could stem cells treat blindness from macular degeneration?
advertisement
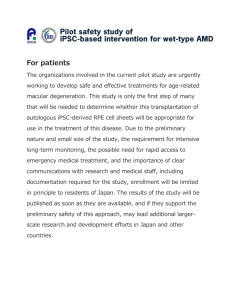
FEDERATION OF EUROPEAN NEUROSCIENCE SOCIETIES 9th FENS Forum of Neuroscience 5-9 July 2014 – Milan, Italy http://fens2014.neurosciences.asso.fr/ PRESS RELEASE EMBARGOED UNTIL TUESDAY 8 JULY 2014, 11:15 CEST / 10:15 BST COULD STEM CELLS TREAT BLINDNESS FROM MACULAR DEGENERATION? New ways of using stem cells to treat a common form of blindness have been developed in mice by scientists in California. A combination of a new surgical technique and stem cells that turn into specific cells in the eye’s retina could offer hope for millions of people with age-related macular degeneration (AMD), delegates heard today (8 July). Mark Humayun, Professor of Ophthalmology, Cell and Neurobiology, and Biomedical Engineering at the University of Southern California, and Keck School of Medicine of USC and USC Viterbi School of Engineering, USA leads the California Project to Cure Blindness. The goal of the research is to replace damaged retinal pigment epithelial (RPE) cells. “We believe that replacing dead or dying RPE cells in AMD could be a way to slow the disease process and even improve vision,” he said at FENS, Europe’s largest neuroscience conference, in Milan. AMD is a devastating disease that can lead to severe vision impairment — a loss of central, sharp vision with colour — and blindness. It occurs mostly in people over the age of 55. This treatment aims to replace dysfunctional RPE cells with fresh RPE cells. “Because of the relatively difficult nature of the surgical procedure and limited healthy RPE cells, transplanting a person’s own cells is challenging, so we rely on human embryonic stem cells,” Professor Humayun said. Stem cells have the potential to become any type of cell. They are cultured in the laboratory before they are implanted, enabling them to mature into a highly pure source of functional RPE cells. Reporting on a year’s progress made in his research to restore vision, Professor Humayun outlined four major themes. Firstly, a specific stem cell line has been identified that contains the characteristics of normal adult RPE cells. Second, a material has been found that can act as a platform that will support the RPE cells and allow them to function in a normal manner. Third, they have begun to demonstrate the safety of the procedure as well as its efficacy in slowing vision loss in rodents. Fourth, they have developed unique surgical techniques that will allow them to place the stem cells in animals’ eyes, and ultimately in people’s eyes. “In parallel to these laboratory studies, we are working towards trials to treat human patients with AMD. Already, results from more than six months of animal studies have demonstrated the safety of the technique, as well as its ability to restore vision. We envision that eventually this will lead us to a successful human clinical trial for those with currently untreatable AMD,” he said. END Abstract Reference R10023: Cell replacement therapy for retinal pigment epithelium diseases Symposia S38: Cell and gene therapy approaches in retinal degenerations Contact FENS Press Office and all media enquiries: Elaine Snell, Snell Communications Ltd, London UK (English language) tel: +44 (0)20 7738 0424 or mobile +44 (0)7973 953 794 email: Elaine@snell-communications.net Mauro Scanu (Italian language) tel: +39 333 161 5477 email: press.office@fens.org Professor Mark Humayun humayun@usc.edu NOTES TO EDITORS The 9th FENS Forum of Neuroscience, the largest basic neuroscience meeting in Europe, organised by FENS and hosted by the The Società Italiana di Neuroscienze (SINS) (Italian Society for Neuroscience) will attract an estimated 5,500 international delegates. The Federation of European Neuroscience Societies (FENS), founded in 1998, aims to advance research and education in neuroscience, representing neuroscience research in the European Commission and other granting bodies. FENS represents 42 national and mono-disciplinary neuroscience societies with close to 23,000 member scientists from 32 European countries. http://fens2014.neurosciences.asso.fr/ Further Reading (Humayun) Microdevice-based cell therapy for age-related macular degeneration. B Lu, YC Tai, MS Humayun. Developments in Ophthalmology. 2014; Epub April 2014; 53: 155-66. DOI: 10.1159/000357375 In vivo detection of hESC-RPE cells via confocal near-infrared fundus reflectance. RM Ribeiro, A Oregon, B Diniz , RB Fernandes, MJ Koss, W Charafeddin, Y Hu, P Thomas, BB Thomas, M Maia, GJ Chader, DR Hinton, MS Humayun. Ophthalmic Surgery, Lasers & Imaging Retina. JulyAugust 2013; 44(4): 380-4. DOI: 10.3928/23258160-20130715-09 Subretinal implantation of retinal pigment epithelial cells derived from human embryonic stem cells: improved survival when implanted as a monolayer. B Diniz, P Thomas, BB Thomas, R Ribeiro, Y Hu, R Brant, A Ahuja, D Zhu, L Liu, M Koss, M Maia, G Chader, DR Hinton, MS Humayun. Investigative Ophthalmology and Visual Science. July 2013; 26;54(7): 5087-96. DOI: 10.1167/iovs.12-11239 A novel approach for subretinal implantation of ultrathin substrates containing stem cell-derived retinal pigment epithelium monolayer. Y Hu, L Liu, B Lu, D Zhu, R Ribeiro, B Diniz, PB Thomas, A Ahuja, DR Hinton, YC Tai, ST Hikita, LV Johnson, DO Clegg, BB Thomas, MS Humayun. Ophthalmic Research. 2012; Epub August 2012; 48(4): 186-91. DOI: 10.1159/000338749