enviormental_injuries
advertisement

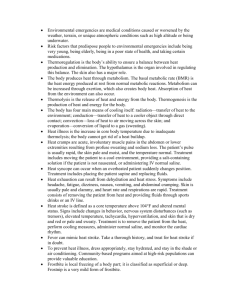
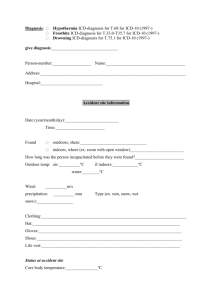
Environmental Injuries •High Altitude Sickness •Frostbite High Altitude Sickness Resulting from hypoxia Will show up within the first few days at altitude 3 types: • AMS: Acute Mountain Sickness • HACE: High Altitude Cerebral Edema • HAPE: High Altitude Pulmonary Edema High Altitude Sickness • AMS: Acute Mountain Sickness – Most common – Causes: insufficient hydration, respiration, genetics – Minor brain swelling due to hypoxic stress • HAPE: High Altitude Pulmonary Edema – Increased fluid in alveoli • HACE: High Altitude Cerebral Edema – Advanced brain swelling – 10% as frequent as HAPE High Altitude Sickness • Acclimatization Faster respiration alone cannot compensate for lower O2 levels at higher altitudes. Body must reset blood chemistry, resulting in increased respiration rate and kidney function, which produces more EPO to increase O2 uptake rate. Some people acclimatize quickly, and can ascend rapidly; others acclimatize slowly AMS: Acute Mountain Sickness S&S – What you see • Headache • Dizzy or lightheaded • Nausea HAPE = AMS + dry cough, respiratory distress, mild chest pain, Severe Case = cyanosis / sputum / rapid pulse HACE = AMS + loss of muscle coordination + altered mental state AMS: Acute Mountain Sickness Assessment • ABCs – listen to breathing sounds • LOR • Vital Signs • OPQRST – When did they get to altitude? • SAMPLE – History of altitude sickness? AMS: Acute Mountain Sickness Treatment • Descend • O2 if severe S&S, or decreased LOR • Position of comfort • Avoid exercise or exertion • Nonprescription drug for headache • Hydrate • Do not leave alone High Altitude Sickness: Prevention Gradual ascent Never ascend with symptoms of AMS Avoid overexertion Consider prophylactics: Acetazikamide (Diamox) Dexamethasone Combination of above Ginko biloba Frostbite • Frostnip • Superficial Frostbite • Deep Frostbite Rate and Severity depend on ~ wind chill, alcohol a/o drugs, altitude, getting wet or being damp, length of exposure Frostbite – what is happening? • The blood vessels constrict as a natural reaction to prevent body heat loss and hypothermia. • With a loss of warming blood flow the fluids in the body tissues and cellular spaces crystallizes • This freezing can damage the blood vessels causing blood clotting and lack of oxygen to the affected area and deeper tissues. Frostbite – Alcohol & Nicotine? • Vasodilators (eg alcohol) causes blood vessels to stay open taking heat away from inner core. Your body therefore cools down faster, promoting hypothermia, and speeding up the onset of frostbite. • Vasoconstrictors (eg nicotine) constrict the extremity blood vessels even more than the body is already doing to maintain core temperature, thereby speeding up the onset of frostbite. Frostnip (1st degree frostbite) S&S – What you see • Most often seen on cheeks, earlobes, fingers, toes • Numbed skin that has turned white in color. • Freezing of top layers of skin tissue, usually reversible • As it heals, appearance is similar to that of sunburn (a 1st degree burn). Frostnip (cont’d) Treatment • Rewarm by gently blowing warm air/placing against warm body part. • Don’t rub - can damage tissue. • Watch for S&S of hypothermia Superficial Frostbite S&S – What you see • The skin will be white or blue and will feel hard and frozen ; but tissue underneath is still soft • Blisters usually appear within 24 hours after rewarming. Superficial Frostbite (cont’d) Treatment • For resort environments, rewarming should be done under medical supervision • Rapid rewarming by immersion in warm (102° to 108°F) water. Need to monitor temp carefully – Continue for 20-30 minutes or color goes to deep red or blue – Give hot drinks and keep patient warm • Rewarming hurts! Suggest ibuprofen • Do not allow to rethaw Deep Frostbite S&S – What you see • Affected parts will have no feeling and blisters may be present. • The skin is white, blotchy and/or blue. The tissue underneath is hard and cold to the touch. Think - Frozen Chicken Deep Frostbite (cont’d) Treatment Delay rewarming until it can be done once & done well. Refreezing ALWAYS causes gangrene. • If injury is extensive & thawing is difficult, try to keep the area frozen. • For resort environments, rewarming should be done under medical supervision • If injury is small area, field rewarming can be started – Rapidly rewarm in warm water (102° to 108°F) – Completely immerse the frozen tissue – Thaw completely Deep Frostbite (cont’d) Treatment: post thaw care • Prevent refreezing • Protect the thawed tissue from trauma • Air dry the extremity carefully; don't rub • Elevate to reduce swelling • Use gauze between fingers/ toes to keep areas dry as swelling occurs. • Do not constrict the extremity Frostbite Summary ….DO’s • Have injury rewarmed under medical supervision • Stay warm after thawing. • Rest the injury (avoid walking on frostbitten feet, etc.). • Leave blisters intact & use sterile covering to prevent rupturing. • Keep affected part clean to reduce risk of infection. • Elevate the area above the heart Frostbite Summary ….DON’Ts • Don't allow thawed injury refreeze as this can cause serious/permanent injury. Best to delay warming • Don't use dry heat (sunlamp, heating pad, etc.) to thaw the injured area. • Don't rub the area with snow. • Avoid alcohol, nicotine, other drugs that may affect blood flow.