File - RMHS Dance Team
advertisement

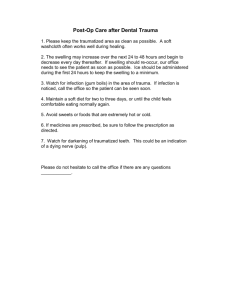
COMMON DANCE INJURIES Though there are some common dance injuries that are recognized in a general way, it is good to keep in mind that the type of dance you practice might determine its own risks. For example, female ballet dancers are likely to suffer from ankle sprains (due to the high demand on foot work); African style dancers are more in risk of getting injuries around the neck or back (due to the strong dynamics of movements executed with the spine); urban dancers have their knees in higher risk (because of the attacked flexions and screw-type extensions they do with the legs). Still, common dance injuries will mainly be those of our musculoskeletal system, derived from the constant physical demand. The following is a list of the most frequent of them, in order of severity. Below you will find an explanation of each one of them, with a description of its treatment. You may notice that there are some repeated principles that apply to the curative process of all of the common dance injuries. There are generally two different phases: an acute phase, where swelling must be handled and healing up measures have to be taken; a rehabilitation phase, where physiotherapy determines an exercising program in order to recover functionality and complete body awareness (security, stability, force and elasticity). During the acute phase, the so called R.I.C.E. principles apply for almost all cases (Rest, Ice, Compression, and Elevation). Analgesic and anti-inflammatory medication is also helpful. It is very important to find the cause or causes that created the situation to avoid its repetition. Without this, there will always be the risk of a relapse or chronic sicknesses. 1. Spasm. A spasm is a sustained and involuntary contraction that happens after a muscular effort that implies an overload. Symptoms: it appears as a decrease in the width of the mobility of surrounding joints, pain (spontaneous and when touching the muscle) and severe decrease of the efficiency of the muscular group that is affected. It can be the preliminary situation of a muscular tear. Treatment: -Rest and regulation of the activity that produced the spasm. -Use of physical, local means: wet heat, deep heat (ultrasound or short waves), professional massage (with use of oils or lubricants), soft mechanical stretching. -Use of analgesic and anti-inflammatory medication. (It is said that the best way of relaxing muscles is to take painkillers. This is because there is a circular behavior in spasms, which makes a contraction to cause pain and then the pain to cause more contraction. So, by eliminating the pain, one can break that circle and release the muscular fibers). -Restart physical activity gradually and carefully to avoid a relapse. 2. Muscle or ligament tear (or strain). A muscle tear is the loss of continuity between muscular fibers. It is the consequence of a trauma or of efforts that imply overload. There are two different types of tears: longitudinal and transversal. The longitudinal tear (also known as tear of sport), happens when muscular fibers split apart and leave a breach that can produce scar tissue. When treated improperly, that new tissue causes a decrease in the efficiency of the muscle as well as possible repetitions or worsening of the injury in the same area. The transversal tear (also known as degenerative tear), happens when muscular fibers rift, loosing contact between them. This happens more frequently in the attachment between the muscle and the tendon in which it ends. Symptoms: local pain, functional loss of the affected muscular group, swelling, local hemorrhage. Treatment: • Acute phase: -It is good to use diagnostic methods like an ultrasound scan or magnetic resonance to delimitate the anatomical damage. This is especially important in the case of transversal tears, because those might need surgical repair. -Avoid overloading efforts or repetition of the exercises that caused the damage. -Apply physical means to diminish inflammation: ice, careful compressive dressings. -Analgesic and anti-inflammatory medication. -Allow a healing period before restarting the physical activity (it can last up to five weeks). • Rehabilitation phase: -Reestablish the elasticity of the muscular group or ligament. -Strengthen the zone in order to recover efficiency, security and full body awareness. 3. Tendonitis. A tendonitis is the swelling of a tendon structure, as a consequence of major traumas or repeated minor traumas. Symptoms: local swelling, pain and loss of functional capability. Treatment: -Avoid any activity that can continue causing local damage or irritation. -Careful rest, according to the severity of the swelling (because in the majority of cases there’s no need to immobilize). -Analgesic and anti-inflammatory medication. -Use of physical means: heat and cold, together with successive stretching and strengthening (they are both necessary and are done since the beginning of the treatment). -Local infiltrations with steroid anti-inflammatory medication (which has a local effect). 4. Sprain. A sprain is the partial rift of ligaments (fibers of the connective tissue) that give support and stability to the joints. They are a consequence of traumas generated by forces that produce displacements that go beyond the physiological limits and can affect the stability of the joint. Sprains are classified in groups (3 degrees), depending on the severity of the swelling, but mostly according to the augmented and abnormal mobility they produce on the joint. The most common ones are ankle and knee sprains. Symptoms: acute immediate pain after the trauma, fast local swelling, severe functional loss of the affected joint. Treatment: -R.I.C.E. principles. -Analgesic and anti-inflammatory medication. In slight cases: -Soft compressive dressings (‘Robert Jones’ compressive dressings, without elastic). In severe cases: -Possibility of rigid immobilization of the joint. The time will depend on the pain, swelling degree and alteration of stability of the joint. In the most severe cases: -Depending on the youth of the person or like in the case of dancers (whose profession is physically engaged) chirurgical repair might be needed. In all cases, a rehabilitation program will be needed in order to recover complete body awareness and functionality. 5. Dislocation. A dislocation is a partial or total loss of the physical coherence between two surfaces of a joint that should remain together. It is produced by an external force that causes the rift of several structures that support the joint (capsular ligament). A dislocation implies an imminent possibility of arterial and peripheral nerves damage (due to the displacement). It is considered as a real orthopedic emergency. Symptoms: a grotesque deformity of the joint happens as a consequence of the trauma, severe pain, total functional disability and alteration of general vital signs. Treatment: - It is very important that friends or people that are in the place of the event do not try to move or fix the affected joint. The person should be taken immediately to a medical center. -Check if there are no fractures associated to the dislocation.-Mechanical or chirurgical reestablishment of the joint’s placement. -Immobilization. • Rehabilitation phase -Functional recovery of the affected zone with physiotherapy, (stretching, strengthening and recovery of body awareness). 6. Fracture. A fracture is the partial or total loss of continuity of an osseous structure (a bone). It is generally produced by direct or indirect traumas but can also be caused by sicknesses or practices that weaken the osseous structure. Some fractures are not caused by major traumas but by repetitive minor traumas. They are called stress fractures and are common among sportive people. A fracture is considered as an orthopedic urgency. Symptoms: deformity, severe pain, swelling, functional loss and hemorrhage. Treatment: - Whenever there’s a suspicion of fracture, the area must be completely immobilized. The person should be taken immediately to a medical center, where doctors will check the diagnosis with x-rays. -The fracture might need internal immobilization (by surgery) or external immobilization (plasters or splints). The period will last until it is considered clinically and by radiological means that the fracture is healed up (there is a lapse of time recognized but it is different for each bone). -Rest and anti-inflammatory means. • Rehabilitation phase -Functional recovery of the affected zone with physiotherapy, (stretching, strengthening and recovery of body awareness). 7. Overload syndromes (also known as chronicle fatigue). The overload syndromes are local or general swelling manifestations produced by repetition, forced training or inadequate technique over muscular or ligament structures. Apparently they do not create damages but they produce pain and diminish physical capabilities. They are also a preliminary situation of degenerative injuries (any of the others above). Symptoms: pain, intensification of muscular tone, loss of elasticity, loss of the capacity of recovery after an effort and functional decrease. Treatment: -Particularly in the case of physically engaged people, it is necessary to make an evaluation of the working load and ways. The goal is to detect the facts that led to the overload syndrome and then correct them. - Once a diagnosis has been defined: -Start a progressive physical therapy. The aim is to strengthen for the load that led to the overload in such a way that the work becomes an easy task and the overload disappears. -Start occupational therapy (specialists will analyze the causes of the situation and will apply corrective measurements. -Analgesic and anti-inflammatory medication. 8. Vascular syndromes. Vascular syndromes are less frequent and do not make part of the musculoskeletal system injuries. Still, they can be caused by demanding physical activity as they can be a consequence of direct major traumas or repetitive minor traumas (like efforts or training). The vascular structures (arteries, veins and lymphatic vessels) can swell and even get obstructed. This produces local swelling symptoms that are sometimes severe, as well as all the consequences that derivate from the obstruction of the blood or lymphatic flow. Symptoms: local swelling, pain, ischemia (local, regional or total circulatory decrease in an extremity), venous congestion and diffuse swelling. Treatment: -It is important to make an early diagnosis because vascular syndromes can evolve into serious illnesses, even though the cause is not always severe. Whenever there’s a suspicion of a vascular syndrome, it is very important to visit the doctor immediately. -The doctor will decide if treating only with rest and anti-inflammatory medication or if it is necessary to make a medicated anticoagulation process or a catheterization (procedure of vascular cleansing). -Rest. This content is of high quality but is provided for general information only. It should not be treated as a substitute for the medical advice of your own doctor or any other health care professional. contemporary-dance.org is not responsible or liable for any diagnosis made by a user based on the content of this page. Always consult your own doctor if you're in any way concerned about your health. “Common Dance Injuries” was written under the direction of Doctor Juan Guillermo Naranjo, Orthopedic Surgeon. Name ___________________________________________________________ Date ______________ Per ___________ “Common Dance Injuries” Questions 1. What are the R.I.C.E. principles? Name two injuries that use R.I.C.E. as a treatment. __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ 2. What are two injuries which require going to the hospital? Why do those injuries require a hospital visit? __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ 3. What is the difference between a sprain (4) and a muscle strain (2)? __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ 4. If you were to notice that your calf muscle seemed overly sore and that you had a lot of pain when you tried to use or stretch that muscle, what would your first course of treatment be and why? __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ 5. If you landed a jump and twisted your ankle, and now your ankle is painful and swollen, what is the most likely injury and how would you begin to treat it? __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________ __________________________________________________________________________________________________