pubdoc_3_9596_1660
advertisement

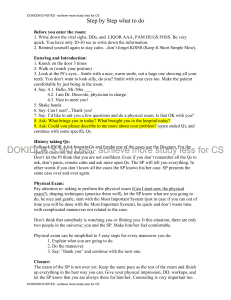
History taking Department of Internal Medicine College of medicine/ Babylon University Third year At the beginning, the student need to gather the following information Patient’s name/ age/ sex/ religion/ occupation/ home address/ marital status/ date of admission/ date of history taking Chief complaint and duration: please mention here the main problem(s) that made the patient seeks the medical advice and the duration of this(ese) compliant(s). It is preferable to mention one chief complaint. Record patient’s words and don’t mention medical jargons for example say shortness of breath and not dyspnea, loose bowel or frequent bowel motions rather than diarrhea. History of presenting illness: In this section, the student needs to tell the story of patient’s compliant in a way that helps to narrow the differential diagnosis of the underlying cause. For example, when the chief complaint is pain (anywhere) the history of presenting illness should answer the following questions SOCRATESSite, Onset (sudden or gradual), Character, Radiation, Associated symptoms (like nausea and vomiting), Timing/ Duration and frequency, Exacerbating and relieving factors, Severity. If the chief complaint (the pain) is related to the cardiovascular system for example, all questions of systemic review that are related to that system should be answered here. The student need to mention any investigation/ procedure(s) has been done and treatment prescribed to the patient during this hospital admission. The change in patient’s condition whether for better or worse need to be explored and documented. 1 Review of other systems: Question of some of important chief complaints will be listed within the systemic review of each system. General questions: Energy Appetite Sleep If there is any weight loss (ask about the ring size, fitness of the clothes), significant weight loss is about 10% of the original weight in the last 3 months. Fever Questions about fever: o Sudden or gradual o Duration, o Continuous or intermittent (occurs every day, every other day or every third day) o Is there any specific time of it (day or night) o Associated with rigor or sweating (ask about the time of sweating and its amount) o Ask about other symptoms like abdominal pain, nausea and vomiting, diarrhea, chest pain, cough , hemoptysis, lion pain….etc. Cardiovascular system: Chest pain (ask questions of pain) Palpitation o onset, duration, frequency o rapid or slow, regular or not o aggravating factors like coffee or alcohol drinking, certain medication, exercise or chest infection o terminated spontaneously or with medication o associated symptoms like syncope dizziness chest pain or polyuria (feature of supraventricular tachycardia). 2 o Is there any history of structural heart disease or valvular heart disease (you can mention these information in the past medical history) Shortness of breath o Onset and duration o severity o Aggravating factor(s) lying flat, After how long? with exercise? After how many meters? cold weather, dust or smoke? o How many pillow you need at night o Relieving factor(s) o Associated features like fever, cough, wheeze, weight gain or loss. Paroxysmal nocturnal dyspnea: is sudden breathlessness which wakes the patient from sleep chocking or gasping for air Orthopnea: is dyspnea on lying flat and is a sign of advanced heart failure Intermittent claudication: is pain felt in the legs on walking due to arterial insufficiency. Cyanosis: is bluish discoloration of skin and mucous membrane, occurs when absolute concentration of deoxygenated hemoglobin > 50 g/l. o Central cyanosis: seen at the tongue and lips o Peripheral cyanosis: seen in hands, feet and ears Syncope/ pre-syncope: loss of consciousness due to inadequate cerebral perfusion. Leg swelling Respiratory system: Cough o Duration (acute less than 3 weeks/ sub-acute from 3 to 8 weeks/ chronic more than 8 weeks) and frequency o Is there any particular time of day when the cough is the worst (nocturnal cough means asthma, gastro esophageal reflex disease (GERD) and left ventricular failure while early morning cough occurs in chronic bronchitis) o Aggravating factors like dust, animals, deodorant, cold weather, exercise or cigarette smoke in asthma/ eating and like lying flat in GERD 3 o Is it progressive o Is there any seasonal variation o Painful or not o Productive or not Sputum o Color Serous: acute pulmonary edema Mucoid: chronic bronchitis/ asthma Purulent: yellow: acute Broncho pulmonary infection and asthma Green: bronchiectasis and lung abscess Rusty: pneumococcal pneumonia o Amount: large amount is seen in bronchiectasis, broncho-pleural fistula o Smell : foul smell indicates bronchiectasis and lung abscess Hemoptysis o Onset, duration and frequency o Amount o Frank blood or streaks the sputum Shortness of breath Chest pain cyanosis Wheeze: is a high pitched whistling sound caused by air passing through narrowed small airways, occur during the expiration Strider: inspiratory musical sound due to upper airway narrowing. Hoarseness of voice Nasal symptoms like rhinorrhea Gastrointestinal system: Painful mouth/ water brush or dry mouth/ halitosis Dysphagia o Onset and duration o Where is the site of dysphagia is it at the pharynx or retrosternal (in the esophagus o Painful or not? o For solid or liquid or both? 4 o Progressive or intermittent? o Is there any heart burn or regurgitation Nausea or vomiting o For how long? How many times the patient vomited? What is the amount? o Does it related to the meal? At early morning? At night? o Does the vomiting associated with nausea, abdominal pain or dyspepsia? Does that pain relieved by vomiting o Is it projectile? o Is the vomitus stained with bile, blood or feculent? dyspepsia Hematemesis o Is there any previous history of hematemesis or peptic ulcer diseases? o Is there any history of smoking, non-steroidal anti-inflammatory drugs (NSAID), steroids or alcohol ingestion? o Is there any history of liver disease? o Does the hematemesis preceded by retching? Does the blood appeared in the very first vomit o How many times? What is the amount of blood? Was it fresh or coffee ground? o What is the color of the stool? Abdominal pain/ abdominal distension Jaundice o Sudden or gradual?/ recurrent or not? o Any right upper quadrant pain or abdominal pain elsewhere? o Is there any fever? o Itching/ ecchymosis/ change in urine or stool color? o Is there any travel history or contact with jaundiced patient (hepatitis A)/ blood transfusion, previous operation, Intravenous drug addiction or tattooing (hepatitis B and C)? o Is there any family history of hemolytic anemia (hereditary spherocytosis) o Is there any sexual contact outside the marriage (if the patient is married)? Diarrhea (ask about change in bowel habits) o Acute, chronic or intermittent? o Is the stool liquid or semisolid? 5 o Is it infrequent with large volume (small intestine) or frequent with small volume (large intestine) o Does it associated with fever? Does it affect patient’s sleep? (to differentiate the organic from functional diarrhea) o Is there any blood, pus or mucous with the stool? o Is there any tenesmus, urgency or incontinence o Ask about drug history Constipation( ask about change in bowel habits) Melena/ rectal bleeding Melena is passing tarry (shiny black) stool with characteristic odor, caused by upper gastrointestinal tract bleeding. o Is the blood mixed with stool or just streaking? o Is it painful? o Is it offensive or not? o Does it associated with hematemesis? Tenesmus Flatulence Genitourinary system: Loin pain/ suprapubic pain Polyuria: is defined as a urine volume exceeds 3 liters per day caused by diabetes mellitus ,diabetes insipidus…etc Oliguria: is defined as being present when less than 500 ml urine is passed per day Anuria: is defined as passing less than 50 ml urine per day usually reflect urinary tract obstruction Frequency: is micturition more often than patient’s expectations Urgency Incontinency (stress?/ urge?): involuntary leakage of urine Nocturia: is defined as waking at night to void urine Hematuria: presence of blood in the urine, microscopic (detected on urinalysis) or macroscopic can be seen by naked eye Burning micturition (dysuria) Hesitancy: 6 Poor stream Post-micturition dribbling Urethral discharge Central nervous system: Headache: in addition to general questions of pain, in case of headache you need to ask these extra question: o Is it the first episode of headache or have there been previous episodes? o If it is a recurrent problem, are all the episodes of similar type? quality? or severity? o Is the pain unilateral or bilateral? o Is the headache disabling or not? Is it affecting the sleep or lifestyle of the patient? o Associated features: is it associated with fever, neck pain, loss of consciousness, abnormal movements, limb weakness, scalp pain or any visual symptoms? o Does it change with changing position? it get worse on wakening or lying down/ associated with vomiting (features of increased intracranial pressure)? Loss of consciousness/ disturbed consciousness Vertigo: a false sense of movement of oneself or the environment; very important to ask about associated unsteadiness, tremor, hearing impairment, ear pain or specific precipitation by head movement. Any weakness Any paraesthesia ( feeling of pins and needles or crawling sensation) Fit/ seizure (mostly the history is taken from a witness and the patient) o Is it the first time? o What happened before the episode? (pre-ictal) What are the aggravating factors like sleep deprivation, fatigue or alcohol withdrawal? Any abnormal feeling(s) preceded the fit like epigastric pain, funny smelling sensation?(this is called aura)? o What happened during the abnormal episode? (ictal) what is the description of that episode? Any loss of consciousness? 7 Any abnormal movement? which part of the body is involved ? For how long the convulsion continued? Any change in patient’s color (cyanosis)?/ any involuntary urination or defecation? Has there been any tongue bite or injury? o What happened after the event (post-ictal)? Any associated features like headache, fever, memory disturbance, limb weakness or paresthesia? Abnormal speech Abnormal movement o Tremor (unilateral or bilateral? at rest or when you stretch your hand? is it progressive or no? does it involve the head and tongue or not? Dance-like movement (chorea) Change in behavior Loss of memory Change in vision/ taste/ hearing Bladder, bowel and functional disturbances Gait/ balance Musculoskeletal system Arthralgia: joint pain Myalgia: muscle pain Bone pain Joint swelling Limitation of joint movement Muscle weakness (proximal, distal or generalized) Gait disturbance Past medical history (ask about): How many times the patient was admitted to the hospital? What was the cause of the admission? Which hospital? What kind of investigations were done for the patient? Were there any complications? 8 Ask specifically about important illnesses like: Hypertension, diabetes mellitus, tuberculosis, asthma, chronic obstructive airway disease, ischemic heart disease , stroke ……etc If the patient has a history of chronic disease, the student need to ask the following questions about that disease o Since when you have this disease and the answer is for example since 2010? How did you discover it? o On what treatment you are now and to which extent it is effective (controlling your symptoms)?. Past surgical history: Ask about any surgical operation (was it major or minor) might be done for the patient?/ in which hospital and who was the surgeon?/ what was the kind of anesthesia (local or generalized)?/ how long the patient stayed in the hospital after the procedure?/ were there any complications? Ask about any procedures done for the patient like esophageo-gastroscopy, colonoscopy and coronary angiogram or intervention? Ask about any history of biopsy taking like liver or kidney biopsy. Gynecological and obstetric history: Number of pregnancies and what was the outlet/ were there any complications like hypertension, proteinuria or pregnancy induced hyperglycemia? Number of deliveries/was it at home or in the hospital (which hospital)/ was it normal vaginal delivery or caesarean section/ was there any complications of the caesarean section Number of still birth/ number of abortions Menstrual history: Menarche: the age when the period starts Frequency, regular or irregular How many days does it last? 9 What is the amount of blood, heavy or not? Is there any clots? Oligomenorrhea : period occurs in intervals longer than 35 days and/or being particularly light (with little amount of blood) Menorrhagia (heavy menstrual bleeding) Dysmenorrhea: pain prior or during the period Amenorrhea o Primary amenorrhea: no period at all by the age of 16 years o Secondary: no period for 3 months or more in a woman who previously menstruated regularly Menopause: the final spontaneous menstrual period Postmenopausal bleeding: spontaneous menstrual bleeding one year after the menopause Treatment history: Any treatment for chronic diseases. The student needs to mention the type of medication, the dose, for how long the patient is on this medication and any possible side effects. Compliance with the prescribed medication Any drug allergy Any history of blood (or blood products) transfusion and for what reason, how many pints, was there any complications? Ask about any radiotherapy or radiation exposure. Personal ,Family and Social history: Ask about: Marital status Number of children (males and females) Patient’s job and the income (sufficient or not?) 10 Smoking/ packs per year = (number of cigarettes smoked in one day/20) × number of years/ for example if the patient smokes 10 cigarettes per day for 10 years, the packs per year for that patient are 5 Alcohol intake/ amount Pets and domestic animals Live in urban or rural area? Home/ how many rooms/ how many persons are living there/ is the house crowded or not? Water supply (tap water, well, river water)? Ask about the father and the mother (are they alive? how old are they?/ if they are dead, ask at which age they died any why? Ask about brothers and sisters Is there any inherited disease in the family/ is there any history of sudden death in the family especially at young age? If there is any similar illness running in the family, think about inherited or infectious disease. اعداد فرع الطب الباطني ا د عالء حسين م د محمد حسن 11 م د يسار فالح م م د براق حيدر