Supplementary Table 1 Selected demography, comorbid medical
advertisement

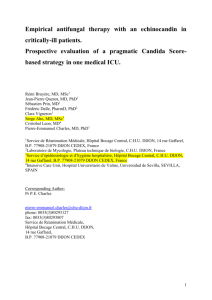
Supplementary Table 1 Selected demography, comorbid medical, surgical and therapeutic risk factors and outcome of adult candidemia patients admitted to 27 intensive care units across India from April 2011 to September 2012 Characteristic Candidemi Characteristic Candidem a cases ia cases (n=913) (n=913) Demography Therapeutic risk factors Age (years) (median; 50.0 (34- interquartile range) 63) Males (%) 534 (58.5) Steroid therapy (%) 164 (18.0) Broad spectrum antibiotics 784 (85.9) (%) Females (%) 379 (41.5) Received antibiotics (%) 849 (93.0) Public sector (%) 377 (41.3) 1 antibiotic (%) 265 (29.0) Private/corporate sector (%) 536 (58.7) 2 antibiotics (%) 298 (32.6) 3 antibiotics (%) 173 (18.9) 228 (25.0) 4 antibiotics (%) 73 (8.0) 209 (22.9) 5 antibiotics (%) 30 (3.3) Comorbid medical conditions Underlying respiratory disease (%) Underlying renal diseasea (%) Renal failureb (%) 191 (20.9) Underlying neurological 178 (19.5) Cytotoxic chemotherapy (%) 20 (2.2) 138 (15.1) Immunomodulator therapy 6 (0.7) 6 antibiotics (%) 10 (1.1) disease (%) Underlying CVD (%) (%) Underlying malignancy (%) 117 (12.8) Antifungal exposure before ICU admission Underlying liver disease (%) 99 (10.8) Prior antifungals (%) 143 (15.7) Underlying GIT disease (%) 65 (7.1) Days on prior antifungals 8.0 (5-13) Liver (%) 99 (10.8 Pancreatitis (%) 62 (6.8) Prior amphotericin B (%) 7/143 (4.9) Neutropenia (%) 12 (1.3) Days on prior amphotericin B 9.0 (3-19) (median; interquartile range) (median; interquartile range) Transplant (%) 12 (1.3) Prior anidulafungin (%) 4/143 (2.8) HIV/AIDS (%) 4 (0.4) Prior caspofungin (%) 11/143 (7.7) Surgical procedures Prior echinocandins (%) 15/143 (10.5) Any surgery (%) 341 (37.3) Days on prior echinocandins 11.0 (5-13) (median; interquartile range) GI surgery (%) 142 (15.6) Prior fluconazole (%) 112/143 (78.3) General surgery (%) 53 (5.8) Prior posaconazole (%) 1/143 (0.7) Neurosurgery (%) 45 (4.9) Prior voriconazole (%) 12/143 (8.4) Vascular surgery (%) 42 (4.6) Prior azoles (%) 125/143 (87.4) Genitourinary surgery (%) 25 (2.7) Days on prior azoles (median; 7.0 (5-13) interquartile range) Orthopedic surgery (%) 19 (2.1) Reasons for prior antifungals Pancreatic surgery (%) 14 (1.5) Prophylactic antifungals (%) 30/143 (20.9) Obstetric surgery (%) 11 (1.2) Empiric antifungals (%) 69/143 (48.3) Hepatobiliary surgery (%) 9 (1.0) Treatment after diagnosis (%) 11/143 (7.7) Invasive procedures Not mentioned (%) 33/143 (23.1) Central venous catheterization 676 (74.0) Outcome (%) CVC removed after 217/676 Length of stay in ICU 17.0 (10- candidemia (%) (32.1) (median;interquartile range) 33) Removed in <24 hours 59/217 Days to candidemia (median; 8.0 (4-15) (%) (27.2) interquartile range) Removed in 24-48 hours 59/217 Resolved (%) 251 (27.5) (%) (27.2) Removed after >48 hours 99/217 Discharged (%) 390 (42.7) (%) (45.6) 483 (45.6) Still admitted (%) 49 (5.4) Total parenteral nutrition (%) 122 (13.4) LAMA (%) 51 (5.6) Dialysis before (%) 185 (20.3) 30-day crude mortality (%) 408 (44.7) Urinary catheter (%) 693 (75.9) 30-day attributable mortality 179 (19.6) Invasive mechanical ventilation (%) (%) Drainage catheter(s) (%) 271 (29.7) Abnormal chest X-ray (%) 58 (6.4) APACHE - Median; (range) 17.0 (0-39) SD = standard deviation, APACHE II = Acute Physiology and Chronic Health Evaluation II, MODS = multi-organ dysfunction syndrome, CVD = cardiovascular disease, GIT = gastrointestinal tract, CVC = central venous catheter, LAMA = left against medical advice, a Underlying renal disease was considered when the case had renal disease without going to failure. Under the underlying disease other than renal failure the conditions include diabetic nephropathy, glomerulonephritis, heptato renal syndrome, hydronephorosis, pyelonephrosis, renal calculi, and haemolytic ureamic syndrome. b Acute renal failure (ARF) was defined as a abrupt loss of kidney function with measurable increase in the serum creatinine concentration (usually relative increase of 50% or absolute increase of 0.5 to 1.0 mg/dL). Chronic renal failure/kidney disease was defined when there was loss of kidney function over months or years. Supplementary Text: Underlying diseases and risk factors: Gastrointestinal conditions included illnesses of the gastrointestinal tract (65; 7.1%), liver (99; 10.8%) and pancreatitis (62; 6.8%). Neutropenia (12; 1.3%) and HIV/AIDS (4; 0.4%) were uncommon (Supplementary Table 1). Antibiotic exposure: The predominant antibiotic exposure was to carbapenems (393; 43.0%) followed by penicillins (289; 31.7%), cephalosporins (222; 24.3%), glycopeptides (209; 22.9%), aminoglycosides (139; 15.2%), quinolones (117; 12.8%) and polymyxins (108; 11.8%). Break through candidemia: A total of 64 patients had overlapping periods of previous antifungals with current ICU admission for at least 4 days. Of these only 13 were on prophylactic treatment and the rest were on empiric treatment. C. tropicalis was seen in 6, C. albicans in 4, and C. glabrata in 3. Of these 6 died and 7 were alive at 30 days after onset. Supplementary Table 2 Antifungal treatment received by adult candidemia intensive care patients after definitive microbiological diagnosis in the ICU Characteristic Candidemi Characteristic Candidemi a cases a cases (n=913) (n=913) Treatment after diagnosis in Change in treatment ICU Antifungal treatment (%) 547 (59.9) Antifungal changed (%) 81/547 (14.8) Days on antifungals (median; 9.0 (5-15) AFST (%) 17/81 (20.9) 72/547 Cost (%) 3/81 (3.7) 8.0 (5-12) De-escalation (%) 13/81 (16.0) Liposomal amphotericin B (%) 7/547 (1.3) No reason (%) 4/81 (4.9) Anidulafungin (%) 22/547 Switch to oral (%) 1/81 (1.2) interquartile range) Amphotericin B (%) (13.2) Days on amphotericin B (median; interquartile range) (4.0) Caspofungin (%) 72/547 Toxicity (%) 7/81 (8.6) 36/81 (44.4) (13.2) Micafungin (%) 7/547 (1.3) Escalation (%) Echinocandins (%) 100/547 Adverse reactions (18.3) Days on echinocandins 6.0 (3.75- (median; range) 14) Fluconazole (%) 359/547 Acute renal failure (%) 5/547 (0.9) Bradycardia (%) 1/547 (0.2) Hypokalemia (%) 2/547 (0.4) (65.6) Posaconazole (%) 1/547 (0.2) Voriconazole (%) 40/547 (7.3) Azoles (%) 394/547 (72.0) Days on azoles (median; range) 10.0 (5-15) SD standard deviation, AFST antifungal susceptibility test. Supplementary Table 3 Candidemia risk factors significantly associated with 30-day crude mortality of adult candidemia intensive care patients Risk factor 30-day crude mortality Survived (n=505) Died (n=408) p Age (mean ± SD) 48.4 ± 17.4 51.3 ± 18.0 0.014 Public sector hospital (%) 188 (37.2) 189 (46.3) 0.006 APACHE II (mean ± SD) 15.6 ± 5.5 18.7 ± 5.7 <0.001 Length of ICU stay (mean ± SD) 28.7 ± 25.4 17.9 ± 14.9 <0.001 Presentation with sepsis (%) 48 (9.5) 64 (15.7) 0.006 Presentation with shock (%) 13 (2.6) 24 (5.9) 0.017 Presentation with MODS (%) 8 (1.6) 17 (4.2) 0.023 Underlying liver disease (%) 43 (8.5) 56 (13.7) 0.014 Underlying respiratory disease (%) 102 (20.2) 126 (30.9) <0.001 Underlying renal disease (%) 89 (17.6) 120 (29.4) <0.001 Acute renal failure (%) 54 (10.7) 74 (18.1) 0.002 Chronic renal failure (%) 25 (5.0) 38 (9.3) 0.012 Renal failure (%) 79 (15.6) 112 (27.5) <0.001 Neutrophil count (day 30) (mean ± SD) 5655.5 ± 2845.9 6761.0 ± 5621.6 0.012 Serum creatinine (day 30) (mean ± SD) 1.3 ± 1.1 2.3 ± 1.8 <0.001 Dialysis (%) 76 (15.0) 109 (26.7) <0.001 Hemodialysis (%) 67 (13.3) 91 (22.3) <0.001 Peritoneal dialysis (%) 7 (1.4) 23 (5.6) 0.001 Invasive mechanical ventilation (%) 240 (55.2) 243 (68.6) <0.001 Corticosteroid therapy (%) 67 (13.3) 97 (23.8) <0.001 Colistin therapy (%) 37 (7.3) 57 (14.0) 0.001 Clindamycin therapy (%) 5 (1.0) 22 (5.4) <0.001 Polymyxin(s) therapya (%) 47 (9.3) 61 (15.0) 0.010 Secondary bacterial infection (%) 48 (9.5) 62 (15.2) 0.010 Acinetobacter spp. sepsis (%) 10 (2.0) 20 (4.9) 0.015 GNB infection (%) 39 (7.7) 55 (13.5) 0.006 338 (66.9) 209 (51.2) <0.001 7.9 ± 9.4 3.8 ± 6.1 <0.001 257 (50.9) 137 (33.6) <0.001 Days on azolesb (mean ± SD) 5.7 ± 8.3 2.6 ± 5.6 <0.001 Abnormal chest X-rayc (%) 22 (4.4) 36 (8.8) 0.006 Antifungal treatment (%) Days on antifungalsb (mean ± SD) Treatment with azoles (%) SD standard deviation, APACHE II Acute Physiology and Chronic Health Evaluation II, MODS multi-organ dysfunction syndrome, GNB gram negative bacteria. a Polymyxin(s) refer to any exposure to colistin and/or polymyxin B. b c Therapy instituted after definitive microbiological diagnosis of candidemia in the ICU. An abnormal chest X-ray includes, abnormal opacities, consolidation, effusions and pneumothorax. Legend Supplementary Fig. 1 Percentage of various Candida species isolated from 918 adult candidemia intensive care patients highlighting the eight species contributing the highest burden. "Others" comprise 22 less common Candida species found in our patients