lecture1
advertisement

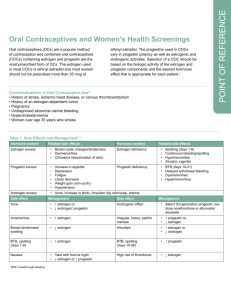
Lectures Lecture 1: Hormonal contraception HORMONAL CONTRACEPTIVE METHODS Hormonal contraceptives are the most commonly used reversible means of preventing pregnancy in the United States and consist of combined (estrogen and progesterone) and progesterone-only methods. Currently, combined hormonal methods are available in oral, transdermal, and vaginal forms, whereas progesterone-only methods are available in oral, injectable, implantable, and intrauterine forms. At this time, there are several hormonal contraceptives in various stages of the FDA approval process in the United States including new formulations for oral use, new subdermal implants and vaginal delivery systems, self-injectables, and male hormonal methods. COMBINED ESTROGEN AND PROGESTIN METHODS Oral Contraceptive Pills (OCPs) Method of Action Oral contraceptive pills (OCPs) are composed of progesterone alone or a combination of progesterone and estrogen. (The progesterone-alone pill is described later in the progesterone-only section.) Over 150 million women worldwide—including one-third of sexually active women in the United States—use oral contraceptives. Figure 24-9 • Serum levels of FSH and LH during a normal menstrual cycle. Figure 24-10 • Serum levels of FSH and LH while taking monophasic oral contraceptive pills. Oral contraceptives place the body in a pseudo-pregnancy state by interfering with the pulsatile release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary. This pseudopregnancy state suppresses ovulation and prevents pregnancy from occurring. Figure 24-9 illustrates the serum levels of FSH and LH during the normal menstrual cycle, and Figure 24-10 shows FSH and LH levels during a cycle on the combination pill. Because the FSH and LH surges do not occur, follicle growth, recruitment, and ovulation do not occur. The bleeding that takes place during the hormone-free interval is actually a bleed due to the withdrawal of hormone rather than a menstrual period induced by endogenous hormone fluctuation. Secondary mechanisms of action for OCPs include thickening the cervical mucus to render it less penetrable by sperm and changing the endometrium to make it unsuitable for implantation. Monophasic (Fixed-Dose) Combination Pills Monophasic combination pills contain a fixed dose of estrogen and a fixed dose of progestin in each tablet. Nearly 30 combinations of estrogen and progestins are available in the United States. In general, the selection of a particular pill for each patient depends on the individual side effects and risk factors for each patient. The combination pill containing both estrogen and progestin is taken for the first 21 days out of a 28-day monthly cycle. During the last 7 days of the cycle, a placebo pill or no pill is taken. Bleeding should begin within 3 to 5 days of completion of the 21 days of hormones. Newer formulations are now available that give 24 days of hormone (rather than the traditional 21 days) and a 4-day hormone-free interval. So-called 24/4 regimens (i.e., Yaz and Loestrin 24 Fe) result in a shorter 3- to 4-day menstrual cycle for most users. Multiphasic (Dose Varying) Combination Pills Multiphasic oral contraceptives differ from monophasic pills only in that they vary the dosage of estrogen and/or progestin in the active hormone pills in an effort to mimic the menstrual cycle. The advantage of the multiphasic dosing is that it may provide a lower level of estrogen and progestin overall but is still highly effective at preventing pregnancy. TABLE 24-3 Interactions of Oral Contraceptives with Other Medications That Reduce the Efficacy of Oral Contraceptives Medications Whose Efficacies are Changed by Oral Contraceptives Barbiturates Chlordiazepoxide (Librium) Carbamazepine (Tegretol) Diazepam (Valium) Griseofulvin Hypoglycemics Phenytoin (Dilantin) Methyldopa Rifampin Phenothiazides St. John's wort Theophylline Topiramate (Topamax) Tricyclic antidepressants TABLE 24-4 Complications Associated with Oral Contraceptives Cardiovascular* Deep vein thrombosis (DVT) Pulmonary embolism (PE) Cerebrovascular accident (CVA)** Myocardial infarction (MI)** Hypertension Other Cholelithiasis Cholecystitis Benign liver adenomas (rare) Cervical adenocarcinoma (rare) Retinal thrombosis (rare) * These complications occur mainly in smokers. ** Most MIs and CVAs occur in users of high-dose estrogen products. Effectiveness OCPs are remarkably effective in preventing pregnancy. In fact, the theoretical failure rate for the first year of use is less than 1%. However, the failure rate with actual real-life usage is closer to 8%. Nausea, breakthrough bleeding, and the necessity of taking the pill every day are often cited as reasons for discontinuing the pill. Several medications are thought to interact with oral contraceptives and reduce the effectiveness of the pill. Conversely, oral contraceptives can also reduce the efficacy of many medications (Table 24-3). Side Effects stroke, DVT, and PE if they use OCPs. The progestins in oral contraceptives have been found to raise low-density lipoproteins while lowering high-density lipoproteins in pill users smoking more than 1 pack per day. For these reasons, oral contraceptives are contraindicated in women over age 35 who smoke 15 or more cigarettes a day. The advent of new progestins and lower estrogen doses has led to pill formulations that are essentially neutral in terms of cardiovascular effect. However, combination oral contraceptive use is still contraindicated in women over age 35 who smoke. These women often benefit from progesterone-only IUDs or permanent female or male sterilization. Neoplastic complications of oral contraceptive use are rare. The effect of long-term oral contraceptive use on breast cancer has been studied extensively over the past decade Table 24-4 lists some of the cardiovascular, neoplastic, and biliary complications associated with oral contraceptive use.Oral contraceptives with estrogen doses greater than 50 mg can increase coagulability, leading to higher rates of myocardial infarction, stroke, thromboembolism, and pulmonary embolism, particularly in women who smoke. Even at lower doses of estrogen (35 mcg or less), women over 35 who smoke more than one pack of cigarettes per day are still at increased risk of heart attackwith no conclusive findings. There is, however, an increased incidence of gallbladder disease and benign hepatic tumors associated with oral contraceptive use. Table 24-5 outlines both the absolute and relative contraindications to oral contraceptive use. TABLE 24-5 Contraindications to Combination Estrogen-Progesterone Contraceptives Absolute Contraindications Thromboembolism Pulmonary embolism Coronary artery disease Cerebrovascular accident Smokers over the age of 35 Breast/endometrial cancer Unexplained vaginal bleeding Abnormal liver function disease Known or suspected pregnancy Severe hypercholesterolemia Severe hypertriglyceridemia Relative Contraindications Uterine fibroids Lactation Diabetes mellitus Sickle-cell disease or sickle C disease Hepatic disease Hypertension Lupus (SLE) Age 40+ and high risk for vascular Migraine headaches Seizure disorders Elective surgery TABLE 24-6 Noncontraceptive Health Benefits of Oral Contraceptives Decrease risk of serious diseases Ovarian cancer Endometrial cancer Ectopic pregnancy (combination pills only) Severe anemia Pelvic inflammatory disease Salpingitis Improve quality-of-life problems Iron-deficiency anemia Dysmenorrhea Functional ovarian cysts Benign breast disease Osteoporosis (increased bone density) Rheumatoid arthritis Treat/manage many disorders Dysfunctional uterine bleeding Control of bleeding in bleeding disorders and anovulation Dysmenorrhea Endometriosis Acne/hirsutism Premenstrual syndrome Advantages/Disadvantages The major advantages of OCPs include their extremely high efficacy rates and the noncontraceptive health benefits primarily attributable to decreased pregnancy, decreased menstrual flow, and decreased ovulation. These benefits include a reduced incidence of ovarian cancer, endometrial cancer, ectopic pregnancy, pelvic inflammatory disease (PID), and benign breast disease (Table 24-6). By taking OCPs, nearly 50,000 women avoid hospitalizations; of these, 10,000 avoid hospitalization for life-threatening illnesses. Disadvantages include cardiovascular complications, increased gallbladder disease, increased incidence of benign hepatic tumors, and the need to take a medication every day Because they contain estrogen, combination OCPs are not suitable for many women. Many women also complain of nausea, headaches, breakthrough bleeding, and weight gain associated with OCP use. Most of these symptoms are generally mild and transient. Transdermal Estrogen and Progestin Hormonal Contraception—Ortho Evr \ Mechanism of Action The contraceptive patch (Fig. 24-11) with the brand name Ortho Evra releases progestin and ethinyl estradiol. The patch releases 150 mg per day of the progestin, norelgestromin, and 20 μg per day of ethinyl estradiol. Although it is difficult to compare the estrogen levels in Ortho Evra users to those in women taking standard OCPs, limited data suggests that the overall average estrogen concentration is higher in Ortho Evra users. Therefore, these patients should be made aware of the possible increased risk of thromboembolism, specifically DVT and PE in Ortho Evra users. There does not appear to be an increased risk of heart attack and stroke in these patients. Women apply one patch each week for 3 weeks followed by 1 week patchfree during which they will have a withdrawal bleed. Effectiveness The patch has been shown to have a 1% pregnancy rate in actual use— similar to other combination hormonal methods. Ortho Evra has been found to have a decreased effectiveness in markedly overweight women (greater than 198 pounds or 90 kg). Advantages/Disadvantages The same primary side effects and noncontraceptive health benefits of OCPs apply to the patch as well. The patch can cause skin irritation in some users. The patch has the added benefit of being self-administered only once a week. Vaginal Estrogen and Progestin Hormonal Contraception-NuvaRing Method of Action The hormone-releasing vaginal ring (Fig. 24-11) with the brand name of NuvaRing releases a daily dose of 15 mcg of ethinyl estradiol and 120 mcg of etonogestrel (the active form of desogestrel). The ring is placed in the vagina for 3 weeks (it is likely effective for 4 weeks), and is removed for 1 week to allow for a withdrawal bleed. Again, this hormone-free period can be skipped to allow for continuous dosing, typically for 3 months. Effectiveness Clinical studies are ongoing, but the vaginal ring is highly effective (0.8% failure rate in actual use), similar to other forms of combined hormonal contraception. Advantages/Disadvantages Because one size of vaginal ring fits all women, the vaginal ring need does not need to be fitted by a clinician. Women place the ring in the vagina themselves for 3 continuous weeks and then remove it for 1 week. Because the ring is left in place continuously it provides a low, steady release of hormone with lower total hormone exposure compared to other combination hormone methods. And, while douching with the NuvaRing in place is discouraged, the use of antifungal agents and spermicides is permitted. PROGESTERONE-ONLY CONTRACEPTION Progesterone-only contraception consists of oral, injectable, implantable, and intrauterine options. These all function primarily using the same mechanisms: thickening the cervical mucus, inhibiting sperm motility, and thinning the endometrial lining so that it is not suitable for implantation. Progestin-Only Oral Contraception Pills (The Minipill) Method of Action Progestin-only pills (POPs; Micronor, Nor-QD) deliver a small daily dose of progestin (0.35 mg norethindrone) without any estrogen. POPs have lower progestin doses than combination pills, thus the nickname minipills. POPs also differ from traditional pills in that they are taken every day of the cycle with no hormone-free days. POPs are believed to thicken the cervical mucus making it less permeable to sperm. This effect, however, decreases after 22 hours so the minipill must be taken at the same time each day. Other mechanisms of action include endometrial atrophy and ovulation suppression (50% of cycles). Effectiveness Progestin-only pills are generally not as effective (failure rate of 8%) as combination hormone regimens. This failure rate increases if punctual dosing is not achieved. Side Effects Side effects of the progesterone-only OCP include irregular ovulatory cycles, breakthrough bleeding, increased formation of follicular cysts, and acne. POPs can also cause breast tenderness and irritability. Advantages/Disadvantages Because they contain no estrogen, progestin-only pills are ideal for nursing mothers and women for whom estrogens are contraindicated including women over 35 who smoke and women with hypertension, CAD, CVD, lupus, migraines, and those with a personal history of thromboembolism. The disadvantages include irregular menses ranging from amenorrhea to irregular spotting. Also, POPs must be taken at the same time each day. A delay of more than 3 hours is akin to a missed pill. Injectable Progesterone-Only Contraception—Depo-Provera Method of Action Although it was only approved for contraceptive use in the United States in 1992, Depo-Provera (medroxyprogesterone acetate; DMPA) has been used in other countries since the mid-1960s. Depo-Provera is injected intramuscularly every 3 months in a vehicle that allows the slow release of progestin over a 3-month period. Depo-Provera acts by suppressing ovulation, thickening the cervical mucus, and making the endometrium unsuitable for implantation. After an injection, ovulation does not occur for 14 weeks; therefore, patients have a 2-week grace period in their every 12week dosing. Effectiveness With a first-year failure rate of only 0.3% when used correctly, DepoProvera is one of the most effective contraceptive methods available. A newer low-dose DMPA is also available although not widely used yet. This formulation carries the benefit of lower progestin levels but the same efficacy rates. Side Effects The primary side effects experienced by Depo-Provera users include irregular menstrual bleeding, depression, weight gain, hair loss, and headache. Over 70% of patients experience spotting and irregular menses during the first year of use. Irregular bleeding is the primary reason for discontinuing Depo-Provera. It is anticipated that 50% of DMPA users will have amenorrhea after 1 year of use and 80% after 5 years of DMPA use. However, the possibility of amenorrhea makes Depo-Provera a good option for women with bleeding disorders, women on anticoagulation, women in the military, and women who are mentally or physically disabled. Women using DMPA for more than 2 years may experience a reversible decrease in bone mineralization similar to that seen in lactating women. Advantages/Disadvantages The primary advantages of Depo-Provera are that it is highly effective, acts independent of intercourse, and only requires injections every 3 months. Like other progestins, Depo-Provera reduces the risk of endometrial cancer and PID and also the amount of menstrual bleeding. It is also useful in the treatment of menorrhagia, dysmenorrhea, endometriosis, menstrualrelated anemia, and endometrial hyperplasia. DMPA is especially useful in women who desire effective contraception but may have concomitant medical conditions that prevent the use of estrogen-containing contraceptives such as women with migraines, seizure disorders, lupus, hypertension, coronary artery disease, and who smoke. TABLE 24-7 The Effects of Depo-Provera Use on Bone Mineralization Bone density is decreased in women using Depo-Provera The decrease in bone density is most rapid in the first year of use The decrease in bone density increases with length of use The decrease in bone density is reversible and occurs over 6 mo to 2 years There is no role for the use of bone density screening (DEXA) in DMPA users There is no role for the use of bisphosphonates, estrogens, SERMS in DMPA users Women on Depo-Provera should be encouraged to take calcium and vitamin D, to stop smoking, and to do regular weight-bearing exercise Irregular bleeding, weight gain, and mood changes are the major disadvantages. Although not con-traindicated, Depo-Provera should be used with caution in patients with a history of depression, mood disorders, PMS, and PMDD. Similarly, Depo- Provera use is not contraindicated in obese women but weight monitoring should be employed when using the medicine in women who may be at increased risk for weight gain. Implantable Progesterone-Only Contraception—Implanon Method of Action Implanon is a single-rod, progestin implant that provides 3 years of uninterrupted contraceptive coverage. The progestin used in Implanon is etonogestrel, the same progestin as used in the NuvaRing. The device provides slow release of 68 mg of etonogestrel over 3 years. It is the size of a matchstick and is placed in the subdermal skin of a woman's upper arm. When appropriate timing of placement is utilized, Implanon is affective 24 hours after placement and has quick return to fertility once the device is removed by a clinician. Effectiveness Implanon is highly effective with only a 0.4% failure rate. Side Effects Irregular and unpredictable light bleeding is the major side effect of Implanon. In the majority of cases (75%), the bleeding is lighter than a normal menstrual bleed and requires only a panty liner or less for protection. However, irregular bleeding was the reason for 20% of discontinuations. Advantages/Disadvantages The major advantage of Implanon is that it is implantable and provides 3 uninterrupted years of contraceptive coverage. There is no maintenance associated with the device and thus no interruption of sexual spontaneity. The disadvantages include the need for a provider to insert and remove the device and the unpredictable bleeding profile.