2-18-14 edits Education Description
advertisement
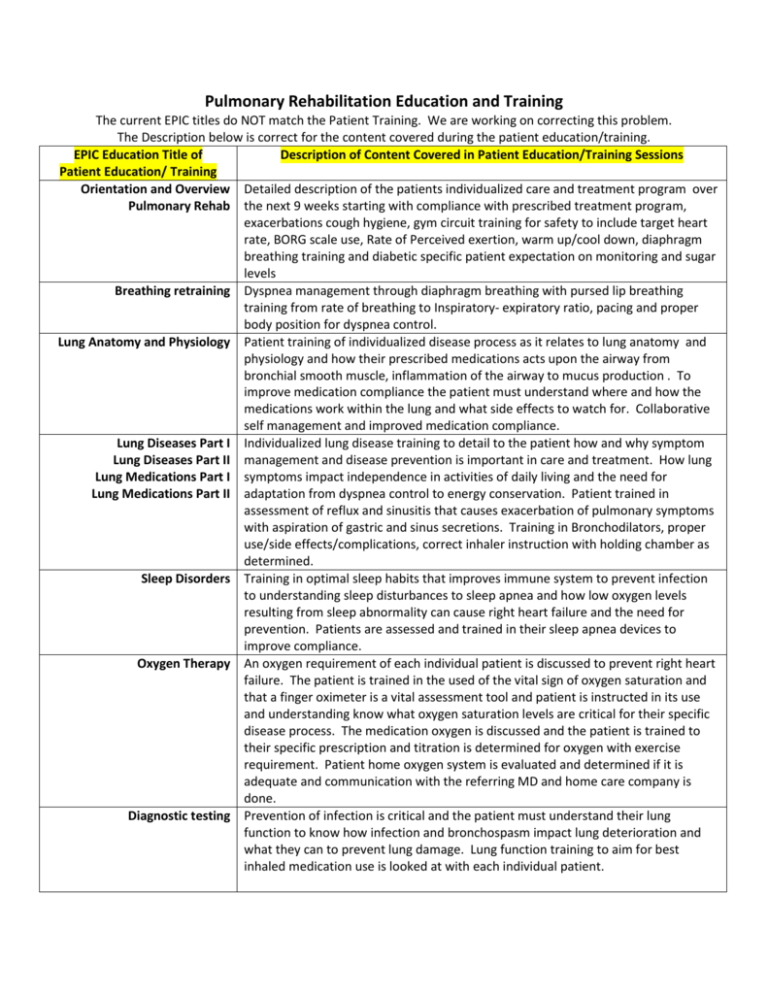
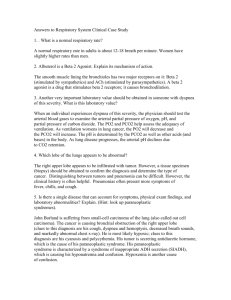
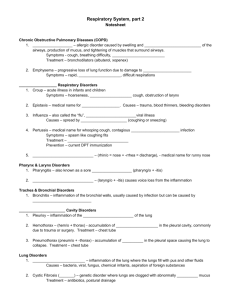
Pulmonary Rehabilitation Education and Training The current EPIC titles do NOT match the Patient Training. We are working on correcting this problem. The Description below is correct for the content covered during the patient education/training. EPIC Education Title of Description of Content Covered in Patient Education/Training Sessions Patient Education/ Training Orientation and Overview Detailed description of the patients individualized care and treatment program over Pulmonary Rehab the next 9 weeks starting with compliance with prescribed treatment program, exacerbations cough hygiene, gym circuit training for safety to include target heart rate, BORG scale use, Rate of Perceived exertion, warm up/cool down, diaphragm breathing training and diabetic specific patient expectation on monitoring and sugar levels Breathing retraining Dyspnea management through diaphragm breathing with pursed lip breathing training from rate of breathing to Inspiratory- expiratory ratio, pacing and proper body position for dyspnea control. Lung Anatomy and Physiology Patient training of individualized disease process as it relates to lung anatomy and physiology and how their prescribed medications acts upon the airway from bronchial smooth muscle, inflammation of the airway to mucus production . To improve medication compliance the patient must understand where and how the medications work within the lung and what side effects to watch for. Collaborative self management and improved medication compliance. Lung Diseases Part I Individualized lung disease training to detail to the patient how and why symptom Lung Diseases Part II management and disease prevention is important in care and treatment. How lung Lung Medications Part I symptoms impact independence in activities of daily living and the need for Lung Medications Part II adaptation from dyspnea control to energy conservation. Patient trained in assessment of reflux and sinusitis that causes exacerbation of pulmonary symptoms with aspiration of gastric and sinus secretions. Training in Bronchodilators, proper use/side effects/complications, correct inhaler instruction with holding chamber as determined. Sleep Disorders Training in optimal sleep habits that improves immune system to prevent infection to understanding sleep disturbances to sleep apnea and how low oxygen levels resulting from sleep abnormality can cause right heart failure and the need for prevention. Patients are assessed and trained in their sleep apnea devices to improve compliance. Oxygen Therapy An oxygen requirement of each individual patient is discussed to prevent right heart failure. The patient is trained in the used of the vital sign of oxygen saturation and that a finger oximeter is a vital assessment tool and patient is instructed in its use and understanding know what oxygen saturation levels are critical for their specific disease process. The medication oxygen is discussed and the patient is trained to their specific prescription and titration is determined for oxygen with exercise requirement. Patient home oxygen system is evaluated and determined if it is adequate and communication with the referring MD and home care company is done. Diagnostic testing Prevention of infection is critical and the patient must understand their lung function to know how infection and bronchospasm impact lung deterioration and what they can to prevent lung damage. Lung function training to aim for best inhaled medication use is looked at with each individual patient. Pulmonary Rehabilitation Education and Training 2 EPIC Education Title of Description of Content Covered in Patient Education/Training Sessions Patient Education/ Training Emotional and Individuals mental and emotional functioning is evaluated and an individualized Social Well-being treatment program is determined to aid in the anxiety, depression and coping mechanism. Training the patient in how their family and home situation affects their treatment program and involving the family members in the patient’s treatment program. Panic control Dyspnea control is through patient training for Panic control with breathing Relaxation Techniques retraining, pursed lip breathing and muscle tension relaxation techniques for improved breath control Nutrition Training in the role of nutrition/food/vitamins in the treatment and prevention of infections, weight and how it impacts breathing and increases the work of breathing to knowing their best BMI. Patient hydration is critical to keep the mucus cells in the lung moist to facilitate a good cough technique with mucus expectoration. Diet and relations to the patient’s blood sugar must be understood. Also the impact of medication and food interactions as individually determined. Fall Prevention Discussing how to make pt’s home safer, fall risks, balance exercises to improve balance to prevent falls Preventing infection Preventing Infection: self management to minimize exacerbations, recognizing triggers, warning signals of infection and determining the patient flu and pneumonia vaccine use and to education the patient when these vital vaccinations should be done. Airway Clearance Airway clearance techniques & devices, to maintain proper bronchial hygiene to prevent exacerbations, decrease dyspnea and enhance quality of life. Advanced Directives Stress and end of life issues must be understood by the patient and how their family and home situation is part of advanced care planning from a power of attorney in health care, palliative care to hospice. Quality of life is improved when the patient has accepted and done advance care planning. Energy Conservation Energy Conservation/performing ADL’s with proper breathing techniques, pacing & assistive devices. Benefits of exercise Individualized Target HR training and how on “bad” breathing days the patient should interval exercise. Patient is trained in the components of their safe exercise program to include: intensity, frequency, duration and mode. Patient is trained in the use of the BORG scale at home to enhance collaborative self management. RPE, pain scale, exercise progression, disease management and long term adherence is individualized for each patient. Community Resources Psychosocial intervention is available for the patient through community programs and this training provides the patient with individualized community resources to enhance compliance with their treatment program, maintain their exercise program and provide psychosocial support through community support groups. Home Recommendations Individualized patient treatment program is reviewed with each patient and written out for the patient to include: their ongoing Exercise program and THR/BORG monitoring levels to medication needed for prevention of infection and maintenance of their disease process to the psychosocial needs of the patient.