Hematopoiesis Notes from Session 1 July 2015
advertisement

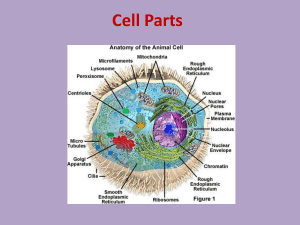
Hematopoiesis Blood Blood is the life sustaining “river” of the body. Blood provides the oxygen and nutrients necessary for life while removing waste from the tissues. It remains ever vigilant in fighting off invaders. It stops the bleeding when the body is injured. It defines who we are and distinguishes self from non-self. What is blood? Blood is a mixture of cellular and fluid elements. The fluid component of blood is called plasma. In total, the volume of blood averages about 70 mL/kg (or about 4.9 liters in a 70 kg adult). The cellular component of blood consists of three major types of cells each with distinct functions. 1. Red blood cells 2. White blood cells 3. Platelets Red blood cells’ major function is to transport oxygen to the tissues and remove carbon dioxide in exchange. This is achieved via a molecule in the red blood cell cytoplasm called hemoglobin. Hemoglobin consists of four globin proteins (typically, 2 -globin chains and 2 -globin chains in adult humans) each associated with heme (a protoporphyrin ring with iron). The red cell has a life span of approximately 100-120 days. The white blood cells comprise a heterogeneous group of cells that play a vital role in our immune system. They identify self from non-self and defend the body against invaders. These cells were discussed in detail during the immunology course. As you will recall, the white cells consist of two large categories of cells: the myeloid and lymphoid lineage cells. The myeloid lineage includes the neutrophils, monocytes, eosinophils, and basophils. The lymphoid lineage includes Blymphocytes, T-lymphocytes, and natural killer cells. Each plays a distinct role within the immune system. Platelets major function is to help stop bleeding at the site of vascular injury. The platelet has a life span of 7-10 days. Plasma is the fluid component of blood. The plasma is composed largely of water along with a variety of nutrients, electrolytes, and proteins. Some of the major proteins found in plasma include the following: albumin, lipoproteins, transport proteins, complement proteins, globulins (antibodies), and the coagulation system proteins. Where is Blood Made? Hematopoiesis is the process by which blood cells are produced and involves a complex balance of cellular proliferation, differentiation, morphogenesis, and functional maturation. This process must be sustained throughout life in order for life to be maintained. From where do the blood cells come? That answer varies during the course of human development. Hematopoiesis in utero is divided into overlapping phases as different organ systems are involved: Mesoblastic period (blood island of the yolk sac, 3-10 weeks gestation) Hepatic period (liver and spleen, 6 weeks – 7 months gestation) Myeloid period (bone marrow, 5 months gestation – birth and beyond) The bone marrow begins to produce blood cells during the third month and becomes the predominant site of hematopoiesis during the last two months of gestation and the only site of hematopoiesis by about three weeks postpartum. Throughout the remainder of life, hematopoiesis only occurs in the liver, spleen, and other sites if the bone marrow becomes diseased, a process termed extramedullary hematopoiesis. Active hematopoiesis takes place in all bones at birth, but is normally restricted to the centrally located flat bones (red marrow) (ribs, vertebrae, pelvis, sternum) after puberty. In contrast, adipose cells gradually fill the marrow spaces of the peripheral bones. Illustration by: Michal Komorniczak (Poland) Bone Marrow As you will hopefully recall from your anatomy and histology courses, bone consists of a thick outer (cortical) layer of dense (compact) bone, and an inner layer of sponge-like trabecular (cancellous, spongy) bone. A single layer of endosteal cells lines the inner cortex and honeycomb network of trabecular bone. In bones with red marrow, the cavities of the trabecular bone are filled with clusters of hematopoietic cells (stem cells and their progeny) and a vast network of vascular channels (marrow sinusoids). Fibroblastoid (reticular) cells cover the adventitial surface of the sinusoids and their cytoplasmic processes form a support lattice for hematopoietic cells. The fibroblastoid cells, vascular endothelial cells, macrophages, extracellular matrix molecules, adipocytes (fat cells), and other non-hematopoietic cells comprise the bone marrow stroma. In addition to providing an adhesive framework for the hematopoietic cells, the stromal cells produce many of the soluble chemical factors (hematopoietic cytokines) that regulate and control the process of hematopoiesis and the egress of mature blood cells from the bone marrow into the bloodstream. This regulatory mechanism assures that the normal production rate of blood cells is equal to the senescence rate, and that the production of hematopoietic cells can increase in response to disease states. The stromal cells, chemical substances, vessels, and other materials that support the hematopoietic cells are referred to collectively as the hematopoietic microenvironment. Hematopoietic Regulation Thus, there are four major processes of hematopoiesis 1. stem cell survival 2. self-renewal 3. proliferation 4. differentiation What steps must be undertaken when processing – controlling – managing hematopoiesis 1. cytokine, hormone, or CSF signaling 2. Binding of a surface receptor 3. Signal transduction pathways, which in the case of the major hematopoietic CSFs) which are all part of the same superfamily of receptors thus have much homology a. JAK-STAT pathways for proliferation b. MAPK pathway for differentiation and antiapoptosis to promote cell viability 4. Transcription factor networks 5. Translation a. microRNA 6. Post-translational modifications 7. Repeat (based on effect of the product generated) As such, every process of hematopoiesis (stem cell survival, self-renewal, proliferation, and differentiation) is orchestrated by a combination of growth factors, cytokines, microRNA, and transcription factors. Cytokines are hormone-like chemical signals (hematopoietic cytokines) within the "microenvironment" provided by the stromal cells and extracellular matrix of the bone marrow. Cytokines include the interleukins (IL), interferons (IFN), tumor necrosis factor (TNF). CSF and hormones are derived generally from external tissue and secreted more systemically. Colony stimulating factors include the likes of erythropoietin (EPO), thrombopoietin (Tpo), colony-stimulating factors for granulocytes (G- CSF) and granulocyte-macrophages (GM-CSF), among many others. The cytokine and colony stimulating factor composition of the microenvironment is dynamic in response to local and systemic factors/needs. Each cytokine and colony stimulating factor has its target(s), but the response to these factors is not hard fast. The response varies depending upon the other cytokines and CSFs present within the local microenvironment at that precise point in time; the surface receptor types and numbers present on the cell at that point in time; and the composition of intracellular microRNA and transcription factors present at that point in time. Some key factors are noted on the illustration below. The cellular membrane receptors for the major hematopoietic colony stimulating factors have been studied and many have been found to be closely related in structure (from a hematopoietic receptor superfamily). The receptors are themselves highly regulated with changing numbers during cell differentiation. The combination of a regulator with its membrane receptor leads to a structural change in the receptor, the triggering of a complex sequence of biochemical events (signal transduction). In the case of many of the major hematopoietic colony stimulating factors’ receptors, the signal pathways employ are both…. a. JAK-STAT pathways for proliferation b. MAPK pathway for differentiation and antiapoptosis to promote cell viability The generation of intracellular substances (signals) in the cytoplasm leads to the generation/recruitment/activation of transcription factors, which have the capacity to activate / repress genes that encode proteins influencing cell proliferation, differentiation, maturation, function and apoptosis (programmed cell death). The molecular events underlying hematopoiesis are incredibly complex and continue to be defined. But let’s stop for a moment to consider the processes by which genes are controlled… Transcriptional Regulatory Networks There are approximately 3 billion bp that make up the human genome and the approximately 20,000 or so human genes. Two main components leading to gene transcription (decoding): 1. Transcription Factor (TF) proteins a. Usually contain multiple domains i. DNA binding domain (usually to only 4-6bp sequences) with similarities TF proteins can be grouped into distinct families, which often bind to similar DNA sequences, such as… 1. Homeobox 2. Basic helix-loop-helix 3. Zinc finger ii. Transcription activation domain iii. Protein-protein interactions domain 1. Some common interactions shared within and between TF protein families 2. DNA sequence motifs within regulatory genes to which the TF proteins bind. a. Random occurrence would have the 4-6bp sequences appear far more commonly than the number of genes being regulated thus there must be more than just simple sequence recognition. Appears that regulatory genes are associated with clusters of TF recognized binding sequences (up to 5)—in contrast to the randomly occurring sequences, which are more isolated/solitary. b. Clusters of binding sites plus protein-protein interactions lead to assembly of high-order complexes. i. Data suggests some TF complexes exist in the nucleoplasm and thus are at least partially pre-formed prior to DNA binding. High-order complexes allows for genes to have networks receiving input from multiple upstream regulators with antagonistic or synergistic interactions (crosstalk). 1. Difficult to model as many different interaction combinations 2. Recent models based on pooled experimental data developed c. One model based on 11 TF proteins controlling common myeloid progenitor (CPM) differentiation (PLoS ONE 2011;6(8):e1000771). i. Encodes the combined logic governing the interactions in which 1. TF are either “ON” or “OFF” 2. Interactions use logic functions “AND”, “OR”, and “NOT” ii. Held up well when predicting consequences of gene knockouts and over-expression in terms of the 4 terminal cell line differentiation (neutrophils, erythrocytes, monocytes, and megakaryocytes) iii. Was not able to account for means by which the CMP pool (stem cell/progenitor pool) was sustained d. A second model based on 10 stem cell TF proteins identified HSC-like gene expression as a stable attractor state (Bioinformatics 2013;29(13):i80-i88). i. Focused on cross-regulation between TF proteins via numerous positive feedback loops ii. Requires simulation of external triggers allowing for exit toward more differentiated states e. Reality is HSC can balance both self-renewal and differentiation so neither of the above models is completely accounting for the real complexities What leads to the production of these transcriptional factor proteins is also of interest as these are also gene products that would require transcription regulation. Cooperative TF binding is only the first critical step regulating gene expression 1. Recruitment of a. Accessory proteins, such as chromatin-modifying enzymes b. Multiple components of RNA polymerase holocomplex 2. Transcriptional elongation 3. RNA processing 4. Nuclear export 5. Translation 6. Post-translational modifications Let’s also briefly introduce the concept of micro-RNA MicroRNA are small non-coding RNA sequences, which (often negatively) regulate translation of coding mRNA by binding the untranslated 3’ region of the target RNA. They occur evolutionarily in association with increased organismal complexity. It is hypothesized that microRNA may be a means by which evolutionary adaptation may occur more quickly as it is likely easier to develop novel microRNA compared with novel coding genes. The microRNA genes are often located within coding gene introns or very near to coding genes. Hematopoietic Regulation -- Summarizing Every process of hematopoiesis (stem cell survival, self-renewal, proliferation, and differentiation) is orchestrated by a combination of growth factors, cytokines, microRNA, and transcription factors. Cytokines are hormone-like chemical signals (hematopoietic cytokines) within the "microenvironment" provided by the stromal cells and extracellular matrix of the bone marrow. The cytokine and colony stimulating factor composition of the microenvironment is dynamic in response to local and systemic factors/needs. Each cytokine and colony stimulating factor has its target(s), but the response to these factors is not hard fast. The response varies depending upon the other cytokines and CSFs present within the local microenvironment at that precise point in time; the surface receptor types and numbers present on the cell at that point in time; and the composition of intracellular microRNA and transcription factors present at that point in time. SO now let’s look at how these processes might occur in regulating hematopoiesis, recognizing that even our discussion will not be able to describe the full complexity but merely highlight some aspects of the process. Granulopoiesis As an example, we will start by looking more closely at the process of granulopoiesis, which is the differentiation and maturation of the granulocytic cells and monocytes. As part of the discussion we will highlight a few key regulatory components, by way of examples, including two transcription factor proteins, GATA2 and PU.1 As with all of the hematopoietic cells, the granulocytes derive form the pleuripotent hematopoietic stem cell. We will recall that there is an ongoing balance being orchestrated at the stem cell level—the balance between maintaining the stem cell pool (self-renewal) and differentiation (lineage commitment). Let’s digress for a moment to discuss GATA2… GATA GATA is a group of 6 TF proteins, which belong to the zinc-finger family of TF proteins—these contain 2 zinc finger domains. GATA2 is located on the long arm of chromosome 3 at position 21.3 1. In embryonic development, GATA2 pivotal in endothelial to hematopoietic transition that produces the first HSCs. As such, homozygous knock-out is lethal. 2. In adults, GATA2 is required for HSC survival and self-renewal What are the targets of GATA2? 1. GATA2 cooperates with six other TF proteins to form a heptad regulatory unit. These other factors include: TAL1, LYL1, LMO2, ERG, FLI1, and RUNX1). Targeted genes of the heptad include microRNAs and are lineage-specific. 2. GATA2 also has direct targets including a. GATA1 b. PU.1 c. CEBPa 3. GATA2 also interacts directly with FOG1, PU.1, and CEBPa Haplo-insufficiency of GATA2 still allows for cell differentiation, but it also appears to lead to a depletion of the HSC pool (i.e. appears to lead to impaired HSC self-renewal). Conversely, over-expression of GATA-2 appears to impair differentiation. Thus, balancing self-renewal and differentiation appears to be a major component of GATA2 function. Clinical syndrome associated with GATA2 deficiency / mutations autosomal dominant with >90% penetrance 1. MonoMAC = monocytopenia with increased susceptibility to atypical mycobacterial infections. 2. Loss of dendritic cells, monocytic B-cells, and NK cells. 3. Familial AML/MDS 4. Pediatric neutropenia with aplastic anemia Longitudinal study of kindreds suggested a progressive course related to impaired cellular immunity 1. Increased warts (related to HPV infection susceptibility), herpes viruses, etc.. 2. Mononuclear cellular loss over time ultimately severely so (monocytopenia, DCs, B-cells, and NK cells with a decreased CD4:CD8 ratio <1) 3. MDS often at younger ages with median 21-33 years (lifetime risk 90% with hereditary MDS pattern)—often normal to hypocellular with megakaryocytic atypia and fibrosis on the marrow examination and often with better preserved Hgb, Plts, and neutrophil counts compared with other MDS patients. Lymphocyte subset analysis by flow will reveal a profound depletion of B-cells and NK cells. Often association with progressively increased FLT3 ligand concentrations. 4. Pulmonary alveolar proteinosis 5. Infection with mycobacterium, fungi, and lymphedema. 6. Increased infection related cancers (related to HPV, EBV, etc…) but also skin and breast cancers. 7. Increased risk of AML (hereditary AML cases)