituitary secretion of adrenocorticotropic hormone.” 592. A nurse performs a physical assessment on a client with type 2 diabetes mellitus. Findings include a fasting blood glucose of 120 mg/dL, temperature of 101 _ F, pulse of 88 beats/min, respirations of 22 breaths/min, and blood pressure of 100/72 mm Hg. Which finding would be of most concern to the nurse? 1. Pulse 2. Respiration 3. Temperature 4. Blood pressure 593. A nurse is interviewing a client with type 2 diabetes mellitus. Which statement by the client indicates an understanding of the treatment for this disorder? 1. “I take oral insulin instead of shots.” 2. “By taking these medications, I am able to eat more.” 3. “When I become ill, I need to increase the number of pills I take.” 4. “The medications I’m taking help release the insulin I already make.” 594. A nurse is providing discharge instructions to a client who has Cushing’s syndrome. Which client statement indicates that instructions related to dietary management are understood? 1. “I can eat foods that have a lot of potassium in them.” 2. “I will need to limit the amount of protein in my diet.” 3. “I am fortunate that I can eat all the salty foods I enjoy.” 4. “I am fortunate that I do not need to follow any special diet.” 595. The nurse is caring for a client who is 2 days postoperative following an abdominal hysterectomy. The client has a history of diabetes mellitus and has been receiving regular insulin according to capillary blood glucose testing four times a day. A carbohydrate-controlled diet has been prescribed but the client has been complaining of nausea and is not eating. On entering the client’s room, the nurse finds the client to be confused and diaphoretic. Which action is appropriate at this time? 1. Call a code to obtain needed assistance immediately. 2. Obtain a capillary blood glucose level and perform a focused assessment. 3. Stay with the client and ask the nursing assistant to call the physician for a prescription for intravenous 50% dextrose. 4. Ask the nursing assistant to stay with the client while obtaining 15 to 30 g of a carbohydrate snack for the client to eat.