What are causes of autism? - Contemporary Practices in Early
advertisement

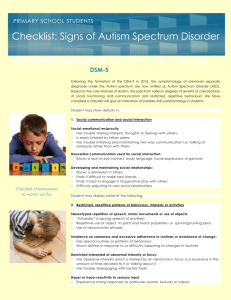
Autism Spectrum Disorders What is an autism spectrum disorder (ASD)? Autism spectrum disorders include Autistic Disorder (AD), Asperger syndrome (AS), and Pervasive Developmental Disorder- Not Otherwise Specified (PDD- NOS). These are neurodevelopment disorders characterized by deficits in social interaction, communication, and repetitive or unusual intense behaviors or interests. The diagnosis is made based on medical and developmental evaluations and the criteria in the Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. The diagnosis of autism can be made as early as 18 months of age but is more often diagnosed in children around three years of age. The characteristics of autism vary in intensity but delays in the acquisition of developmental skills and atypical patterns of development are seen in all children with autism. The Individuals with Disabilities Education Act (IDEA) defines the disorder as “a developmental disability significantly affecting verbal and nonverbal communication and social interaction, generally evident before age 3, which adversely affects a child’s educational performance. Other characteristics often associated with autism are engagement in repetitive activities and stereotyped movements, resistance to environmental change or change in daily routines, and unusual responses to sensory experiences.” [See 34 Code of Federal Regulations §300.8(c)(1).] Associated Disorders There are other disorders that are often confused with or accompany autism spectrum disorders. These include: intellectual disability, Rett syndrome, childhood disintegrative disorder, fragile X syndrome, tuberous sclerosis, phenylketonuria, fetal alcohol spectrum disorder, Angelman syndrome, Smith-Lenli-Opitz syndrome, CHARGE syndrome, Down syndrome and schizophrenia. It is important to determine during the diagnostic process if these associated disorders are present. Children with ASD may also have seizures, intellectual disabilities, learning disabilities, gastrointestinal disorders, sensory processing disorders, attention deficit hyperactivity disorder, and sleep disturbances. www.teachingei.org p. 1 How many children have autism? There currently is not an accurate estimate of the number of people with ASD in the United States and controversy exists over how we diagnose and categorize who has an autism spectrum disorder (ASD). However, the Center for Disease Control and Prevention estimated that in 2007 about 1 in 150 8 year old children had an ASD based on data gathered from government surveys of selected community, health, and medical records through the Autism and Developmental Disabilities Monitoring Network project. Estimates of the prevalence also vary by region and it is difficult to determine if the overall prevalence rate is increasing, decreasing or remaining the same. The prevalence rate is for higher for boys than girls and ASDs are more common than Down syndrome (1 in 800) and childhood cancers (1.5 in 10,000). For more information about the prevalence rate of ASDs, see the Center for Disease Control and Prevention, Autism Information Center at http://www.cdc.gov/ncbddd/autism/index.html Description of Autism Spectrum Disorders Currently, there is no one medical test to determine if a child has ASD and the etiology of autism is unknown. The diagnosis is made through a combination of observations, parent, caregiver and educator interviews, and meeting a threshold of criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). Autistic spectrum disorder is diagnosed when a child meets a total of six or more of the criteria in the areas of qualitative social impairment (at least two of these criteria), qualitative communication impairments (at least one) and restricted, repetitive, and stereotyped patterns of behavior, interests, and activities (at least one) and manifests these delays by age three when Rett syndrome and child disintegrative disorder have been ruled out. The criteria for the diagnosis of Asperger syndrome are similar to ASD. Individuals with Asperger syndrome have qualitative impairments in social interactions and restricted, repetitive, and stereotyped patterns of behavior, interests, and activities with significant social skill and pragmatic language impairments but without delays in receptive and expressive language, cognitive or adaptive (self-help) skills. Schizophrenia must also be ruled out in order for Asperger syndrome to be diagnosed. Children with pervasive developmental disorder, not otherwise specified (PDD-NOS) also demonstrate atypical social interactions, delays in communication skills, and restrictive or intense behaviors or interests thus meeting many of the criteria to be diagnosed with ASD, but just below the threshold to make the diagnosis of ASD. For a detailed description of the criteria, see the Autism Information Center at the Center for Disease Control and Prevention http://www.cdc.gov/ncbddd/autism/hcp-dsm.html www.teachingei.org p. 2 Autism Spectrum Disorders Type Autistic Disorder Asperger Syndrome Pervasive Developmental Disorder, Not Otherwise Specified PDDNOS Characteristics Delays in social, communication, and adaptive skill development with repetitive, restrictive or intense patterns of behavior, interest and activities. Delays in social skills and pragmatic language, with repetitive, restrictive or intense patterns of behavior, interest and activities without delays in cognitive, adaptive, or language development. Delays in social, communication, and adaptive skill development with repetitive, restrictive or intense patterns of behavior, interest and activities but do not meet the threshold of criteria for a diagnosis of Autistic Disorder. What are causes of autism? The cause is still unknown. Children are at higher risk of having ASDs if there is a history of the disorder in the family, parents are of advanced maternal or paternal age, or there has been exposure in utero to environmental toxins. What are interventions used for individuals with autism? The goal of intervention is to promote participation in naturally occurring activities and routines. Intervention often focuses on social and communication skill development. There are a wide variety of behavioral, educational, medical, and communication interventions available to promote learning, social interaction, communication, and adaptive development for children with ASD. Not all of the interventions used have strong evidence to support their effectiveness. The chart below is a quick reference list of the more common interventions used with children with ASD divided into types and categories of “Established” Interventions; “Emerging” Interventions; and “Unestablished” Interventions based on research and the National Standards Report published by the National Autism Center in 2009. As defined by in the report, “Established” Interventions are those with sufficient evidence to confidently determine a treatment produces beneficial treatment effects. “Emerging” Interventions are those that have one or more studies suggesting a treatment will produce beneficial treatment effects but need further study on effectiveness. “Unestablished” interventions are those with little or no evidence to support their use. It is beyond the purpose of this document to describe each of these interventions in detail, a few are brief descriptions are included below. Refer to the National Autism Center reports and listed resources for more comprehensive information about any of these interventions. www.teachingei.org p. 3 Common Interventions for ASD Type Behavioral CommunicationBased Educational Established Emerging Applied Behavioral Analysis (ABA) Differential reinforcement Discrete Trial Teaching (DTT) Functional Communication Training (FCT) Task Analysis Token Economy Behavioral toilet training Behavior chain interruption Cueing and prompting Noncontingent reinforcement Self Management Schedules Cognitive Behavioral Interventions Naturalistic Teaching Strategies Pivotal Response Treatment (PRT) Story Based Unestablished Exposure-Based Interventions (ie: exposure to increasingly anxiety provoking situations; preventing maladaptive strategies) Alternative and Augmentative Communication (AAC) Language Production Training Echo relevant word training Structured discourse Picture Exchange Communication System (PECS) Sign Instruction Hannen® Method Total Communication Initiation Training Music Therapy Structured Teaching/ Treatment and Education of Autistic and related communication-handicapped children (TEACCH) www.teachingei.org p. 4 Auditory Integration Training Facilitated Communication Academic Interventions: The Expression Connection Picture to text matching Handwriting training Type Relationships-Based Established Emerging Joint Attention Based Modeling Peer Training Developmental Relationships-Based Treatment Denver Model Developmental, Individual Differences, Relationships-Based (DIR/Floortime) Relationship Development Intervention Imitation-Based Interactions Theory of Mind Training Social, Communication, Emotional Regulation, Tansactional Support (SCERTS™) Relationship Development Intervention (RDI) Exercise-Based Interventions Massage/Touch Therapy Alert Program Sensory Diet Sensory-Motor Pharmacological Unestablished Sensory-Integration Therapy Medications including anticonvulsants, antidepressants, stimulants, and antipsychotics have been used to improve attention and reduce anxiety, obsessivecompulsive behaviors, irritability, tantrums, self-injury and aggression in children with ASD. Defeat Autism Now (DAN) Protocol Gluten & Casein-Free Diet Omega 3 Fatty Acids Dietary www.teachingei.org p. 5 Brief Descriptions of Common Interventions Behavioral/Educational Applied Behavioral Analysis (ABA) Intensive programming (25-40 hours/week) One to one interaction Applies task analysis Strict behavior modification Discrete Trial Training, Lovass Method Treatment & Education of Autistic and Communication Handicapped Children (TEACCH) Classroom based program Strong parent training component Incorporates: Visual organization Behaviorally training Developmentally appropriate practices Relationship Based Developmental, Individual-Difference, Relationship Based (DIR) Builds on social communication Focuses on the relationship between child and parent Child directed play Builds shared attention Stresses engagement in the relationship Floortime Relationship Development Intervention (RDI) Addresses social learning Uses natural occurring activities and routines to shape language and social interactions Parents are primary facilitators Language Hanen Method Pragmatics Based on social-interactionist theory Emphasizes importance of contingent, simplified language Natural occurring activities and routines Families are primary facilitators Practical use of language Use of gestures, expression, proximity, inflection Uses social situations to rehearse appropriate communication Social Stories (Gray) www.teachingei.org p. 6 Alternative and Augmentative Communication (AAC) Low and high tech devices such as: Picture boards Picture Exchange Communication System (PECS) Signs Gestures Computers Synthesized speech Voice Output Communication Aids (VOCA) According to the National Academies of Science (http://www8.nationalacademies.org/onpinews/newsitem.aspx?RecordID=10017) intervention is most successful when: The child begins to receive intervention as early as possible, There is active engagement in intensive instructional programming for the equivalent of a full school day, including services that may be offered in different sites, Services are provided for a minimum of 5 days a week all year, Use of planned teaching opportunities, organized around relatively brief periods of time for the youngest children (e.g., 15- to 20-minute intervals), and Sufficient amounts of adult attention in one-to-one or small group instruction in order to meet individualized goals. Although there are differences in the philosophies that guide interventions, effective programs offer similar levels of intensity and organization, staffing, ongoing monitoring, and the use of discrete trials, incidental learning, and structured teaching periods embedded into the program. Tools used to help identify young children with ASD In addition to medical, educational, developmental assessments to determine skill performance and developmental skill acquisition there are several tools that have been developed specifically for children with autism: Autism Behavior Checklist (ABC) Autism Diagnostic Interview-Revised (ADI-R) Autism Diagnostic Observation Schedules (ADOS) Focus: social communication Checklist for Autism in Toddlers (CHAT) Focus: Development of attention and early communication Childhood Autism Rating Scales (CARS) Focus: Sensory motor behaviors Detection of Autism by Infant Sociability Interview (DAISI) Focus: Social engagement Gilliam Autism Rating scale (GARS) Focus: Behavior, communication, development, interaction Screening Tool for Autism in Two-Year Olds (STAT) Focus: Play, imitation, communication References Hyman, S. & Towbin, K.E. (2007). Autism spectrum disorders. In M.L. Batshaw , L. Pellegrino, & N. J. Roizen (Eds.), Children with Disabilities (6th ed.) (pp.325-344). Baltimore: Paul H. Brookes Publishing Company. Johnson, C.P., Myers, S.M., & the Council on Children with Disabilities (2007). Identification and evaluation of children with autism spectrum disorders. Pediatrics 120 (5), 1183-1215. www.teachingei.org p. 7 Greenspan, S.I., Brazelton,T. B., Cordero, J., Solomon, R., Bauman, M.L., Robinson, R., Shanker, S. & Breinbauer (2008). Guidelines for early identification, screening, and clinical management of children with autism spectrum disorders. Pediatrics 2008;121;828-830. Kelly, A.B., Garnett, M.S., Attwood, T. & Peterson,C. (2008). Autism spectrum symptomatology in children: The impact of the family and peer relationships. Journal of Abnormal Child Psychology. 38, 1069-1081. National Center for Health Statistics, Center of Disease Control and Prevention, U.S. Department of Human Services. Available at http://www.cdc.gov/nchs/ Resources Autism Society of America http://www.autism-society.org/ Autism Speaks http://www.autismspeaks.org/ Autism Speaks Family Services Kit http://www.autismspeaks.org/community/family_services/100_day_kit.php Association for Science in Autism Treatment http://www.asatonline.org Center for Disease Control and Prevention, Act Early http://www.cdc.gov/ncbddd/autism/actearly/default.htm Center for Disease Control and Prevention, Autism Information Center http://www.cdc.gov/ncbddd/autism/ Interdisciplinary Council on Developmental and Learning Disorders www.icdl.com MAAP Services for Autism, Asperger Syndrome, and PDD http://www.maapservices.org National Dissemination Center for Children with Disabilities http://www.nichcy.org National Institutes of Mental Health http://www.nimh.nih.gov/health/topics/autism-spectrum-disorders-pervasive-developmentaldisorders/index.shtml National Institute of Child Health and Human Development (NICHD) http://www.nichd.nih.gov www.teachingei.org p. 8 National Institute on Deafness and Other Communication Disorders Information Clearinghouse http://www.nidcd.nih.gov Committee on Educational Interventions for Children with Autism, National Research Council. (2001). Educating Children with Autism. Washington, DC: National Academies Press. http://www.nap.edu/openbook.php?isbn=0309072697&page=R5 Online Asperger Syndrome Information and Support http://www.udel.edu/bkirby/asperger/as_thru_years.html Professional Development Resources Autism Internet Modules http://www.autisminternetmodules.org/ Interactive Collaborative Autism Network (ICAN) Learning Modules http://www.autismnetwork.org/modules/index.html The National Professional Development Center on Autism Spectrum Disorders http://autismpdc.fpg.unc.edu/content/autism-internet-modules-aim The PDA Center: Professional Development in Autism http://depts.washington.edu/pdacent/courses/autism101.html# Cite As: Georgetown University Center for Child and Human Development. Contemporary Practices in Early Intervention: Autism Primer. 2011. Available online at http://www.teachingei.org. www.teachingei.org p. 9