About Maimonides Medical Center
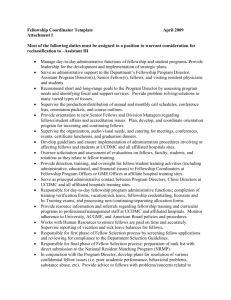
advertisement

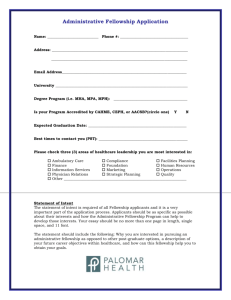
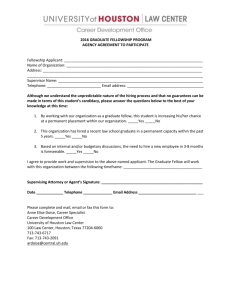
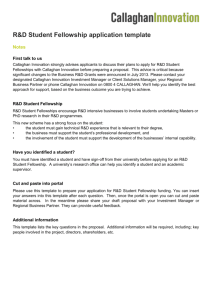
Maimonides/CIR Fellow for Quality and Work Redesign Fellowship Program Overview and Application 2012 Contents About Maimonides Medical Center .............................................................................................................................................. 2 Our History ............................................................................................................................................................................ 2 Mission Statement.................................................................................................................................................................. 2 About CIR ................................................................................................................................................................................. 2 About Maimonides/CIR Fellow for Quality and Work Redesign Fellowship ....................................................................................... 2 Program Goals/Objectives .......................................................................................................................................................... 3 Program Overview ..................................................................................................................................................................... 3 Teaching and Learning Methods.............................................................................................................................................. 4 Overall Expectations .............................................................................................................................................................. 4 Application Process .................................................................................................................................................................... 5 Benefits................................................................................................................................................................................. 5 Requirements ........................................................................................................................................................................ 5 Timeline ................................................................................................................................................................................ 5 Program Format ......................................................................................................................................................................... 6 Patient Safety Theory ............................................................................................................................................................. 6 Quality Improvement .............................................................................................................................................................. 8 Effective Change Management.............................................................................................................................................. 12 Hospital Operations .............................................................................................................................................................. 14 Key Institutional Resources ....................................................................................................................................................... 16 Main Faculty ........................................................................................................................................................................ 16 Adjunct Faculty .................................................................................................................................................................... 16 Application Form ...................................................................................................................................................................... 18 Page | 1 About Maimonides Medical Center At 100 years old, Maimonides Medical Center remains a vital and thriving non-profit, non-sectarian hospital. It is the preeminent treatment facility and academic medical center in the Borough of Brooklyn – and among the best in the country. Maimonides provides high quality compassionate patient care and community services to people of all faiths and backgrounds from the incredibly diverse population of Brooklyn. Our History Maimonides Medical Center was officially named in 1966 after Rabbi Moshe Ben Maimon, a brilliant 12th-century philosopher who laid the foundation for the modern medical training of physicians. Rabbi Maimon, better known as Maimonides, was deeply committed to cultural tolerance and humane care, in addition to high medical standards. It was he who said, “The physician should not treat the disease, but rather the patient who is suffering from it.” At Maimonides Medical Center, we have practiced our namesake’s philosophy with an unmatched passion for close to 100 years. Maimonides was founded as the New Utrecht Dispensary in 1911. In 1919, it absorbed several smaller dispensaries and became Israel Hospital of Brooklyn. In 1920 it merged with Zion hospital and became United Israel Zion Hospital. New facilities were built to accommodate the growing patient needs (the building that is now our Administration building on Tenth Avenue). In 1947, Maimonides Hospital was formed by the merger of United Israel Zion and Beth Moses hospitals. Mission Statement Maimonides Medical Center is dedicated to fostering healthy communities. We provide high quality, compassionate patient care and comprehensive community services. As a premier academic medical center, we are devoted to educating health care professionals, patients, families, employees and the communities we serve. We conduct research that improves the lives of our patients. We welcome patients of all faiths, and at the same time remain uniquely committed to serving the special healthcare needs of the Orthodox Jewish community, whose religious and cultural traditions help guide the provision of Maimonides services. About CIR The Committee of Interns and Residents (CIR) is the oldest and largest housestaff union in the country, representing more than 13,000 interns, residents, and fellows in California, Florida, Massachusetts, New Jersey, New Mexico, New York, Washington, D.C., and Puerto Rico. Membership in CIR gives residents an important voice to improve their salary and working conditions, their education and training, and the quality of care they provide to patients. CIR brings together housestaff in a chapter-based organization whose purpose is to represent its doctor-members and the interests of the patients and communities they serve through the use of collective bargaining and resident advocacy. While maintaining its unique identity and special strengths, CIR achieves its mission as an affiliate of Service Employees International Union working with other doctors and other health care employees. About Maimonides/CIR Fellow for Quality and Work Redesign Fellowship Maimonides/CIR Fellow for Quality and Work Redesign Fellowship is a part of an agreement between Maimonides Medical Center and CIR to create a Fellowship position to focus on hospital based clinical and administrative issues, system based practice, and performance improvement. Page | 2 Program Goals/Objectives The Maimonides/CIR Fellow for Quality and Work Redesign Fellowship provides didactic and mentored clinical research training for physicians. The mission is to offer opportunities to develop new knowledge for the ongoing improvement of the quality and value of health care services. The fellow will become a leader prepared to: o o o o o o Innovate and continually improve health care Learn to navigate the complex dynamics of hospitals/clinical operations Understand the scientific basis of quality improvement and patient safety Teach health professionals about health care improvement Lead healthcare professionals in improvement efforts Manage change for the improvement of healthcare Design, conduct, write and publish a research paper in healthcare improvement efforts Program Overview The Maimonides/CIR Fellow for Quality and Work Redesign Fellowship is designed to be a one-year independent experience for a qualified physician to learn about quality improvement, system design, patient safety, and the overall development of physician leadership skills. Through an intensive 12-month training period, conceptually grouped into four 3month rotations: patient safety theory, quality improvement, hospital operations, and effective change management, the fellow will learn proven tools and techniques to improve the quality, efficiency and safety of patient care within the institution. The fellow will be exposed to a wide array of tools, strategies, and methodologies in the fields of safety and quality improvement. The fellowship will have a didactic as well as an “experiential” component. In addition, the fellow can choose to enroll in a Masters in Public Health Program (tuition paid) at Brooklyn College. A central element of the training program is the development of strong mentoring relationships. The fellow will be matched with an experienced clinical mentor who will work one-on-one with the fellow and assist and monitor his/her progress throughout the program. Fellows will also participate in up to 8 hours of clinical activity per week within his/her own medical specialty, and will seek opportunities for process improvement opportunities that arise during his/her clinical work. Each fellow is required to complete a “Final Project” – a quality improvement initiative guided by his/her faculty mentor. Working with an interdisciplinary team and his/her mentor, the fellow will design and lead a quality improvement project, endorsed by senior leadership. The fellow will receive feedback and support from program as well as his/her mentor. Page | 3 Teaching and Learning Methods Fellows will: o Participate in lectures, readings, discussions, shadowing, and mentored projects; o Participate in various quality improvement committees o Participate in monthly meetings with a designated mentor on a selected patient safety or quality improvement project; o Participate in individualized meetings and discussions with Fellowship Faculty, and o Design and lead quality and safety improvement projects. Overall Expectations Learning during the Fellowship is based upon adult learning theory and designed to be active rather than passive. The fellow is expected to be responsible for his/ her own learning and is encouraged to assess his/her progress regularly with program Faculty. The fellow is responsible for completing homework assignments on specific quality improvement topics. The fellow is expected to build a portfolio of knowledge, skills and attitudes during the fellowship experience. The outcome of this work should be the development of the following competencies: o Design and make a change for the improvement of healthcare. o Plan, conduct & write-up (for a peer-reviewed journal) a research project on improvement. o Teach a group of health professionals about what they might do to improve care. Performance Improvement achievement will be assessed by a team of core Faculty at the conclusion of the Fellow’s Final Project. Graduation expectations include a final presentation based on the outcomes of the “Final Project”. Page | 4 Application Process Physician applicants must have a strong desire to become a leader in health care improvement, be self-motivated, inquisitive, creative, and eager to learn. The Fellow must know how to work well in team settings and must meet all of the following criteria: o Possess an MD or DO o Be finished with housestaff training in a primary specialty, but ideally be board certified, board eligible or the equivalent o Be committed to a career focused on patient safety and quality o Be a US citizen, non‐citizen national, or permanent resident Benefits o Salary: $70,000 o Support for travel to conferences and tuition for graduate‐level coursework (for example, MPH tuition coverage, biostatistics classes) o Research support (biostatistician, data collection and analysis training) Requirements Applications and admission to the Fellowship are on a rolling basis. As there is only one position available per year, we encourage you to apply early. The application process is designed to be simple. Interested applicants should send: 1. CV, 2. Two professional references (on official letterhead, signed, and mailed directly from the reference), and 3. A personal essay (1-2 pages) explaining why the applicant wants to pursue this opportunity and describing the professional and personal goals that will be met by completing this program. Interviews take place at Maimonides Medical Center. Timeline Applications for the first class of fellows will be accepted between January 15th, 2011 and February15, 2012 with a start date of July 1, 2012. The fellowship program cycles with the academic year (July to June). Applications are reviewed by the Joint Quality Project Fellowship Steering Committee. Page | 5 Program Format This program covers a broad range of topics conceptually grouped into four areas: patient safety theory, quality improvement, hospital operations, and effective change management. Patient Safety Theory Fellows will learn the principles of patient theory including: o o o o o o o o o Principles of system design, human factors, and high reliability Actionable improvements from a standardized adverse event. Coaching methods for disclosure and apology after an adverse event Essentials of root cause analysis Failure Modes and Effects Analysis. Designing safe systems and building a “Just Culture” Emerging trends in quality and safety theory Understanding Patient Perspectives Measurement and reporting Additional Training opportunities Structured Interviews developed by Dr. Lisa Altshuler, Department of Pediatrics (Objective Structured Clinical Exams ((OSCEs)) Crucial Conversations with Dr. Kathryn Kaplan, Vice President and Chief Learning Officer. Required Reading List: Kohn, LT, Corrigan, JM, & Donaldson, MS, (Eds.) (1999). To Err is Human: Building a Safer Health System (Executive Summary). Committee on Quality of Health Care in America, Institute of Medicine Washington, DC. National Academies Press. Reason, J. (2000). Human error: models and management. BMJ, 320:768-70. Gosbee, J. Human factors engineering and patient safety. Quality and Safety in Health Care, 11:352-54. Bloomrosen, M, Starren, J, Lorenzi, NM, Ash, JS, Patel, VSL, & Shortliffe, EH (2011). Anticipating and addressing the unintended consequences of health IT and policy: a report from the AMIA 2009 Health Policy Meeting. JAMIA, 18:82-90. Issac, T, Weissman, JS, Davis, RB, et al (2009). Overrides of medication alerts in ambulatory care. Arch Intern Med, 169(3):305-11. Watcher, RM (2010). Patient safety at ten: unmistakable progress, troubling gaps. Health Affairs, 29:1-9. Page | 6 Making Health Care Safer: A Critical Analysis of Patient Safety Practices. San Francisco, CA: University of California at San Francisco (UCSF) – Stanford University Evidence-based Practice Center, 2001. Chapter 5, Root Cause Analysis. Kizer, K. (2001). Patient Safety: A call to action. A consensus statement from the National Quality Forum (NQF). Medscape General Medicine, 3(2):10 Leape, LL (1994). Error in medicine. JAMA 272(23):1851-1857. The Joint Commission Sentinel Event Policy and Procedures. (January 6, 2011) Available at: http://www.jointcommission.org/assets/1/6/2011_DSC_SE.pdf Buckman, Robert and Yvonne Kason. How to Break Bad News: A Guide for Health Care Professionals. Baltimore: Johns Hopkins University Press, 1992. Online Independent Learning: Institute for Healthcare Improvement Open School House Modules: IHI PS 100: Introduction to Patient Safety No one embarks on a health care career intending to harm patients. But much too often, patients die or suffer injuries from the care they receive. In this course, you’ll learn why becoming a student of patient safety is critical for everyone involved in health care today. First, you’ll learn about the human and financial toll of medical error around the world. Next, you’ll learn the basics of the psychology of error and try your hand at identifying unsafe acts in real health care cases. Finally, you’ll learn five essential behaviors that any health care worker can adopt right away to improve the safety of patients. Estimated Time of Completion: 1 hour 30 minutes IHI PS 101: Fundamentals of Patient Safety This course provides a comprehensive introduction to the field of patient safety. You’ll learn the different types of errors, why errors occur, and how they can be prevented. You’ll understand effective and ineffective strategies for responding to errors when they do occur – especially with the goal of reducing, and ultimately eliminating, the chance that they’ll occur again. You’ll learn about the different kinds of error-reporting systems, and the effectiveness of each. Finally, you’ll learn about the difference between error and harm – and why reducing harm is the appropriate target of efforts to improve safety. Estimated Time of Completion: 1 hour 15 minutes IHI PS 102: Human Factors and Safety This course is an introduction to the field of “human factors”: how to incorporate knowledge of human behavior, especially human frailty, in the design of safe systems. You’ll explore case studies to analyze the human factors issues involved in health care situations. And you’ll learn how to use human factors principles to design safer systems of care – including the most effective strategies to prevent errors and mitigate their effects. Finally, you’ll learn how technology can reduce errors – even as, in some cases, it can introduce new opportunities for errors. Estimated Time of Completion: 1 hour Page | 7 IHI PS 104: Root Cause and Systems Analysis This course introduces students to a systematic response to error called root cause analysis (RCA). The goal of RCA is to learn from adverse events and prevent them from happening in the future. The three lessons in this course explain RCA in detail, using case studies and examples from both industry and health care. By the end, you’ll learn a step-bystep approach to completing an RCA after an error – and improving the process that led to the error. Note: Because RCAs are usually conducted in teams, it may be beneficial to take this course with a small group. Estimated Time of Completion: 1 hour 20 minutes IHI PS 105: Communicating with Patients after Adverse Events You chose to work in health care in order to care for people. So when you accidentally harm a patient, it can be exceptionally hard to talk about it. In this course, you’ll learn why communicating with patients after adverse events can feel so difficult for health care professionals – and why it’s nonetheless essential. You’ll learn what to say to a patient, and how to say it, immediately after such an event occurs. You’ll also learn how to construct an effective apology that can help restore the trust between the caregiver and the patient. You’ll find out what kinds of support both patients and caregivers may need after an adverse event. Finally, you’ll consider how to communicate when an error causes minor harm to a patient or does not reach the patient at all. NOTE: Because there are several opportunities for discussion during the final two lessons of this course (lessons 4 and 5), it may be beneficial to work through those lessons as a group. Estimated Time of Completion: 1 hour 30 minutes IHI PS 106: Introduction to the Culture of Safety No matter how safe we make the design of systems in which we work, there is no substitute for effective teamwork and communication. In this course, you’ll learn what makes an effective team. Through case studies from health care and elsewhere, you’ll analyze the effects of teamwork and communication on safety. You’ll learn essential communication tools, such as briefings, SBAR, and the use of critical language. Finally, you’ll learn how to use these tools when they are most essential—at transitions in care, when errors are most likely to occur. Estimated Time of Completion: 1 hour Quality Improvement Quality improvement is an interdisciplinary process designed to raise the standards of the delivery of preventive, diagnostic, therapeutic, and rehabilitative measures in order to maintain, restore or improve health outcomes of individuals and populations. Fellows will learn the principles of quality improvement including: o History and fundamentals of quality improvement o Health care process design, clinical outcomes, or waste/cost reduction Page | 8 o o o o o Quality measurement techniques, methodologies and research methods Strategic and Organizational Improvement Failure Modes and Effects Analysis Benchmarking Financial Data and Cost Analysis Reading Suggestions: The policy and quality articles in JAMA, NEJM, Annals of Internal Medicine, American Journal of Medical Quality, Physician Executive Journal, Joint Commission Journal on Quality and Patient Safety Required Reading List: Berwick, DM (1989) Continuous Improvement as an ideal in health care. NEJM, 320(1):53-56 Excerpts from: Godman, E (1996). A Study in Hospital Efficiency. Boston, MA: Reprinted by the Joint Commission on Accreditation of Healthcare Organizations, Oakbrook Terrace, IL. David Leonhardt. “Making health care better. “(2009, Nov. 8). The New York Times. 8 Nov. 2009 http://www.nytimes.com/2009/11/08/magazine/08Healthcare-t.html?pagewanted=all Kenney, C (2008). The Best Practice: How the New Quality Movement is Transforming Medicine. New York, NY: PublicAffairs. (Chapter1) Mathews, SC, Pronovost, PJ, Herzlinger, RE (2011) Focus on Quality: An Opportunity to Execute Health Care Reform. Am. J.Med Qual, 2011 May-Jun;26(3):239-40 American Hospital Association. Health Care Reform: Implementation Timeline. (May 2010). Retrieved from http://web.mhanet.com/userdocs/articles/Reform%20Ready/Reform_Timeline_FINAL_5-25-2010.pdf American Hospital Association. Legislative Advisory: Summary of the Most Significant Health Reform Changes Affecting Hopsitals and Other employers (May 11,2010) Retrieved from http://www.wsha.org/files/149/Hospitals-as-Employers-May2010.pdf Kaiser Family Foundation. Focus on Health Reform: Summary of New Health Reform Law. (March 26, 2010) Retrieved from http://www.kff.org/healthreform/upload/8061.pdf Iglehart, JK (2011) Implementing health care reform – an interview with HHS secretary Kathleen Sebelius. N Engl J Med. 2011; 364:297-299 Merlis, M (2010, July 27) Health Policy Brief: Accountable Care Organizations. Health Affairs. Berwick, DM, Nolan, TW, Whittington J (2008). The triple aim: care, health and cost. Health Affairs, 27(3):759-769. Lipshultz, AK, Fee, C, Schell, H, Campbell, L, Taylor, J, Sharpe, BA, Nguyen, J, & Gropper, MA (2008). Strategies for success: A PDSA analysis of three QI initiatives in critical care. Jt Comm J Qual Patient Saf. 34(8):435-444. Page | 9 Useful Links: Agency for Healthcare Research and Quality (AHRQ): www.ahrq.gov/ AHRQ Quality Measures Clearinghouse: http://qualitymeasures.ahrq.gov/ Centers for Medicare & Medicaid Services (CSM) Hospital Quality Initiatives: https://www.cms.gov/hospitalqualityinits/ CMS Physician Quality Reporting Initiative (PQRI): https://www.cms.gov/PQRS/ Institute for Healthcare Improvement: http://www.ihi.org Joint Commission Resources: http://www.jcrinc.com/ National Committee for Quality Assurance (NCQA): http://www.ncqa.org National Quality Forum: http://www.qualityforum.org/ Online Independent Learning: Institute for Healthcare Improvement Open School House Modules: IHI QI 101: Fundamentals of Improvement Serious errors occur at the best hospitals and clinics – despite the best efforts of talented and dedicated providers. As the Institute of Medicine (IOM) declared in 2001, in words that still ring true, “Between the health care we have and the care we could have lies not just a gap, but a chasm.” This course launches you on your journey to becoming a health care change agent. First, you’ll get a sense of the scope of the problem, from an up-close and personal look at a wrongsite surgery at a major academic hospital… to a high-level picture of the current quality of care in the US and around the world. Then you’ll begin to work on a solution to the problem, using the roadmap for change offered by the Institute of Medicine’s six aims for improvement – and a theory of how to change systems. Estimated Time of Completion: 1 hour 15 minutes IHI QI 102: The Model for Improvement: Your Engine for Change This course will teach you how to use the Model for Improvement to improve everything from your tennis game to your hospital’s infection rate. You’ll learn the basic steps in any improvement project: setting an aim, forming a team, selecting measures, developing ideas for changes, testing changes using Plan-Do-Study-Act (PDSA) cycles, and measuring to determine if the changes you are testing are leading to improvement. Estimated Time of Completion: 1 hour 30 minutes IHI QI 103: Measuring for Improvement Measurement is essential in any improvement work: It tells you if the changes you are testing are leading to improvement. But measurement for improvement is different from measurement for research. In this course, you’ll learn how to use three basic kinds of measures: outcome, process, and balancing measures. You’ll learn how to collect, display, and interpret data – to ensure that measurement accelerates the pace of change, rather than slowing it down. Page | 10 Estimated Time of Completion: 1 hour IHI QI 104: Putting It All Together The first three IHI Open School quality improvement courses introduced you to the fundamentals of improving health care. In this course, you’re going to see how people in real health care settings actually use these methodologies to improve care. You’ll start by learning the four phases of an improvement project's "life cycle": innovation, pilot, implementation, and spread. Next, you’ll delve deeper into the theory of spreading change – both the foundational work by sociologist Everett Rogers, and IHI’s Framework for Spread. This course presents two real case studies of organizations that actually used the methodologies you’re learning about to improve an important aspect of patient care. Estimated Time of Completion: 1 hour IHI QI 105: The Human Side of Quality Improvement If you want to improve a complex system, you’ll probably need to convince the people around you to do things differently. But a change that seems sensible and beneficial to you may feel threatening to others. In this course, you’ll learn why culture change is crucial to the success of many improvement projects. You’ll discover the most common reasons people resist change, and then you’ll practice responding in a way that mitigates that resistance. You’ll also learn how new ideas typically spread through a population, and what you can do to help different parts of the population adopt the change. Finally, you’ll learn different ways to motivate people – and which methods are likely to be most effective in a health care setting. Estimated Time of Completion: 1 hour 15 minutes IHI MHO 101: Achieving Breakthrough Quality, Access, and Affordability How does an organization go from providing ho-hum, average care to providing breakthrough quality, access, and affordability to patients? In this course, you’ll learn to apply a basic framework for designing, operating, and improving complex systems of care that can lead to rapid gains in performance. First, you’ll learn that while advances in technology have led to much better patient outcomes over the past few decades, they’ve also made for a much more complex health care system. That complexity makes it impossible to predict exactly how the system will perform dynamically, which in turn means that constant, broad-based innovation is absolutely required as staff members discover “weak signals” of system failure. Improving big clinical problems such as central line infections, you’ll learn, requires that staff members report tiny, apparently harmless problems as they occur – and it requires that senior leaders actually do something about those problems. By the end of this course, you’ll identify the “weak signals” of system failure all around you, and you’ll also figure out exactly what your organization needs in order to respond effectively. Estimated Time of Completion: 1 hour 45 minutes Page | 11 Effective Change Management Fellows will learn the principles of change management including: o Challenges of effective change in the health care setting and specific strategies for managing each of the challenges. o Best strategies for engaging caregivers in change, engaging front line staff, assuring leadership engagement, and identifying methods to assure effectiveness of change. o Conflict Management o Negotiation Theory o Teamwork and facilitation o Process and Outcomes Thinking o Change Concepts/Change Theory o Learning Cycles for Improvement Other Training opportunities Myers-Briggs Indicators Required Reading List: Berwick, DM (2002) User’s manual for the IOM’s ‘quality chasm’ report. Health Affairs, 21(3)80-90. Chassin, MR, & Becher, EC (2002). The Wrong Patient. Ann of Int. Med, 136(11):826-833. Pronovost, P, Berenholtsz, S, Dorman, T, et al (2003). Improving Communications in the ICU Using Daily Goals. J Crit Care, 18(2):71-75. Berenholtz, SM, Schumacher, K, Hayanga, AJ, et al (2009). Implementing standardized operating room briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf, 35(8):391-7. Berwick, DM (1996). Harvesting knowledge from improvement. JAMA, 275:877-878. Willingham, Robert L. How to Speak So People Will Listen. Waco, Tex.: Word Books, 1968. Fisher, Roger and William L. Ury with Bruce Patton, editor. Getting to Yes: Negotiating Agreement Without Giving In. Boston: Houghton Mifflin, c1991. Ury, William. Getting Past No: negotiating in difficult situations. New York: Bantam Books, 2007. Jones, Gareth R. Organizational Theory, Design, and Change (6th Edition). Upper Saddle River, N.J.: Prentice Hall, 2010 Page | 12 Online Independent Learning: Institute for Healthcare Improvement Open School House Modules: IHI L 101: So You Want to Be a Leader in Health Care When you think of a leader, what comes to mind? A president? A CEO? No matter what your position or formal title is, you can be a leader. In this course, you’ll zoom in on a hospital that’s having some trouble with infection control. As you grapple with this case, you’ll learn that leadership isn’t a position of authority—it’s an action. You’ll learn how to persuade different types of people and build enough unity to move forward. Finally, you’ll learn how to measure your effectiveness as a leader. Written reflections and discussions are key to this course—don’t skip them! Periodically you’ll be directed to a discussion board where you can post your answers and discuss them with other students. Estimated Time of Completion: 1 hour 30 minutes IHI PS 103: Teamwork and Communication No matter how safe we make the design of systems in which we work, there is no substitute for effective teamwork and communication. In this course, you’ll learn what makes an effective team. Through case studies from health care and elsewhere, you’ll analyze the effects of teamwork and communication on safety. You’ll learn essential communication tools, such as briefings, SBAR, and the use of critical language. Finally, you’ll learn how to use these tools when they are most essential—at transitions in care, when errors are most likely to occur. Estimated Time of Completion: 1 hour IHI QI 106: Level 100 Tools This practical course will teach you how to create and use three essential tools for improvement: PDSA (Plan-Do-StudyAct) templates, measurement planning forms, and run charts. Working through step-by-step tutorials that put you right in the middle of health care scenarios, you’ll learn how to plan a series of tests, collect data, graph your results, and interpret what your graph is trying to tell you. The course is fully hands-on, so get ready to practice new skills along the way. Note: You will need Microsoft Word and Excel (any version) to make the most of this course. Estimated Time of Completion: 3 hours Page | 13 Hospital Operations Fellows will learn the principles of hospital operations including: Core elements of quality program design, utilization, peer review Health Care as a System Health Information Technology Key interactions between quality and patient safety, medical staff leadership, hospital operations, and senior leadership. o Fundamentals of hospital administration o Effective practice dissemination o Change management o o o o Fellow will participate in the following committees: The Multidisciplinary Peer Review/Root Cause Analysis Committee Performance Improvement Committee Capacity Management Committee Fellow will shadow senior leadership: Dominick Stanzione, Executive Vice President & Chief Operating Officer Lillian Fraidkin, Senior Vice President & Chief of Staff Thomas Smith, Chief Nursing Officer & Senior Vice President Required Reading List: Bradley, EH, Holmboe, ES, Mattera, JA, Roumanis, SA, Radford, MJ, Krumholz, HM (2003). The roles of senior management in quality improvement efforts: what are the key components? J Healthc Manag, 48(1):15-28; discussion 29. Keroack, MA, Youngberg, BJ, Cerese, J L, Krsek, C, Prellwitz, LW (2007). Organizational factors associated with high performance in quality and safety in academic medical centers. Acad Med, 82(12):1178-86. Berwick, D, Enthoven, A, & Bunker, J (1992) Quality Management in the NHS: The doctor’s role-I/11. British Med Jnl, 304 ;235-239; 304-308. Englebright, J, Perlin J (2008) The chief nurse executive role in large healthcare systems. Nurs Adm Q, 32(3):188-94. Wharam, JF, & Sulmasy, D (2009). Improving the quality of health care: Who is responsible for what? JAMA, 301(2):215217. Conway, J (2008) Getting boards on board: engaging governing boards in quality and safety. Joint Comm Jnl on Qual and Pat Saf, 34(4):214-220 Page | 14 Inozu, Bahandir and Dan Chauncey, Vickie Kamataris and Charles Mount. Performance Improvement for Healthcare: Leading Change with Lean, Six Sigma, and Constraints Management. New York, McGraw-Hill Companies, 2011. Opportunities to interact with local leading patient safety organizations such as Institute for Healthcare Improvement IHI Patient Safety 23rd Annual National Forum (December) AHRQ Annual Conference Focuses on Innovation and Collaboration in Health Care (September) Opportunities to interact with senior leadership and be involved with patient safety initiatives: Performance Improvement Committee Multidisciplinary Peer Review/Root Cause Analysis Committee Capacity Management Page | 15 Key Institutional Resources Institutional Champions: Dr. Davidson Clinical Leader: Program Director/Chair from core training program Administrative Leader: Department specific Main Faculty Dr. Patrick Borgen Dr. David Cohen Nancy Daurio, RN Dr. Steven Davidson Lillian Fraidkin, RN Susan Goldberg, RN Elaine Gunn Dr. Loren Harris Dr. Samuel Kopel Dr. John Marshall Dr. Howard Minkoff Barbara Sommer Dominick Stanzione Thomas Smith Adjunct Faculty Peter Homel Page | 16 Biostatistician Committee Schedules The Multidisciplinary Peer Review/Root Cause Analysis Committee is scheduled every Friday 8:30a - 10:30a in the Boardroom Performance Improvement Committee is scheduled for every 3rd Monday 8:00a - 10:00a in the Boardroom Capacity Management Committee is scheduled for 2nd and the 4th Monday 3:30-4:30 in the Boardroom with exceptions, see below: Capacity Management Meeting Schedule for 2012 1/9 – 3:30p (Board Room) 1/23 – 3p (Admin. Bld, Room 2C) 2/13 - 3:30p (Board Room) 2/27 – 3:30p (Board Room) 3/12 – 3p (Admin. Bld, Room 2C) 3/26 – 3:30p (Board Room) 4/9 – 3:30p (Board Room) 4/23 – 3:30p (Board Room)) 5/14 – 3p (Admin. Bld, Room 2C) 5/28 – 3:30 (Board Room) 6/11 – 3:30p (Board Room) 6/25 – 3:30p (Board Room) 7/9 – 3:30p (Board Room) 7/23 – 3:30 (Board Room) 8/13 – 3:30p (Board Room) 8/27 – 3:30 (Board Room) 9/24 – 3:30p (Board Room) 9/10 – 3:30p (Board Room) 10/8 – 3:30p (Board Room) 10/22 – 3:30p (Board Room) 11/12 – 3:30p (Board Room) 11/26 – 3:30p (Board Room) 12/10 – 3:30p (Board Room) 12/24 – 3:30p (Board Room) Page | 17 Maimonides Medical Center Joint Quality Project Fellowship Application Form PERSONAL DATA Name (first, middle, last): _______________________________________________________ First, Middle, Last Permanent address: ___________________________________________________________ ____________________________________________________________________________ Mailing address (if different): _____________________________________________________ ____________________________________________________________________________ Telephone: (home) ___________________________ (cell) ____________________________ Fax: ____________________________ E-mail: _____________________________________ Professional Degree: ______________ Gender: ____Male ____Female Date of Birth: ________________________________ Month/Day/Year FELLOWSHIP QUALIFICATIONS Do you have an MD or DO? ____Yes Page | 18 ____No If you are a graduate of a foreign medical school (except Canada), you are required to be certified by the Educational Council for Foreign Medical Graduates. If you are certified, indicate below and provide a copy with this application. Date of Certificate _________________________Number _______________________ Have you completed housestaff training in a primary specialty? ____Yes ____No If yes, name of primary specialty completed: ________________________________________ Medical License # _____________________________, _____________________________ State Board certified? ____Yes Board eligible? ____Yes ____No ____No Are you a citizen of the United States or have permanent resident status? ____Yes ____No If not, Visa status: ____________________________________________________________ Please have 2 recommendation letters sent directly to the Joint Quality Project Fellowship Steering Committee at the street or e-mail address below. One letter must be from your current Program Director or Supervisor. Please list their names, positions, institutions, address, telephone and email here: Name/Position/Institution: _______________________________________________________ Address: ____________________________________________________________________ Phone: _____________________________________________________________________ Page | 19 E-mail: _____________________________________________________________________ Name/Position/Institution: _______________________________________________________ Address: ____________________________________________________________________ Phone: _____________________________________________________________________ E-mail: _____________________________________________________________________ Robin Gitman, MBA, MPH Associate Vice President/DIO Joint Quality Project Fellowship Academic Affairs Maimonides Medical Center 4802 10th Avenue Brooklyn, NY 11219 rgitman@maimonidesmed.org 718-283-8245/phone 718-283-8239/fax Page | 20 BACKGROUND INFORMATION Have your privileges at any hospital or other facility ever been denied, limited, suspended, revoked, or not renewed? And/or have you ever been denied membership or renewal therein or been subjected to disciplinary proceedings in any hospital or medical organization? Yes No If yes, please give full details on a separate sheet. Has your license to practice medicine in any jurisdiction ever been limited, suspended, or revoked? Yes No If yes, please give full details on a separate sheet. Have you ever voluntarily relinquished your license? Yes Page | 21 No If yes, please give full details on a separate sheet. PLEASE ENCLOSE: 1. Curriculum vitae 2. Personal statement of no more than two pages explaining why the applicant wants to pursue this opportunity and describing the professional and personal goals that will be met by completing this program, along with any additional information that may be helpful to the Joint Quality Project Fellowship Steering Committee. 3. Type of clinical work desired during fellowship: ___________________________________ ____________________________________________________________________________ SIGNATURE: ___________________________________ DATE: __________________ Application Deadline: 3/15/2012 for July 2012 entry. Send completed application form, CV, and personal statement to the address below. Please have your medical school forward transcripts directly to us as below. Robin Gitman, MBA, MPH Associate Vice President/DIO Joint Quality Project Fellowship Academic Affairs Maimonides Medical Center 4802 10th Avenue Brooklyn, NY 11219 rgitman@maimonidesmed.org 718-283-8245/phone 718-283-8239/fax Page | 22