Clinical Uncertainty in Primary Care
advertisement

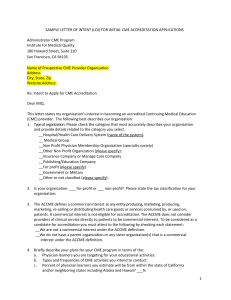
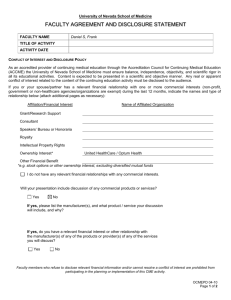
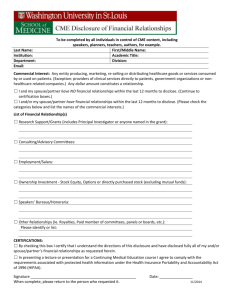
Clinical Uncertainty in Primary Care: The challenge of collaborative engagement Chapter 9 Practice Inquiry: Uncertainty Learning in Primary Care Practice On-line Resource #2 The CME Programs: Practice Inquiry - Improving Clinical Judgment and Clinical Practice, at the Department of Family & Community Medicine at University of California, San Francisco,and at Kaiser Permanente Medical Center Oakland, California Lucia S. Sommers, DrPH The Practice Inquiry CME Program at UCSF based in the Department of Family and Community Medicine began in 2005 preceded by 2 ½ years of pilot work. As of summer 2012, seven PI groups are part of the program. Two PI groups have been meeting in Kaiser Permanente Medical Centers based in the Department of Medicine; one group has been CME- certified since 2005 and the other group is currently applying for accredited CME status. In the US, most states require physicians and mid-level practitioners to obtain ‘CME credits’ in order for licensure renewal. Practice Inquiry Groups Group Site Affiliation First Mtg Date Current Members Meeting Frequency/ Time Facilitation 1. Maxine Hall Health Center (San Francisco)) Community health center (publicly funded) 2002 6 PCPs 1 NP Every other month LS 2. Asian Health Services (Oakland) Community health center (publicly funded) 2004 22 PCPs 1 PA Weekly MD member Private Non-profit HMO 2004 4-7 PCPs 2-3 specialists MD member Private, non-profit, university sponsored 2005 6 PCPs 2 NPs Monthly, ON HOLD (Physician facilitator retired) Monthly Community health center (publicly funded) 2006 Every other month LS Private practice 2006 5 PCPs 1 NP 1 Specialist 3 PCPs 1 NP 7. Axis Health Center (Pleasanton) Community health center (publicly funded) 2009 6-8 PCPs 1 NP 8. Sutter East Bay Foundation (Albany) Hospital system-owned PCP group practice 2010 6 PCPs 2 NPs Monthly LS 9. Kaiser Permanente (Richmond) Private Non-profit HMO 2010 7-9 PCPs 3-4 specialists Weekly MD member (in Northern California) 3. Kaiser Permanente (Oakland) 4. Lakeshore UCSF FM Faculty Practice (San Francisco) 5. Potrero Hill Health Center (San Francisco) 6. Baywest (San Francisco) Monthly, ON HOLD (Lost members; new hires as of 7/12) Monthly PCP- primary care physician, NP- nurse practitioner, PA – physician assistant, LS- Lucia Sommers 1 LS MD members LS MD member Funding: $500 annual accreditation review fee waived by UCSF as a community service in the interest of supporting non-commercial, practice-based CME; no fees at Kaiser Permanente CME Program Clinician Educational Objectives: To share uncertainties in managing difficult/complex patients with colleagues To practice blending multiple clinical judgment input into strategies for engaging uncertainty To identify recurring uncertainties requiring clinic-wide educational/ system interventions CME Program Group Participation Requirements: Minimum of 3 clinicians to count as CME credit-worthy (Category 1 CME credit) Facilitator present (4th group member or external person of group’s choosing) Case log maintained (See example case log below.) Participant comments via annual PI Feedback Questionnaire (See Figure 1 attached.) UCSF CME Program (#MGR12059) Department of Family and Community Medicine PRACTICE INQUIRY (Name of Group) CASE LOG (November – January ) Date # 11/18 #69 1/20 2 Clinical Uncertainty Case Description/Issues Feedback/Discussion Pt. cancelled apt with PCP Implications for larger practice – should we tell patients about potential adverse effects of certain antibiotics (e.g., cipro) and sterioids? To do lit review: frequency of tendon rupture with levaquin & cipro, “I’m not sure what needs to be done Pt currently on seroquel, Consider getting EKG to look at QT next.” 75yo female experiencing clonopin, lomectil, coumdin, interval drug interaction between Seroquel digoxin, and flecamide. Gets Consider referring to new and her cardiac meds – SOB and SOB and tachy, hot and sweaty cardiologist. New tachy while walking. I need to while walking; anxiety re To do lit review on how seroquel negotiate management changes falling. Cardioverted with no interacts with cardiac meds with pt’s psychiatrist and improvement; now to receive cardiologist to reduce symptoms holter “He keeps getting admitted… looks Mid 70’s male with CHF from Common CHF dilemma like patient and daughter have given Pakistan lives with caregiver Placement in B&C, nursing daughter; HTN, DM; home? up trying.” New ambulatory , 02 dependent; 4 Ready for hospice? admits in 4 months, non Depressed? (anti-depressants compliant with meds, now on were prescribed but probably doesn’t take) verge of being admitted again. Follow-up #56: 39 yo female with At lastdoes visit,he complaining oflife? What want out of many atypical problems over a lot of referredreferral to GI, abdom Considerpain; counseling systems (hx of Cushings syndrome, negative colonoscopy.; not pos adrenal insuffic, PCOS, and anti-coag. ovarian mass being worked up at Keeps cancelling visits at last Old UCSF OBGYN; post chole developed minute and only comes when DVT on BCP; warfarin rx failed to in crisis impact INRs,) struggling with the Consider phone call/letter to insurance company to cover her lay out terms of relationship Lovenox Follow-up #68: 25 yo male prescribed Levaquin for bad bronchitis (ABX allergies); subsequently complained couldn’t Old move shoulder; saw commercial regarding tendon rupture caused by Levequin 11/18 1/20 New/ Old #72 JO Key Statistics: Largest number of groups in any one year: 14 Number of groups meeting for at least 3 years: 10 Number of groups meeting for at least 5 years: 6 Number of groups meeting regularly for at least 18 months no longer participating: 3 Program Evaluation: Case Series Analysis (150 cases) o Uncertainty type: 33% diagnostic, 25% management uncertainties, 23% diagnostic/management; 19% clinician-patient relation o 15% - adverse outcome; 8% End-of-life o Top 7 condition types: morbid obesity, chronic pain, use of the prostate specific antigen (PSA) test, lipid abnormalities, and incidental findings on studies, bi-polar disorders, and patients with both diabetes and hypertension. (See On-Line Resource #3 “Practice Inquiry Clinical Uncertainty Taxonomy” for a description of the work underway to categorize 350 uncertainty cases using an automated data collection and categorization tool.) Seven- Year Trend Analysis (Data collected via annual PI Feedback Questionnaire; see Figure 1, attached.) Practice Inquiry Clinician Self-Report Trend Analysis Program Years # SF Bay Area Groups #Forms distributed Response Rate Overall Value* % Clinicians writing case comments ** 2005-06 7 2006-07 9 2007-08 10 2008-09 6 2009-10 7 2010-11 8 2011-12 7 60 110 72 65 77 83 57 80% 71% 75% 55% 73% 68% 79% 3.9 4.0 unavailable 4.0 3.8 4.1 4.0 58% 67% 67% 57% 47% 51% 66% *5-point Likert scale, 5 = highest value **Examples “Blind older female with chronic renal disease and diabetes needing to use insulin but refusing. Came here daily for injections but can’t continue forever.. Patient refusing to self-inject; no family. Group advised to offer oral meds and if in the end the patient refuses, then to just accept that it’s the patient’s choice” “Elderly female with anemia - will check an additional test and then stop worrying about it” “Long-term use of Fosamax in patients who have been on it for >5 years; I’ll repeat Dexa and consider DC-ing med” “Patient with newly diagnosed lupus. Since patient not be able to be seen by specialist for a couple of months, what should I be doing if the patient is not having a flare…Patient has mildly elevated ESR. Question: without symptoms, need to lower ESR? Group thought ‘no.’“ “Patient with chronic pain, depression, poor motivation. Brought to the group – came away with different interpretation of patient behavior – ultimately more successful management of the patient” 3