S mansoni
advertisement
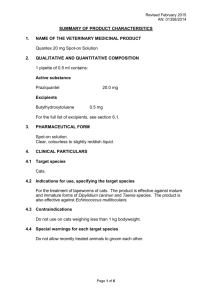
Drugs Used in Treatment of Schistosomiasis • • • • • • • Schistosomiasis is is a parasitic disease caused by several species of trematode flatworms of the genus Schistosoma (blood flukes).Most of human infections are caused by: -Schistosoma mansoni cause intestinal schistosomiasis -Schistosoma haematobium causes urinary schistosomiasis -Schistosoma japonicum cause Asian intestinal schistosomiasis The diseases also known as bilharzia, bilharziosis or snail fever named after discovery by after Theodor Bilharz, who first described the cause of urinary schistosomiasis in 1851. In terms of impact this disease is second only to malaria as the most devastating parasitic disease. Although it has a low mortality rate, schistosomiasis often is a chronic illness associated with massive illness that can damage of the internal organs and, in children, impair growth and cognitive development. In urinary schistosomiasis, there is progressive damage to the bladder, ureters and kidneys with increased risks for bladder cancer . In intestinal schistosomiasis, there is progressive enlargement of the liver and spleen, intestinal damage, and hypertension of the abdominal blood vessels with increased risks for liver cirrhosis, liver and/or rectal cancer . The disease is endemic in ~74 developing countries, infecting more than 200 million people, in Africa, the Caribbean, eastern South America, Southeast Asia and in the Middle East. About 20 million suffer severe consequences from the disease worldwide with ~ 200,000800,000 deaths/year. • • • • • • The adult worms of both sexes live and mate in the portal circulation (veins or venules )of the liver, gut wall or the bladder where they feed on red blood cells and cause massive tissue destruction. Schistosomes have a typical trematode vertebrate-invertebrate lifecycle, with humans being the definitive host. In certain developmental stages of its life cycle, the parasite live in certain types of freshwater snails that being the intermediate host. Biomphalaria sp., the intermediate host for S. mansoni, Bulinus sp., the intermediate host for S. haematobium , and Oncomelania sp. the intermediate host for S. japonicum Human contact with water is thus necessary for infection by schistosomes. Eggs are eliminated with feces or urine of infected individual into fresh water bodies. Under optimal conditions the eggs hatch and release miracidium , which swim and penetrate specific snail intermediate hosts . The stages in the snail include 2 generations of sporocyst and the production of cercariae. Upon release from the snail, the infective cercariae swim, penetrate the skin of the human host , and shed their tail. As the cercaria penetrates the skin it transforms into a migrating schistosomulum stage. • • • • • • The newly transformed schistosomulum may remain in the skin tissues for 2 days before locating a post-capillary venule; from here the schistosomulum travels to the lungs where it undergoes further developmental changes to the liver. 8-10 days after penetration of the skin, the parasite migrates to the liver sinusoids. worms develop an oral sucker after arriving at the liver, and it is during this period that the parasite begins to feed on red blood cells (cause of anemia). The nearly-mature worms pair, with the longer female worm residing in the gynaecophoric channel of the shorter male. Adult worms in humans migrate to mesenteric venules in various locations, which at times seem to be specific for each species . Worm pairs of S. mansoni and S. japonicum reside in the mesenteric or rectal veins. S. haematobium ultimately migrate from the liver to the perivesical venules of the bladder, ureters, and kidneys and can be also found in the hemorrhoidal venules. Parasites reach maturity in six to eight weeks, at which time they begin to produce eggs(300-3000 egg/day). Many of the eggs pass through the walls of the blood vessels, and through the intestinal wall (S. mansoni and S. japonicum) , andthrough the ureteral or bladder wall (S. are eliminated with feces or urine, respectively . • • Up to half the eggs released by the worm pairs become trapped in the mesenteric veins, or will be washed back into the liver, where they will become lodged. Worm pairs can live in the body for an average of 4.5 years, but may persist up to 20 years. Trapped eggs mature normally, secreting antigens that elicit a vigorous immune response. Pathogenesis: • The eggs themselves do not damage the body. Rather it is the cellular infiltration resultant from the immune response that causes the pathology classically associated with schistosomiasis. • • • • Schistosomiasis is a chronic disease symptomatic, with anemia, malnutrition, retarded growth, abdominal destension and cognetive impairment being common in endemic areas. Acute schistosomiasis may occur weeks after the initial infection, especially by S. mansoni and S. japonicum include (Katayama's fever) that is manifested as (generalized weakness, fever, abdominal pain, cough, diarrhea, and eosinophilia). By continous infection many inflammatory reactions occur leading to granulomatous and fibrotic changes in the affected organs like colonic polyposis with bloody diarrhea, pulmonary hypertension and portal hypertension (ascites, and varicosity; esophageal ,hemorrhoid , and umbilicus) with hematemesis Pathology of S. haematobium include most of katayama’s fever symptoms in addition to cystitis, glomerulonephritis, and ureteritis with hematuria, which can progress to bladder cancer. Skin symptoms: At the start of infection, mild itching and a papular dermatitis of the feet and other parts after swimming in polluted streams containing cercariae. Treatment of schistosomiasis: • • • • In addition to pharmacological interventions used to eradicate the infection , prevention of disease spreding is also utilized which is best accomplished by eliminating the water-dwelling snails that are the natural reservoir of the disease. Many chemicals like acrolein, copper sulfate and niclosamide in addition to other natural and ecological interventions like crayfish populations, sarcoca plant, and gopo berry can be used for this purpose. There are ongoing and extensive researchs into developing a schistosomiasis vaccine that will prevent the parasite from completing its life cycle in humans. Some antigenic structures of the parasite like paramyosin and Sm14 have been proposed as a vaccine candidate. Drugs like praziquantel , artemisinin and its derivatives, metrifonate, and oxamniquine utilized to treat different types of schistosomiasis (1)Praziquantel • • Praziquantel is a synthetic isoquinoline-pyrazine derivative that is highly effective broad-spectrum antihelminthic drug.It is considered the agent of choice for the treatment of all forms of schistosomiasis in addition to many other trematode and cestode infections. The drug does not only affect the adult schistosomes but also the immature forms and it has a prophylactic effect against cercarial infection. Mechanism of action: • • • It works by increasing the parasitic cell membrane permeability to Ca2+, causing contracture and paralysis of the parasite. The drug apparently disrupts Ca2+ homeostasis in the parasite by binding to the PKC-binding sites in a β subunit of schistosome voltage-gated Ca2+ channels. This induces an influx of the ion, a rapid and prolonged contraction of the musculature, and eventual paralysis and death of the worm. The dying parasites are dislodged from their site of action in the host organism and may enter systemic circulation or may be destroyed by host immune reaction (phagocytosis). Praziquantel also interfere with adenosine uptake and make the parasitic worm is unable to synthesize purines that interfere with nucleic acid synthesis. Pharmacokinetics: • • • • • Praziquantel tablets are taken with liquid after a meal. The dosage is 20 mg/kg per dose for two (S mansoni and S haematobium) or three (S japonicum ) doses at intervals of 4–6 hours. It is rapidly absorbed, with a bioavailability of about 80% after oral administration. Peak serum concentrations are reached 1–3 hours after a therapeutic dose. Cerebrospinal fluid concentrations of praziquantel reach 14–20% of the drug's plasma concentration. About 80% of the drug is bound to plasma proteins. Most of the drug is rapidly metabolized to inactive mono- and polyhydroxylated products after a first pass in the liver. The half-life is 0.8–1.5 hours. Excretion is mainly via the kidneys (60–80%) and bile (15–35%). Plasma concentrations of praziquantel increase when the drug is taken with a high-carbohydrate meal . Praziquantel is metabolized by CYP3A4. Agents that induce CYP3A4 such as phenytoin, carbamazipine, ifampin, corticosteroidsand azole antifungals will affect the metabolism and reduce the bioavailability of praziquantel. • Enzyme inhibitors like cimetidine causes increased praziquantel levels Adverse effects: Praziquantel is considered to be a very safe drug with minimal side effects in therapeutic dosage. Side effects include GI disturbance, dizziness, aching in muscles and joints, skin rashes and low-grade fever. Some effects are more marked in patients with a heavy worm load and may be caused by products released from the dead worms. The safety of praziquantel in children younger than age 4 years is not established, but no specific problems in young children have been documented. Indeed, the drug appears to be better tolerated in children as in adults. Praziquantel increased abortion rates in rats and therefore should be avoided in pregnancy if possible. Because the drug induces dizziness and drowsiness, patients should not drive during therapy and should be warned regarding activities requiring particular physical coordination or alertness. Some resistance has developed to the drug (especially with S mansoni infections). (2) Metrifonate • Metrifonate is an an organophosphate compound acts as safe alternative therapy for the treatment of S. haematobium infections. It is not active against S mansoni or S japonicum. Mechanism of action: • It acts as irreversible acetylcholinesterase inhibitor that temporarily paralyzes the adult worms, resulting in their shift from the bladder venous plexus to small arterioles of the lungs, where they are trapped, encased by the immune system, and die. The drug is not effective against S. haematobium eggs; live eggs continue to pass in the urine for several months after all adult worms have been killed. • It has been used in mass treatment programs. In mixed infections with S haematobium and S mansoni, metrifonate has been successfully combined with oxamniquine. Pharmacokinetics: • • • Metrifonate is given in oral dose of 7.5–10 mg/kg is given three times at 14-day intervals for treatment of S. haematobium infestation. It was also effective as a prophylactic agent when given monthly to children in a highly endemic area. is rapidly absorbed from GIT. T he peak blood levels are reached in 1–2 hours; the half-life is about 1.5 hours. Clearance appears to be through nonenzymatic transformation to dichlorvos, its active metabolite. Metrifonate and dichlorvos are well distributed to the tissues and are completely eliminated in 24–48 hours. Adverse effects: Transient cholinergic symptoms may be experienced , including nausea and vomiting, diarrhea, abdominal pain, bronchospasm, headache, sweating, fatigue, weakness, dizziness, and vertigo. These symptoms may begin within 60 minutes and persist up to 12 hours. Metrifonate should not be used after recent exposure to insecticides or chlinomimetic drugs that might potentiate cholinesterase inhibition. Metrifonate is contraindicated in pregnancy. (3) Oxamniquine Oxamniquine is a tetrahydroquinoline acts as alternative to praziquantel (especially in instances of praziquantel resistance) for the treatment of S. mansoni infections. It has also been used extensively for mass treatment. It is not effective against S haematobium or S japonicum. Mechanism of action: • It acts by DNA binding resulting in Contraction and paralysis of the worms and eventual detachment from terminal venules in the mesentery and transit to the liver, where many die; surviving females return to the mesenteric vessels but cease to lay eggs. Pharmacokinetics: • • • • Oxamniquine is a potent single-dose agent that given orally. Optimal dosage schedules vary for different regions of the world. In the Western Hemisphere and western Africa, the adult oxamniquine dosage is 12–15 mg/kg given once. In northern and southern Africa, standard schedules are 15 mg/kg twice daily for 2 days. In eastern Africa and the Arabian peninsula, standard dosage is 15–20 mg/kg twice in 1 day. In mixed schistosome infections, oxamniquine has been successfully used in combination with metrifonate. It is readily absorbed from GIT; it should be taken with food (mild GI irritation). Its plasma half-life is about 2.5 hours. The drug is extensively metabolized by liver to inactive metabolites (principally the 6-carboxy derivative,70%, and 2-carboxy metabolite, 10-20%) both are excreted in the urine—up to 75% of the initial dose in the first 24 hours. Adverse effects: • It is generally well tolerated following oral doses. Some CNS symptoms(dizziness with or without drowsiness and headach) and GI effects (as nausea, vomiting, and diarrhoea) may occurs in at least 1/3 of patients, beginning up to 3 hours after a dose and usually lasting for up to 6 hours. • • • • Infrequent adverse effects are allergic symptoms ( low-grade fever, urticaria and skin rashes), elevated values of liver enzyme and proteinurea have been transiently reported in some patients. An orange to red discoloration of the urine, and a transient decrease in leukocytes.Mild hallucinations and seizures have been reported (especially in patients with a history of convulsive disorders and epilepsy). Since the drug makes many patients dizzy or drowsy, it should be used with caution in patients whose work or activity requires mental alertness (e.g. driving ). Drug is contraindicated in pregnancy