BIO 208 - Microbiology - Unit 4 - Diseases of the Gastrointestinal Tract
advertisement

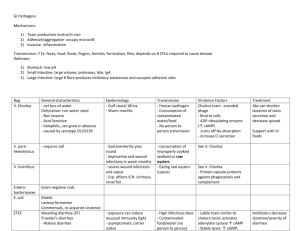
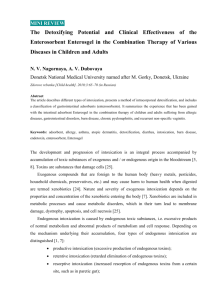
BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System This outline is intended to facilitate your preparation for lecture. This web outline will NOT substitute for regular lecture attendance. F. Food and waterborne pathogens that cause disease of the gastrointestinal (GI) system Digestive system overview CDC estimates that each year ~ 1 in 6 Americans (or 48 million people) gets sick, 128,000 are hospitalized, and 3,000 die of food borne diseases. Focus Syndrome - Gastroenteritis = inflammation of stomach & intestines - extremely common – symptoms include primarily diarrhea; sometimes nausea, vomiting, crampy abdominal pain – caused by a diverse assortment of bacterial, viral, and protozoan pathogens. General mechanisms by which microbes cause disease in the GI: A. Produce toxins B. Adhere to and damage intestinal microvilli C. Invade intestinal epithelial cells A. Diseases due to toxin production: 1. Toxin production only (no colonization of intestines) = Bacterial Food Poisoning bacteria need not enter the body they secrete toxins into the food that you ingest these toxins aren’t destroyed by heating Example organisms that cause food poisoning Bacillus cereus, Clostridium botulinum (6 cases in 2010), Clostridium perfringens, Staphylococcus aureus Toxin contaminated foods do not look, smell, or taste bad! 1 BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System Class Pick Disease - S. aureus food poisoning Agent – Staphylococcus aureus (bacterium, GPC, cat+) – infected by lysogenic phage Virulence Can tolerate moisture & salt Rapid growth between 20-37C Heat and enzyme stable enterotoxin (bacteriophage encoded) – in gut, stimulates local neural receptors that transmit to vomiting center in brain –can be produced by 1 x 105 CFU/g food. Transmission Ingestion of toxin contaminated foods – meat and meat products; poultry and egg products; salads such as egg, tuna, chicken, potato, and macaroni; bakery products such as cream-filled pastries, cream pies, and chocolate éclairs; sandwich fillings; and milk and dairy products. Seen year round – most common Nov-Dec & Jul-Aug. Contamination of food by human carrier Clinical Picture – rapid and acute onset of nausea, explosive vomiting, retching, prostration; possible diarrhea. Treatment – resolves spontaneously after ~ 24hours Frequency– one of the most common food-borne illnesses but frequency is difficult to access as hospitalizations are rare (and deaths very rare). Mortality – rare Prevention – at end of lecture 2 BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System 2. Colonization of intestines followed by toxin production Class Pick Disease – Asiatic or epidemic cholera Since 1817 there have been 7 cholera pandemics: 1832-1849 – 150,000 deaths 1866 – 50,000 deaths U.S. alone current pandemic - 1961-present – 100,000 – 200,000 cases/year Agent – Vibrio cholerae serogroup O1 (bacterium, GNcurvedR) Virulence flagella mucinase attachment 3 toxins including cholera toxin – during acute illness, patients can lose 1L fluid per hour or half of body’s fluid component in 1 day! Transmission - Cholera is generally a disease spread by poor sanitation, resulting in contaminated water supplies. In the U.S. sporadic cases occur when shellfish harvested from fecally polluted coastal waters are consumed raw. Cholera may also be transmitted by shellfish harvested from nonpolluted waters since V. cholerae O1 is part of the natural microbiota of these waters. Clinical Picture – Symptoms may vary from a mild, watery diarrhea to an acute diarrhea, with characteristic rice water stools. Onset of the illness is generally sudden, with incubation periods varying from 6 hrs to 5 days. Abdominal cramps, nausea, vomiting, dehydration, and shock; after severe fluid and electrolyte loss, death may occur. Treatment – rehydration either intravenously or orally with a solution containing sodium chloride, sodium bicarbonate, potassium chloride, and dextrose (glucose) plus tetracycline. The illness is generally self-limiting. Recovered patients may shed Vibrio for up to 1 year! Frequency – rare in U.S. (8 cases reported in 2010) Mortality – untreated, 60%. 1% with treatment. 3 BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System B. Disease due to microbes that adhere to, enter, and damage intestinal microvilli – Shigella, E. coli O157:H7, Campylobacter, Rotavirus and Norwalk virus (of cruise ship fame), Entamoeba histolytica. Class did not pick any diseases that have this mechanism of damage These are listed here just FYI – in lecture we will skip to p. 5 1. Disease - Dysentery Agent - Shigella species (bacterium, GNR, lac- Enterobacteriaceae) Virulence Acid tolerant – survive acid in stomach Exotoxin causes diarrhea Transmission Humans are only host Obligate pathogen Person-person, also contaminated food, fomites, flies Ingest small number of bact. (as few as 10 cells!) Frequency – 13,882 cases reported in 2010 2. Disease - Hemorrhagic colitis Agent – E. coli O157:H7 (bacterium, GNR, a lac- E. coli) Virulence Specific attachment via an outer membrane protein called intimin Effacement of the intestinal microvilli disrupting transport Production of shiga toxins into lumen Transmission Present asymptomatically in 50% of feedlot cattle Contaminates meat – 90% of ground meat is contaminated May be present in irrigation water produce (e.g., spinach) Infectious dose is only 1-10 cells Frequency 4,757 cases of shiga-toxin E. coli (includes O157:H7) reported in 2010. Complications and Mortality Hemolytic uremic syndrome (HUS): Persons with HUS have kidney failure and often require dialysis and transfusions. Some develop chronic kidney failure or neurologic impairment (e.g., seizures or stroke). Some have surgery to remove part of the bowel. Est. 61 fatal cases/yr; 3-5% with HUS die. 4 BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System 5 C. Disease due to microbes that adhere to and then invade across intestinal epithelial cells; may spread to deeper tissues – Salmonella, Hepatitis A, Reovirus, Enterovirus. Class Pick Disease - Salmonellosis Agent - Salmonella serotype Typhimurium and Salmonella serotype Enteritidis (non-typhoid) are most common in U.S. SE emerged in U.S. during 1980s (eggs). (bacterium, GNR, lacEnterobacteriaceae) Virulence Intracellular survival 2 enterotoxins Transmission Found in virtually all animals Most widespread of infections contracted from animals (zoonotic) Obligate pathogen in humans (never part of normal intestinal microbiota) Children more susceptible Transmitted in contaminated food (poultry (*), eggs, dairy, contaminated water) More common in summer than winter Clinical Picture - Acute symptoms 12-72 hours after infection- Diarrhea, fever, abdominal cramps. Chronic consequences - arthritic symptoms may follow 3-4 weeks after onset of acute symptoms. Treatment – generally resolves spontaneously in 4 days to 1 wk. Severe diarrhea may lead to hospitalization. In these patients Salmonella can spread from intestines blood stream with high mortality. Frequency – U.S. – 2nd most commonly reported food borne illness (Norovirus is #1). 40,000 cases reported per year U.S. (actual number of infections may be 1,200,000 or more). The incidence of salmonellosis appears to be rising both in the U.S. and in other industrialized nations. S. Enteritidis isolations from humans have shown a dramatic rise in the past decade, particularly in the northeast U.S. (6-fold or more), and the increase in human infections is spreading south and west, with sporadic outbreaks in other regions. 50,674 cases reported in 2010. Complications and Mortality - S. typhi and S. paratyphi A, B, and C produce typhoid and typhoidlike fever in humans. Various organs may be infected, leading to lesions. The fatality rate of typhoid fever is 10% compared to less than 1% for most forms of salmonellosis. S. Dublin has a 15% mortality rate when septicemic in the elderly, and S. Enteritidis is demonstrating approximately a 3.6% mortality rate in hospital/nursing home outbreaks, with the elderly being particularly affected. Salmonella septicemia (bacteria in the blood) has been associated with subsequent infection of virtually every organ system. Salmonella are becoming multiple drug resistant BIO 208 Microbiology Unit 4. Food and water-borne infections of the Gastrointestinal System Prevention and Control of Food borne Illness Careful food production, handling of raw products, preparation of finished foods Near Future Industry Advances 1. Chlorinating drinking water sources for food animals 2. Sanitary slaughter and meat processing 3. Irradiation of raw products At home 1. Wash hands (w/ soap, 20 sec) 2. Thaw in refrigerator or microwave 3. Don't cross-contaminate cooked w/raw 4. Wash fruits & veggies - even pre-washed 5. Wash knives 6. Wash countertops, cutting boards, etc. in dilute bleach 7. Clean sponges daily 8. Separate towels 9. Pay attention to "use-by" dates 10. Don't buy "bad" cans 11. Immediately refrigerate leftovers - shallow (less than 2") - less than 40ºF 6