searo
searo
Home
About
WHO in
SEAR
SEAR
Countries
Topics
List
Regional
Health
Situation
Informati
on
Sources
Related
Websites
Communi
cable
Diseases
Tubercul
osis
searo
xml_no_dtd
Communicable Diseases Department
Tuberculosis
TB in South-East Asia
Epidemiology
Goals and
Objectives
Achievements
Key Milestones achieved in
2008
Country
Profiles
Achievements
DOTS coverage
DOTS coverage is defined as the population living in administrative areas where DOTS services are
available. This indicator serves as a proxy for people with access to DOTS. Population access to
DOTS in the Region has been 100% since the end of 2006.
Case notifications
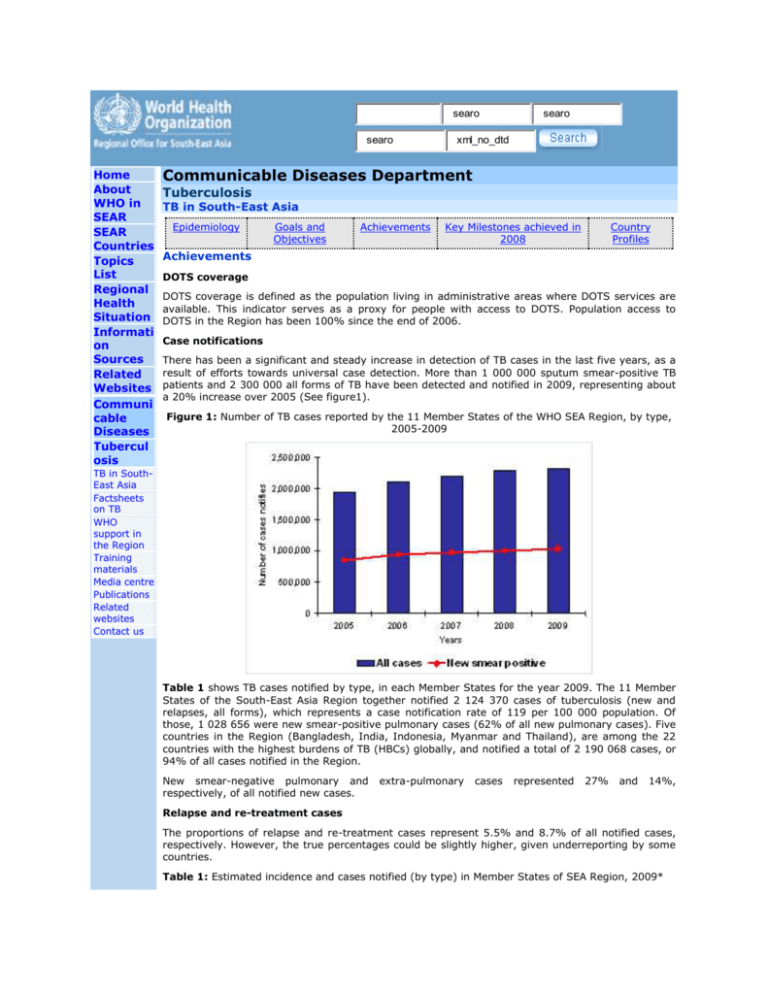
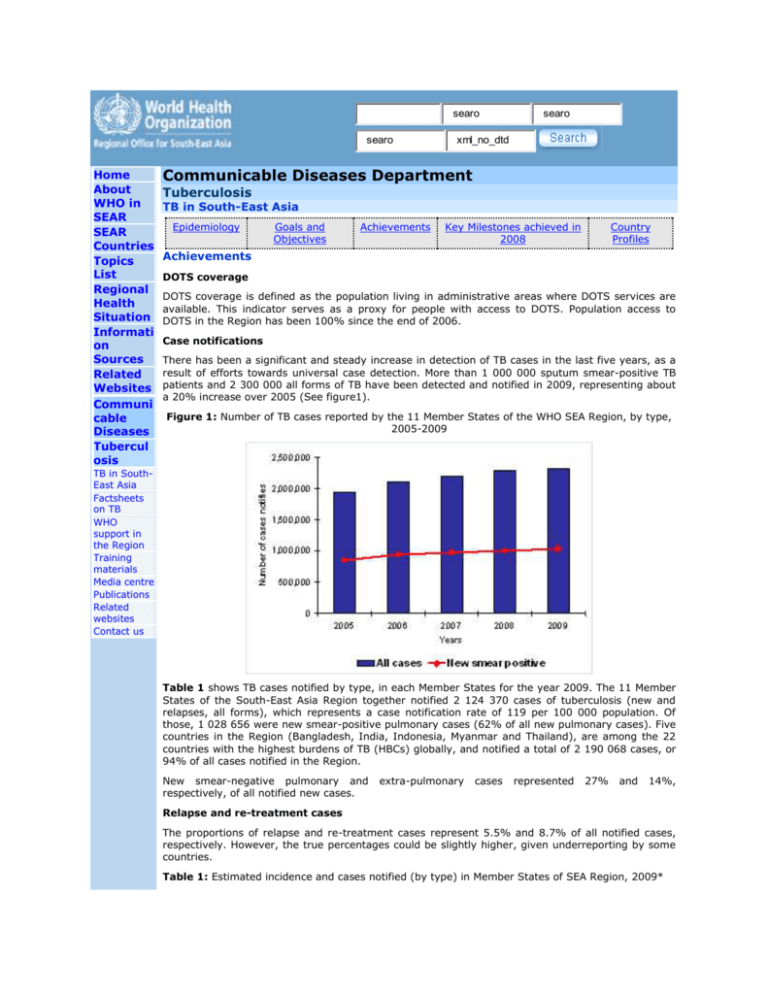
There has been a significant and steady increase in detection of TB cases in the last five years, as a
result of efforts towards universal case detection. More than 1 000 000 sputum smear-positive TB
patients and 2 300 000 all forms of TB have been detected and notified in 2009, representing about
a 20% increase over 2005 (See figure1).
Figure 1: Number of TB cases reported by the 11 Member States of the WHO SEA Region, by type,
2005-2009
TB in SouthEast Asia
Factsheets
on TB
WHO
support in
the Region
Training
materials
Media centre
Publications
Related
websites
Contact us
Table 1 shows TB cases notified by type, in each Member States for the year 2009. The 11 Member
States of the South-East Asia Region together notified 2 124 370 cases of tuberculosis (new and
relapses, all forms), which represents a case notification rate of 119 per 100 000 population. Of
those, 1 028 656 were new smear-positive pulmonary cases (62% of all new pulmonary cases). Five
countries in the Region (Bangladesh, India, Indonesia, Myanmar and Thailand), are among the 22
countries with the highest burdens of TB (HBCs) globally, and notified a total of 2 190 068 cases, or
94% of all cases notified in the Region.
New smear-negative pulmonary and
respectively, of all notified new cases.
extra-pulmonary
cases
represented
27%
and
14%,
Relapse and re-treatment cases
The proportions of relapse and re-treatment cases represent 5.5% and 8.7% of all notified cases,
respectively. However, the true percentages could be slightly higher, given underreporting by some
countries.
Table 1: Estimated incidence and cases notified (by type) in Member States of SEA Region, 2009*
Estimate
TB cases notified
d
incidenc
e - All
forms
New New
New
Treatm Treatm Other
Countr
(in
smea smear
Type
Total
extra- Relap
ent
ent
rey
thousan
runkno notificati
pulmon
se
after
after
treatm
ds)
positi negati
wn
ons
ary
failure default
ent
(Confide
ve
ve
nce
intervals
)
Banglad
esh
Bhutan
360
(300340)
1.1
(0.9-1.3)
109
402
434
25 375 21 999
285
355
4 099
0
0
0
0
160 875
51
16
9
0
0
1 150
2 247
2 312
1 651
8 366
0
88 665
DPR
Korea
82
(70-96)
29
366
India
2 000
(1 600-2
400)
624
617
384
113
233 026
108
361
18 870
73 549
88 976
Indonesi
a
430
(350520)
169
213
108
616
11 215
3 710
225
723
1 030
0
294 732
Maldives
0.12
(0.100.14)
45
13
41
1
1
2
1
0
104
Myanma
r
200
(160240)
41
357
4 558
1 331
518
3 247
0
133 439
Nepal
48
(39-58)
15
442
Sri
Lanka
13
(11-16)
32 491 12 232
50 919 31 509
9 794
7 054
2 598
279
240
0
0
35 407
4 764 1 996
2 358
196
89
124
261
0
9 880
9 143
1 964
575
726
664
0
65 940
406
41
8
3
0
0
4 759
102
545
1 796
2 328
237
Thailand
93
(75-110)
TimorLeste
5.6
1 206 3 095
(4.6-6.8)
32
810
20 058
3 300
SEA
1 028
(2 900-3
Region
656
700)
636
755
329
338
127
826
23 706 77 545
SEA
Region
(2008)
635
943
310 830
122
836
23 681
0.1%
5.6%
3.9%
0.1%
N/A**
1 796 1 533 286
1 007
385
Percentage change
2009 vs. 2008
2.1%
82 661 102 151 1 866 2 287 512
-6.6%
0.4%
-3.9%
1.7%
*Figures may be updated in early 2011 following revision or completion of surveillance data by
Member States
**The calculation method for estimates changed in 2010, and therefore new and old estimates
should not be compared.
Treatment outcomes
Table 2 shows the treatment success rates among new smear-positive cases and re-treatment cases
enrolled for treatment in the Member States during 2008. For new smear-positive cases the
treatment success rate is above the target of 85% in the SEA Region as a whole, and this target has
been achieved or surpassed in 9 of the 11 countries.
The overall cure rate in the Region for new smear-positive cases was 84.2% and the completion rate
3.8% (overall success rate of 88%), for the 1 011 353 cases registered in 2008.
The success rate among re-treatment cases is lower, 74% for the whole Region, and ranging from
66% to 82% in the countries. Similarly, while the case fatality rate among new smear-positive cases
is low, it is more than double among the re-treatment cases. Default rates are also higher among retreatment cases, and are especially high (for all cases) in India, Sri Lanka and Timor-Leste.
Table 2: Treatment outcomes of new smear-positive cases and re-treatment cases notified in 2008
in Member States of the SEA Region (expressed as percentage of the total number of cases
notified)*
New smear-positive cases*
Countri
Notifi
es
ed
Succ
ess
rate
Re-treatment cases*
Not
Case
Failu Defa evalua
Succ
fatal
Notifi
re
ult
ted
ess
ity
ed
rate rate /trans
rate
rate
fer out
Not
Case
Failu Defa evalua
fatal
re
ult
ted
ity
rate rate /trans
rate
fer out
Bangla
desh
106
089
91
4
1
2
2
509
1
-
-
-
-
-
Bhutan
354
91
3
3
0
3
70
79
3
16
1
1
DPR
Korea
28
026
89
2
4
2
2
14
170
82
3
10
3
2
India
615
977
87
4
2
6
1
289
285
74
7
4
13
2
Indone
sia
166
376
91
2
1
4
2
5
430
72
4
3
14
7
Maldiv
es
53
45
4
0
11
40
0
0
0
0
0
0
Myanm
ar
41
247
85
6
3
5
2
8
631
73
12
5
7
3
Nepal
14
640
89
4
1
3
3
1
954
76
10
5
5
5
Sri
Lanka
4
646
85
6
2
7
1
393
70
8
2
15
5
Thailan
d
33
078
82
7
2
4
4
3
468
66
9
4
7
14
TimorLeste
867
85
5
0
7
3
35
71
11
6
11
0
SEAR
1
011
353
88
4
2
5
1
328
527
74
7
4
12
2
*Figures may be updated in early 2011 following revision or completion of surveillance data from
Member States
Key milestones achieved in 2009
As a result of the resolution at the Sixtieth Regional Committee held in Bhutan in 2007, the new
Stop TB Strategy has been adopted by all 11 countries and it is the basis for national TB control
plans. National TB Programme manuals have been also updated and national programme capacity
for scaling up interventions under the Stop TB strategy has being built in various technical areas.
Management of drugs has been strengthened and no stock-outs of first-line anti-TB drugs have been
reported at the national level in all 11 countries; 5 countries are receiving GDF grants; and 6 are
transitioning/fully utilizing GDF direct procurement services
All 11 countries have nation-wide quality-assured networks for smear microscopy, and laboratories
in Bangladesh, India, Indonesia, Myanmar, Nepal, Sri Lanka and Thailand have been accredited for
quality assurance for culture and drug susceptibility testing (C and DST). Two supra-national
reference laboratories have been set up in the Region.
National guidelines for the management of multidrug resistant TB (MDR-TB) have been developed
for Bangladesh, Bhutan, India, Indonesia, Myanmar, Nepal, Sri Lanka and Timor-Leste. Sites for the
management of MDR-TB under programme conditions are functional in all these countries, and
enrollment of patients is ongoing in all except for Bhutan and Sri-Lanka, where enrollment will start
in late 2010. in total, 3 000 MDR-TB patients are currently on treatment and the number of MDR-TB
treatment sites is expanding.
Ten of the 11 countries in the Region established National Coordinating committees for TB/HIV
collaborative activities. TB/HIV interventions are widely available in Thailand, which has established
a “one-stop shop” approach and India, which implemented an “intensified” package of interventions
available to 600 million people in 18 states: intervention are being expanded in Indonesia (in Papua
and Java Bali where epidemic is concentrated), Myanmar and Nepal.
Medical colleges and private sector providers are increasingly involved in working with national TB
control programmes in the Region through public-private mix (PPM) initiatives; the International
standards for TB care are being promoted through professional societies in Bangladesh, India,
Indonesia, Myanmar, Nepal and Sri Lanka to link with all private and public health professionals.
Member States reported that over 360 medical colleges, nearly 20 000 private practitioners, 2 500
NGOs, 150 corporate institutions, 1500 large public and private hospitals and 550 prisons are
collaborating in PPM initiatives.
There are several hundred community-based interventions in place in the Region, with very
encouraging examples of community-based approaches. A wealth of initiatives, particularly for case
finding and treatment support, are increasingly being incorporated into routine service delivery by
national programmes. However, systematic approaches to social mobilization are yet to be
developed and established in countries, with the possible exceptions of Bangladesh and Indonesia.
Attention to advocacy, communications and social mobilization (ASCM) in increasing across the
Region. A regional framework on ASCM will be finalized by early 2011; seven countries have
appointed ACSM focal points and ACSM activities have been included in all Global Fund for Aids
Tuberculosis and Malaria proposals.
During 2009, external monitoring and evaluation through joint reviews of the national TB
programme were undertaken in Bangladesh, Bhutan, India and Sri Lanka.
Last update: 10 December 2010
| WHO/SEARO Home| SEARO Search| Suggestions| SEARO Sitemap| Contact us|
© WHO Regional Office for South-East Asia 2012 All rights reserved
searo
searo
Home
About WHO in
SEAR
SEAR Countries
Topics List
Regional Health
Situation
Information
Sources
Related
Websites
Communicable
Diseases
Tuberculosis
TB in South-East
Asia
Factsheets on TB
WHO support in the
Region
Training materials
Media centre
Publications
Related websites
Contact us
searo
xml_no_dtd
Communicable Diseases Department
Tuberculosis
TB in South-East Asia
Epidemiology
Goals and
Objectives
Achievements
Key Milestones
achieved in 2008
Country
Profiles
Key Milestones achieved in 2008
DOTS
The entire population in the Region now lives within access to DOTS facilities; The overall
case detection rate reported in 2007 was 68.5%, close to the global target of 70%, and the
overall treatment success rate for the cohort of new smear-positive cases initiated on
treatment in 2006 was 87%. By the end of 2008, five* countries—Bhutan, DPR Korea,
Maldives, Myanmar and Sri Lanka—had achieved or maintained both global targets for case
detection and treatment success under DOTS, based on UN population figures for the
Member countries.
Strengthening national laboratory networks
External quality assurance for smear microscopy is being strengthened in all Member
countries through training of laboratory staff. Seven countries—
Bangladesh, India, Indonesia, Myanmar, Nepal, Sri Lanka, and Thailand—have at least one
national-level laboratory with facilities for mycobacterial culture and drug susceptibility
testing for the detection of MDR-TB cases. Bangladesh, Nepal and Sri Lanka are in the
process of having their national reference laboratories accredited for quality assurance of
culture and drug susceptibility testing, while additional reference laboratories are being
accredited in India, Indonesia, Myanmar and Thailand.
Recognizing that TB-HIV co-infection must be addressed effectively, national HIV/AIDS and
TB programmes in seven countries in the Region have developed national policies and
strategies for TB-HIV. National level TB/HIV coordinating bodies have been established. The
regional strategic framework for TB/HIV is also being revised and updated. TB/HIV activities
are widely available in Thailand and are being expanded in India and Myanmar. India is
implementing an intensified package of TB/HIV interventions in the nine states with a high
HIV prevalence. There has been a more than 5 fold increase in referrals from HIV
counselling and testing centres to the TB services and more than 3 fold increase in referrals
from the TB to HIV services over the last 3 years. Indonesia, with a concentrated HIV
epidemic, has established interventions in Papua and Java Bali, which are the country’s HIV
high-prevalence areas. Cross-referrals between the TB and HIV programmes have been
strengthened, and the TB recording and reporting systems in these countries revised to
include information on TB/HIV co-infection.
Bangladesh, India, Nepal, and Timor-Leste have established MDR-TB case management
under their national programmes. Nepal has recently expanded to all five regions in the
country, while India is gradually expanding services to additional states. Indonesia and
Myanmar are expected to begin enrolling MDR-TB patients in early 2009. Two countries,
Bhutan and Sri Lanka, have submitted applications to the Green Light Committee and plan
to commence MDR-TB case management in 2009.
National guidelines for the management of childhood TB were finalized in Bangladesh,
Indonesia and Myanmar. Myanmar and Nepal received their first grants for anti-TB
paediatric formulations through the Global Drug Facility (GDF), supported through
UNITAID, while paediatric grants were approved for DPR Korea and Sri Lanka.
India is introducing infection control measures in health facilities while Indonesia, Myanmar
and Thailand will undertake assessments and prepare infection control plans in 2009.
Countries have also included measures to address vulnerable populations at higher risk and
cross-border issues in their national plans for TB control and Global Fund applications.
Public and private partnerships
TB technical working groups and/or specific task forces and sub-working groups have been
established both at the regional and at national levels in Bangladesh, DPR Korea, India,
Indonesia, Myanmar, and Nepal.
A major strategy towards improving case detection and treatment success rates has been
the inclusion of public health care providers operating outside the Ministry of Health, such
as the railways, military and prison health services, as well as private providers in all
Member countries where patients seek services through the private health sector. The
International Standards of TB Care were endorsed by professional bodies-- medical
associations in India, Indonesia, Myanmar, and Nepal. Inter-sectoral collaboration and
public-private partnerships for delivery of services were further scaled up in eight Member
countries—Bangladesh, India, Indonesia, Myanmar, Nepal, Sri Lanka, Thailand and TimorLeste. Over 350 medical colleges, 22 000 private practitioners, 1 500 large public and
private hospitals, 150 corporate institutions, 2,500 nongovernmental organizations and 550
prisons are now working with national TB control programmes. Some recent initiatives in
countries were formal inclusion of pre-service training on the principles and practices of TB
control and establishing of referral mechanisms through providing lists of DOTS centres to
teaching institutes, inclusion of private laboratories in diagnostic network and QA systems,
and launching of “IMPACT” a coalition of professional associations for TB control, in India.
In 2008, India also formally established a widely inclusive national partnership, becoming
the second country in the Region to establish such a partnership, in addition to Indonesia.
Indonesia intensified training of private and public hospital and laboratory staff and
introduced coordination meetings between community health facilities and hospitals to
improve transfer mechanisms between lung clinics and puskesmas. In Myanmar, services
have been resumed throughout the network of PSI Sun Quality Clinics and the NTP plans
further expansion of public/private mix services through the Myanmar Medical Association.
There are also very encouraging examples of community-based approaches in several
countries, but these need to be systematically documented and the experiences used to
more widely replicate successful models at the national level.
Surveillance, monitoring and evaluation
TB prevalence and incidence were revised for Timor-Leste based on a review of more recent
data and trends in cases notified and for DPR Korea based on an ARTI survey completed in
2007. Annual reports were received from all countries and are being used to finalize the
Regional and WHO Global reports for 2009.
In five countries in the Region, drug resistance surveys were conducted or will continue
through 2008-2009, to assess the extent of anti-TB drug resistance among TB patients. The
overall rates of multi-drug resistant TB (MDR-TB) in the Region is 2.8 % among new
smear-positive patients and 18.8% among previously treated patients.
Surveillance for HIV prevalence among TB patients is undertaken routinely in Thailand and
in nine states in India. In Myanmar, Nepal, Sri Lanka and in the remaining states and union
territories in India, data from sentinel surveys are used to follow trends in HIV prevalence
among TB patients.
These surveys are contributing to more accurate estimations of the burden of disease. At
the same time, countries are beginning to focus on mechanisms that will ensure that
routine case notifications begin to reflect the disease magnitude and trends. Data
management software was upgraded in Myanmar and Nepal and further improvements
made in the Windows-based EPI centre software in India. Training on data management
and analysis for central and international level programme staff were conducted in
Bangladesh, India, Myanmar and Thailand.
The practice of quarterly and annual internal reviews and larger joint reviews every
two/three years, inviting international experts for joint monitoring and evaluation together
with national programmes and partners was continued. These have helped to objectively
review the performance of the respective national TB programmes, and lead to substantial
improvements in programme performance.
Resources
Domestic funding for TB control continues to account for over half of the funding for
national TB control programmes. By the end of 2008, a total of 23 proposals were approved
by the Global Fund in support of TB control programmes in the Region. In addition, nine
Member countries benefit from funds from other development partners and donor
governments with the exception of Bhutan and Maldives where the only external funds are
through WHO country budgets.
All 11 Member countries continue to access quality-assured affordable anti-TB drugs on a
regular basis through grants or direct procurement services of the Global Drug Facility.
Operational Research
National TB programmes and partners are engaged in carrying forward several operational
research projects. Examples are public-private mix (PPM) models in India and Indonesia;
field testing of new diagnostics and shorter treatment regimens in India; approaches to
community-based TB care in Bangladesh, India, Indonesia, Thailand and Timor-Leste.
In addition, some support continues to be received through the small grants scheme under
TDR. National workshops on operations research priority setting and dissemination are held
regularly in India.
Last update: 04 March 2009
| WHO/SEARO Home| SEARO Search| Suggestions| SEARO Sitemap| Contact us|
© WHO Regional Office for South-East Asia 2012 All rights reserved
searo
searo
Home
About WHO in
SEAR
SEAR Countries
Topics List
Regional Health
Situation
Information
Sources
Related
Websites
Communicable
Diseases
Tuberculosis
TB in South-East
Asia
Factsheets on TB
WHO support in the
Region
Training materials
Media centre
Publications
Related websites
Contact us
searo
xml_no_dtd
Communicable Diseases Department
Tuberculosis
TB in South-East Asia
Epidemiology
Goals and
Objectives
Achievements
Key Milestones
achieved in 2008
Country
Profiles
Goals and Objectives
Goals
The overall goal for TB control is to reduce morbidity, mortality and transmission of TB until
it is no longer a public health problem in the Region.
Objectives
The UN Millennium Development Goals (MDGs) provide a benchmark to measure the impact
of disease control and prevention programmes, including tuberculosis control.
The objectives for tuberculosis control in all Member Countries in the Region are to:
reach and thereafter sustain the 2005 targets—achieving at least 70% case detection and
85% treatment success among all TB cases under DOTS (Indicator 24),
in order to then,
reach the targets of halving TB deaths and prevalence (Indicator 23) by 2015,
in turn to
“have halted and begun to reverse the incidence of TB” as implicitly stated under Goal 6 of
the MDGs.
Millennium Development Goals, 2015
Goal 6: Combat HIV/AIDS, malaria and other diseases
Target 8: To have halted and begun to reverse the spread (incidence) of
priority communicable diseases, including TB
Indicator 23: Prevalence and death rates associated with tuberculosis
Indicator 24: Proportion of smear-positive pulmonary tuberculosis cases
detected and cured under DOTS (the internationally recommended TB
control strategy)
The Regional Strategic Plan 2006–2015
The Regional Strategic Plan for TB Control (2006-2015) describes the future directions and
focus of work for TB control in the Region. The targets and strategies in this document are
consistent with the global targets and strategies, but focus on priorities most relevant to
this Region and build on what has been achieved during the previous 5-year period.
The interventions proposed are grouped under the following 4 strategic approaches:
1. Sustaining and improving the quality of DOTS to reach all TB patients;
2. Forging partnerships to ensure equitable access to an essential standard of care to all TB
patients;
3. Establishing interventions to address TB-HIV and MDR-TB; and
4. Strengthening monitoring and surveillance to measure progress towards MDGs.
In addition, every effort will be made to ensure that there are adequate finances and
human resources to support the implementation of all the planned interventions.
Last update: 04 March 2009
| WHO/SEARO Home| SEARO Search| Suggestions| SEARO Sitemap| Contact us|
© WHO Regional Office for South-East Asia 2012 All rights reserved