Labor Deep Dive
advertisement

IHI Perinatal Community Labor Deep Dive Tool
Background:
Reliable care, understanding the process of care, and decreasing variation while
being mindful of weak signals in the system allows the Perinatal teams to now
learn about opportunities in the 1st and 2nd stage of labor.
Prerequisite: understanding of HRO concepts and proven record of execution
(IHI oxytocin bundles >95%compliance). This work builds on successful execution
of the oxytocin bundles, incorporates the work needed for effective vacuum
bundle execution, and supports enhanced understanding of the process of labor
experienced by patients in your organization.
Supporting References:
1. Nursing Care and Management of the Second Stage of Labor, Second Edition.
Association of Women’s Health, Obstetric and Neonatal Nurses. 2008.
2. Hines S, Luna, K, Lofthus J, et al. Becoming a High Reliability Organization:
Operational Advice for Hospital Leaders. (Prepared by the Lewin Group under
Contract No. 290-04-0011.) AHRQ Publication No. 08-0022. Rockville, MD: Agency
for Healthcare Research and Quality. April 2008.
3. Bakker, P.C.Kurver, P.H. Kuik, ZD.J. et al. Elevated uterine activity increases the risk
of fetal acidosis at birth. American Journal of Obstetrics and Gynecology.196,
313e311-e316.
4. ACOG Practice Bulletin. Dystocia and Augmentation of Labor. Number 49. December
2003.
5. ACOG Practice Bulletin. Fetal Lung Maturity. Number 97. September 2007.
6. ACOG Practice Bulletin. Induction of Labor. Number 107, August 2009.
7. ACOG Practice Bulletin. Intrapartum Fetal Heart Rate Monitoring. Number 106, July
2009.
8. ACOG Practice Bulletin. Operative Vaginal Delivery, Number 17. June. 2000.
9. ACOG Practice Bulletin. Postpartum Hemorrhage. Number 76. October 2006.
10. ACOG Practice Bulletin. Shoulder Dystocia. Number 40. November 2002.
11. Johnson J, Figueroa R, Garry D, et al. Immediate Maternal and Neonatal Effects of
Forceps and Vacuum-Assisted Deliveries. Obstetrics and Gynecology. 2004;
103:513-8.
Please see Perinatal Bibliography for a complete list.
1
IHI Perinatal Community Labor Deep Dive Tool
Structure
Oxytocin
Deep
Dive
1. Interdisciplinary Fetal Monitoring Education
2. Documentation tools consistent with NICD terminology
3.Weekly fetal monitoring strip and case reviews (or#4)
4. Monthly fetal monitoring strip and case reviews
5. Standard mixture and policy for oxytocin
administration
6. One standard administration order set
7. If provider opts out of standard order set, system in
place to identify and address when standardized dosage
is not followed.
8. Team definition for tachysystole
9. Clinical algorithm for identification and management of
tachysystole
10. Clinical algorithm for management of
indeterminate/abnormal FHR patterns (NICHD 2009)
11. RN empowered to call cesarean team (not to
diagnose the need for cesarean, but to activate the team)
12. RN empowered to call neonatal team
13. Consistent handoff tool {SBAR, etc} specify
14. Informed Consent for oxytocin administration
15. Individual Provider data published about
induction/augmentation rates?
Labor Deep Dive Tool
16. Gestational age criteria standardized
17. Team definition for labor
18. Team definition for normal and abnormal first stage
of labor.
19. Admission criteria standardized
20. Established criteria for augmentation.
21. Established team huddle at critical decision points in
the patient journey. Example- (1)admission, (2)when
patient is complete to review risk factors to proceed
forward, (3)other examples- after 2 hours with minimal or
no progress, discuss plan of care to include- forceps,
vacuum, CB, continuation of pushing, etc.)
22. Second Stage Algorithm in place
23. Established policy and criteria for operative vaginal
delivery ( forceps and vacuums)
24. Established team definition of normal and abnormal
second stage of labor
25. Any dual mode delivery reviewed (vacuum-forceps;
forceps-cesarean; etc)
26. Established neonatal hand off criteria
2
Yes
No
N/A
IHI Perinatal Community Labor Deep Dive Tool
Worksheet
Study Population:
(TJC PC-02 Denominator) Nulliparous patients delivered of a live term singleton newborn
in vertex presentation
OR:
(NQF Definition) Live births at or beyond 37.0 weeks gestation that are having their first
delivery and are singleton (no twins or beyond) and vertex presentation (no breech or
transverse positions). Excluded- patients with abnormal presentation, preterm, fetal death,
multiple gestation diagnosis codes, or breech procedure codes.
Random sample of 20 patients who meet the definition.
Teams will then further define the segment of the population they will work on,
example would be 1st or 2nd stage focus as a patient segment.
Team Worksheet (include all structural questions that request definitions)
Definition of Labor:
___________________________________________________________________
___________________________________________________________________
___________________________________________________________________
Team definition for normal and abnormal first stage of labor.
___________________________________________________________________
___________________________________________________________________
___________________________________________________________________
Definition of protracted labor or arrest of descent
___________________________________________________________________
___________________________________________________________________
Notes:
3
IHI Perinatal Community Labor Deep Dive Tool
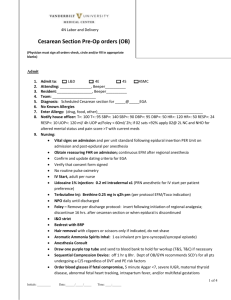
All patient records: (TJC PC-02 Denominator) Nulliparous patients delivered of a live
term singleton newborn in vertex presentation
BMI on admission _____
Gestational Age:____________
Weight gain in pregnancy___________
EFW:______________________
Diabetic Yes □
No□
1. Reason for admission:
Previous cervical ripening
Spontaneous labor
SROM
Medical induction reason
Elective Induction
AROM
Other
YES
NO
Bishops score / cervix on admit
First Stage Recognition System
Time labor Diagnosed___________ Cervical status_______________
Time of arrest of labor_____________
Time of oxytocin augmentation___________ Cervical status_______________
If patient receives oxytocin in 1st Stage, review oxytocin deep dive process
questions.
1st
Stage Oxytocin Specific Review
Process
Careful Monitoring1. Appropriate level (high risk) based
electronic fetal monitoring (or IA) for fetal
heart rate and uterine activity while oxytocin
administered.(Per Perinatal Guidelines)
2. Oxytocin initiated as intended – no delay
in administration due to provider or nursing
response.
4
Yes
No
Explanations to support the process
questions
High risk- every 15 minutes during the active phase of
the first stage of labor. Every 5 minutes during the
second stage of labor
Was there a delay in initiation or during
administration due to provider unavailability,
nursing staffing, provider staffing issues?
IHI Perinatal Community Labor Deep Dive Tool
Timely Identification3. □Tachysystole identified and managed
according to protocol /algorithm
□Tachysystole identified and managed
according to team definition and standing
orders
If tachysystole was not present, please
make sure you note this in this column but
do not collect information on yes/no unless
it is present.
□ No tachysystole present
4.
□ Indeterminate/abnormal FHR identified
Appropriate Interventions5. Oxytocin dose decreased or discontinued
during labor due to tachysystole?
6. Oxytocin dose decreased or discontinued
during labor due to FHR?
7. Oxytocin resumed after a decrease or
stop?
Note in this column if reassuring/normal
status always present.
8. Terbutaline administered?
9. Interventions needed?
10. Once labor was progressing, was
oxytocin discontinued?
Activation of Team Response
11. Documentation of physician notification
of change in dosage of oxytocin.
12. If requested, timely response by OB care
provider for bedside evaluation.
13. Escalation plan in place if needed and
documented.
__________#times
__________#times
Decrease or stop related to the presence
of tachysystole or non-reassuring FHR.
Other?
Interventions may be change in position,
IV fluid bolus, and emergency cesarean.
Was oxytocin stopped when labor pattern
was effective?
If tachysystole or indeterminate/abnormal
FHR noted, was provider supportive of
decision to discontinue medication?
Delivered by cesarean yes
no (if no proceed to 2nd Stage)
If yes, indication _______________________________________
Proceed to outcomes box.
5
IHI Perinatal Community Labor Deep Dive Tool
SECOND STAGE RECOGNITION SYSTEM
Station at start of 2nd stage: ____________
Time complete: _____________
Time pushing started: ___________
Yes
Process
No
NA
Explanations to support
the process questions
Careful Monitoring1. -Appropriate level (high risk)
based electronic fetal
monitoring (or IA) for fetal heart
rate and uterine activity if
oxytocin administered. (Per
Perinatal Guidelines).
-With or without oxytocin,
FHR and uterine activity is
recorded, interpretable and
consistent with risk level.
2. Supportive Care
-If AWHONN 2nd stage
algorithm in place, evidence it
was followed in the record.
-Evidence patient received
alternative strategies for
comfort care.
3.Powers: Uterine contractility
adequate
4.Pitocin initiated / reinitiated in
2nd stage
Timely Identification
5.FHR interpretation:
Category II or III
If identified, team documents
plan for reassessment
____minutes and exit strategy
6. EFM tracing remains
adequate for fetal assessment
during second stage
6
Consider: adequate when
entering second stage to turn off
the Pit or to go up on the Pit to
get the patient delivered.
Consider: starting augmentation
in second stage or restarted
once off for a prolonged
deceleration
Consider:
-N/A if FHR remains in Category
I.
-If Category III, evidence that
delivery occurred by internal
standards (30 minutes or less)
IHI Perinatal Community Labor Deep Dive Tool
Appropriate Interventions
7. Oxytocin dose decreased or
discontinued during 2nd stage
due to tachysystole
__________#times
8.Oxytocin dose decreased or
discontinued during 2nd stage
due to FHR?
9.If protracted, arrested or
abnormal descent identified
then team / algorithm
interventions were performed?
10. Interventions needed for
change in FHR? Document
those applied (intrauterine
resuscitation measures)
11.Pushing InterventionsIf FHR decelerations, was
pushing with every 2nd or 3rd
contraction initiated?
Activation of Team
Response
12.Documentation of physician
notification of change in status
13.If requested, timely
response by OB care provider
for bedside evaluation.
14.Escalation plan in place if
needed and documented.
15. Recognition of abnormal
2nd stage and plan
documented- may include
nursing interventions such as
positioning/pushing techniques,
proceed to delivery, expectant
management, augmentation.
7
Consider: team has
implemented this as a
multidisciplinary strategy
IHI Perinatal Community Labor Deep Dive Tool
Conclusion
Length of Second Stage:
Time of Delivery:
Mode of Delivery:
Single or dual
mode of delivery
SVD
Cesarean Section
Station:
Reason:
Vacuum
Station:
Reason:
Forceps
Station:
Reason:
NOTES:
_________________________________________________________________________________
_________________________________________________________________________________
______________________________________________________________________________
8
IHI Perinatal Community Labor Deep Dive Tool
Outcomes (T=from Perinatal Trigger
Tool)
Neonatal Outcomes
1. (T1) Apgar <7 at 5 min
2. (T2) Admission to NICU or higher
level of care
3. (T18) Instrumented delivery, vacuum
or forceps (document indication)
4. 2 or more late preterm infant (LPI
Indicators)- Respiratory distress (tachypnea,
Yes
No
N/A
Comments
retractions, nasal flaring, grunting, apnea,
cyanosis, low O2 sat)
Thermoregulation issues (temp
instability)
Hypoglycemia
Significant feeding issues (greater than
10% weight loss)
Hyperbilirubinemia (requiring
phototherapy, prolonged hospital
stay
5. (T16) Neonatal Injury (e.g. fractured
clavicle) cephalohematoma, facial
drooping, documented palsy,
hyperbilirubinemia
6. (T20) Cord gas < 7.20
7. (T22) Other Shoulder dystocia
(document morbidity)
Maternal Outcomes
1. (T7) 3rd or 4th degree laceration
2. (T9) Blood Transfusion
3. (T18) Instrumented delivery, vacuum
or forceps (document indication)
4. (T15) Excessive blood loss,
postpartum hemorrhage
5. (T22) Other Shoulder dystocia
(document morbidity)
6. Cesarean section (indication)
NOTES:
9
.