abstract - Neurology
advertisement

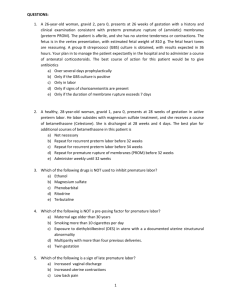
GENITAL TRACT BACTERIA LINKED TO PRETERM PRE-MATURE RUPTURE OF MEMBRANE (PPROM) AND THEIR ANTIBIOTIC SUSCEPTIBILITY PATTERN AMAH HC1, UCHEGBU U1, AMAH CC2, NDUDIM – DIKE J1, NWOSU DC EGEDE N3 and ULONEME GC4 1. 2. 3. 4. Department of Medical Laboratory Science, Faculty of Health Science, Imo State University Owerri, Imo State, Nigeria Orange Specialists Medical Laboratory, No 10 Oparaugo Street Owerri, Imo State Department of Gynaecology and Obstetrics, Federal Medical Centre, Owerri, Imo State. Department of Anatomy and Neurobiology, Faculty of Medicine, Imo State University, Owerri Imo State, Nigeria. ABSTRACT BACKGROUND: Genital tract infection has been associated with increased risks for preterm premature rupture of the membranes (PPROM). This study was carried out to ascertain the role of genital tract infection in the aetiology of PPROM as well as the antibiotic susceptibility profile of the incriminating pathogens. METHODS: A total of 102 pregnant women presented with PPROM between 24 weeks and 37 weeks of gestation and 102 control cases were enrolled while attending prenatal clinic of the federal medical centre, Owerri. The sociodemographic characteristics of the study population was taken and microbial flora were isolated using standard bacteriological methods. Disc susceptibility test was performed according to NCCLS methods. RESULTS: Pathogens were isolated in 85 patients, giving a recovery rate of 83.3%. The common pathogens include Escherichia coli (23.5%), Staphylococcus aureus (20.6%) Streptococcus spp (16.7%) and Candida albican (13.7%). Levofloxacin was the most effective antibiotics against all the isolated pathogens while ampicillin-cloxacillin was the least active. CONCLUSION: The timely detection and administration of ceftriaxone erythromycin, cefuroxime or augmentin were suggested for conservative management of PPROM. GENITAL TRACT BACTERIA LINKED TO PREGNANT WOMAN WITH PPROM AND THEIR ANTIBIOTICS SUSCEPTIBILITY PATTERN Introduction: Preterm premature rupture of membrane (PPROM) is the rupture of the fetal membranes before the onset of labour before 37 weeks of gestation. It occurs in approximately 3 percent of pregnancies and leads to one third of preterm births. It increases the risk of prematurity and leads to a number of other perinatal and neonatal complications including a 1 to 2 percent and risks of fetal deaths. The most serious outcome of preterm premature rupture of membranes is often associated with adverse maternal and infants outcomes related to infection. Studies `indicates that one of the causes is genitals tract infection, has been associated with increased risks for premature rupture of the membranes (gravett et al., 2002). Fetal membranes are made of an outer four to six layered chorion attached to a collagen rich connective tissue and an inner single cell amnion (kitzimiller et al., 2004). Hypothesis is that several organisms implicated in bacterial vaginosis secretes proteases that degrade collagen and weaken the fetal membranes leading to PPROM inflammatory markers like IL-1, IL-6 and tumor necrosis factor during infections resulting to increase in metalloproteinase causing collagen degradation, decreased tensile power of membrane and eventual rupture. Patients with PPROM may present with leakage of vaginal fluid or bleeding but without contractions. Diagnosis of PPROM is made through history from the patient and by a sterile speculum vaginal examination. Pooling of liquor in the posterior vaginal fornix or leakage of it from the cervical ostium confirms the diagnosis. Ferning of liquor is observed on the microscope or change of nitrazine paper to blue because of the alkalinity of the amniotic fluid is supportive of the diagnosis of PPROM (parry et al., 2008). The aim of the study was to estimate the incidence rate, identification and antibiotics susceptibility pattern of incriminating microbial pathogens of pregnant women with PPROM, as there was no record of this research in this locality. In PPROM, the management involves administration of antibiotics that reduces the risk of perinatal infection and increase the latency period while steroids reduce perinatal morbility and mortality (Mercer et al., 2005). MATERIAL AND METHODS A prospective cross-sectional study was undertaken involving pregnant women admitted to Federal medical centre, Owerri Imo State, southeast Nigeria, between April 1, 2013 to April 1, 2015. Federal medical centre Owerri is a tertiary hospital that serves as a referral centre for many cases of PPROM. The PPROM group comprised women (102) between 24 weeks and less than 37 weeks of pregnancy presenting to the prenatal and labour ward of the hospital with a confirmed diagnosis of PPROM. The non-PPROM control groups were invited to enroll in the study while attending prenatal clinic of the hospital. The women in the PPROM and non-PPROM groups were matched for age (+ 2 years), parity and gestational age (+ 2 weeks). The women beyond 24 weeks of gestation diagnosed to have PPROM with Diabetes mellitus, preclampsia, polyhydroamniosis, IUD, abruption, placenta previa, more than one fetus, known congenital malformation, cervical incompetence were exclude from the study. Also women were excluded from PPROM when they had had PPROM more than 24 hours prior to presentation, received antibiotic treatment within 7 days of presentation, PPROM with temperature up to 380C or active vaginal bleeding. Ethical approval was obtained from the ethical committee of the hospital and written informed consent was obtained from all the participants. Endocervical swabs were taken aseptically from all recruited women. All women were evaluated for rupture of membrane with the aid of a detailed history taking, a physical examination and a sterile speculum examination. A diagnosis of membrane rupture was made at the initial examination using standard clinical assessment criteria if two of the following three clinical signs were present: a visual pooling of fluid in the posterior fornix, a positive nitrazine test, or microscopic evidence of ferning (caughey et al., 2008). The specimen were inoculated on blood, chocolate and Mac Conkey agar plates. All plates were incubated for 48 hours aerobically with the exception of chocolate agar that was incubated in a candle jar. Thereafter, a wet mount and gram staining study was done for each specimen. Emergent colonies were identified according to standard bacteriology methods. Disc susceptibility test was performed according to NCCLS method. The results were analyzed using the statistical software of STATA 8.0 in the analysis of statistical differences was used test person CHI square and test based on an analysis of variance. The level of statistical significance was P<0.05. Table 1: Sociodemographic characteristics of the study population characteristics Age , y 16-20 21-25 26-30 31-35 36-40 41-45 Parity 0 PPROM n=102 3 10 31 42 13 3 Non-PPROM X2 (n=102) 3 0.00 11 32 41 13 1 0.03 21 20 P value 1.000 0.862 1 2 3 4 25 28 28 6 14 5 30 27 3 14 8 Gestational age, week 28-39 35 34 31-33 17 22 34-36 50 46 Level of education No formal education 2 0 Primary education 3 1 Secondary Education 31 41 Marital Status Single 2 0 Married 101 103 0.00 1.000 0.50 0.477 0.50 0.477 Table 1: Microbial flora isolated from the genital treat of participating women Organisms PPROM NON-PPROM Pvalue (n – 102) (N-102) Staphylococcus aureus 21(20.6) 3(2.8) <0.001 Escherichia coli 24(23.5) 1(1.0) <0.001 Streptococcus spp 17(16.7) 2(2.0) <0.001 Gardnerella vaginalis 8(7.8) 1(1.0) <0.001 Candida albican 14(13.7) 2(2.0) <0.001 Proteus mirabilis 3(2.9) 0 <0.150 Klebsiella pneumonia 2(2.0) 0 <0.130 Negative specimen 17(16.7) 93(91.2) <0.001 9(8.8) <0.001 Total number of positive Isolate 85(83.3) Table: 3 SENSITIVITY TO ANTIBIOTICS DRUGS AMONG ISOLATED BACTERIA IN THE PPROM GROUP Antibiotic Streptococcus spp N=17 Staphylococcus aureus Escheriachia coli N=21 N=24 Proteus Klebsiella mirabilis Pneumonia N=3 N=2 Gentamicin 13(76.5) 14(66.7) 20(83.3) 2(66.7) 1(50.0) Ceftriaxone 15(88.2) 18(85.7) 22(91.7) 2(66.7) 1(50.0) Erythromycin 12(70.6) 13(61.9) 9(37.5) 0 0 Ciprofloxacin 14(82.4) 16(76.2) 22(91.7) 2(66.7) 1(50.0) Levofloxacin 16(94.1) 19(90.5) 23(95.8) 3(100) 2(100.0) Cefuroxime 11(64.7) 12(57.1) 13(54.2) 1(33.3) 1(50.0) Ampicilin- 7(76.5) 8(38.1) 6(02.5) 1(33.3) 0 13(76.5) 15(71.4) 4(16.7) 1(33.3) 1(50.0) cloxacillin Amoxiclav Table: 4 SENSITIVITY TO ANTIBIOTICS DRUGS AMONG ISOLATED BACTERIAL IN THE NON-PPROM GROUP Antibiotic Streptococcus spp N=2 Staphylococcus aureus Escheriachia coli N=3 N=1 Gentamicin 2(100.0) 2(66.7) 1(100.0) Ceftriaxone 2(100.0) 2(66.7) 1(100.0) Erythomycin 2(100.0) 3(100.0) 1(100.0) Ciprofloxacin 2(100.0) 3(100.0) 1(100.0) Levofloxacin 2(100.0) 3(100.0) 1(100.0) Cefuroxime 1(50.0) 1(33.3) 0 Ampicillin- 0 0 0 1(50.0) 2(66.7) 0 cloxacilin Amoxiclav 3. RESULTS In total, 204 women participated in the study. The demographic characteristics of the participants are shown in Table 1. Both groups were apparently homogenous (P>0.05). The mean age of the women in the PPROM group was 30.2 + 3.2 years and the mean age of the nonPPROM group was 30.4 + 2.3 years. Most women in the study population had a parity of 0 – 2. The mean gestation age of the fetuses in the PPROM and non-PPROM groups were 32.5 + 1.5 weeks and 33.1 + 1.8 weeks respectively. Bacteria were recovered from 85(83.3%) of the specimens taken from women with PPROM (P<0.001) (table 2). Escherichia coli were the bacteria isolated most frequently in the PPROM group; while the common next organism isolated was Staphylococcus aureus (30.6%). These bacteria identified were frequently significant in the PPROM than the non-PPROM group (Table 2). In the PPROM, Levofloxacin was the most effective antibiotic: 63 (94.0%) of the bacterial isolates cultured from the 67 bacterial isolates, isolated were sensitive to levofloxacin (Table 3). Ampicillin-cloxacillin was the least effective of the antibiotics tested: only 22(32.8%) of the bacterial isolates were sensitive to the antibiotic (Table 3). The sensitivity of isolates from the non-PPROM group is shown in table 4. DISCUSSION: Despite many years of research the etiology of preterm delivery remains to be unraveled. Several studies contain the complexity of reasons both from the mothers side or the blastocyst and depending on the external environment (Hiller et al, 2005). In studies by Das CR et al., (1996) showed that infection was 2-3 times more common in patients with rupture of membranes before 37 weeks of gestation than when foetal membranes ruptured at term. In this study, we found a significant correlation between PPROM and pathogenic micro-organisms. The following bacterial pathogens were significantly isolated: Staphylococcus aureus, Escherichia coli, Streptococcus spp, proteus mirabilis, klebsiella pneumonia and Gardnerella vaginalis. According to sherman et al., 2007 the colonization of Streptococcus agalactiae or Enterobactecteriacae alone do not induce preterm labor and PPROM only lowering the percentage of lactobacilli or co-infection with other micro-organisms of high virulence (such as klebsiella spp and pseudomonas aeruginosa) increase the risk of premature contractions. In our research has confirmed that infection with Klebscella spp, etiology was positively correlated with PPROM, as klebsiella spp was not isolated from the non-PPROM group. According to Krychowska – cwkla et al., (2011), ureaplasm urealyticum, Mycoplasma hominis, Bacteriodes, Chlamydia trachomatis and Neisseria Gonorrrhoea are implicated in premature spontaneous birth. These bacterial agents may contribute to the negative specimens with no bacterial growth, as they are not cultivated by the conventional methods used in our study. The rationale for prophylactic treatment of PPROM with antibiotics is that infection appears to be both a cause and consequence of PPROM and can lead to premature delivery (Lewis et al., 1995). The administration of antibiotics in cases of PPROM forms part of the current standard care due to strong evidence that antibiotics prolong latency period in short-term neonatal morbidity by eradication of intrauterine infection and decreasing inflammatory responses (Kenyons et al., 2003). Ampicilin-cloxacillin is one of the antibiotic habitually implicated in selfmedication in Nigeria, which might explain why only 22(32.8%) of the isolates were sensitive to ampicillin-cloxacillin. Due to the teratogenic and fetotoxic concerns of quinolone, Berkovitch et al (2004) the use of effective ciprofloxacin and Levofloxacin should be discouraged. In conclusion, based on the outcome of the antibiotic sensitivity test, the use of ceftriaxone, Erythomycin and Cefuroxime and augmentin suggested for the conservative management of PPROM. REFERENCE Berkovitch M, pastoszak A, Gazariah M, Lewis M, Koren G. (2004). Safety of the new quinolones in pregnancy. Obstet Gynaecol; 84:535-538 Cauphey AB, Robinson JN, Norwits Er (2008). Contemporary diagnosis and management of preterm premature and management of preterm premature rupture of membranes Rev Obstet Gynaecol; 1 (1): 11-22. Das CR, pattnaik Pl, sahoo PLC (1996). Prevalence of vaginal infection in preterm labour. Antiseptic ; 93(4):140-43 Hiller SL, Nugent Rp, Eschen DA,, krohn MN, Gibbs Rs, Martin DH, cotch MF, and Edelman R (2005). Association between bacterial vaginosis and preterm delivery of a low-weight infant. N Engl J. Med. :333 (26):1737-42 Kenyons, Boulvain M, Neilson J (2003). Antibiotics form preterm rupture of membranes. Cochrane Database Syst Rev; 2 : CD001058 kitzimiller.J.L (2004). Preterm premature rupture of membranes. In Fuchs Fund Stubblefield P.G (eds): preterm birth: causes, prevention; and management. 1st edition Macmillan ; PP 298322. Krychowska-Cwikla A, Dmoch-Gajzlerska E (2011). Analysis of microorganisms isolated from cervical canal of pregnant women giving birth prematurely in Poland. Prog health Sc, volume 1:1 Lewis DF, Fontenot MT, Brooks GC, Wise R, perkins MS Heymann AR (1995). Latency period after preterm premature rupture of membranes: a comparison of ampicillin with and without sulbactan. Obstet Gynaecol : 86 (3): 392-5. McGregor JA, French JI, Lawellin D, Franco-Butt A, Smith C, Todd JK (2007). Bacterial protense-induced reduction of chorioamniotic membrane strength and elasticity. Obstet Gynaecol. 69 (2) : 167 – 74 Mercer BM, Arheart KL (2005). Antimicrobial therapy in expectant management of preterm premature rupture of the membranes lancet. 346 (11): 1271 – 9 Pairy S, Strauss J.F. (2008). Mechanism of disease: Premature rupture of the fetal membranes. N Engl J Med ; 338 : 663-670