Module #8 – Endocrine Emergencies
advertisement

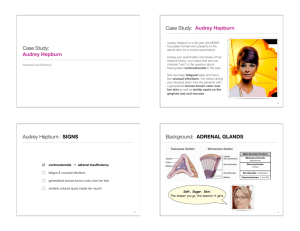
Learner Version Module #8 – Endocrine Emergencies Objectives: on facilitator version References: on facilitator version CASE A 74 yom with past medical history of oxygen dependent COPD presents to the ER with fatigue, sob and productive cough present for three days. His outpatient medications are atrovent and albuterol MDIs and nebulizers. He has had four hospitalizations in the past year for COPD exacerbations. On review of systems, patient reports that he has lost ~15 lbs over the past 6 mos. On physical examination, temperature 99.0 F, BP 88/52, HR 114 (after Duoneb was given), RR 20 with O2 sat 88% while on 4L of oxygen. Weight is 115 lbs, BMI 21. Physical examination is significant for a thin man with globally diminished breath sounds without any crackles or wheezing. He is breathing with pursed lips with contraction of accessory respiratory muscles. Remainder of the exam is normal. Labs: Na 131, K 4.0, Cl 92, CO2 40, BUN 6, Cr 0.4, Glu 55 WBC 12.1 (42% N, 46%L, 4%M, 6%E), Hgb 13m Hct 40, Plt 225 Lactate wnl, Coags wnl, LFTs wnl, trop wnl Imaging: PA/LAT CXR reveals no evidence of infiltrate or nodules. There is flattening of the diaphragms bilaterally. Hospital Course: A diagnosis of COPD exacerbation is made. The patient is admitted to the hospital and started on atrovent and albuterol nebs Q6H, doxycycline, and prednisone 60mg taper. His breathing and oxygenation improves over the course of 3 days. What is your differential diagnosis for his weight loss? What lab values are abnormal and not explained by COPD exacerbation? What diagnosis would explain the weight loss, hypotension and the abnormal lab findings? Would you suspect this to be primary, secondary or relative adrenal insufficiency? How would you work it up? How do you perform Cosyntropin stimulation test? How is the interpretation of the results of cosyntropin stim test different in critically-ill patients vs non-critically ill patients? What is the value of random cortisol level? Results of Cosyntropin stimulation test are as follows: Baseline: ACTH 5 (normal 10-65) Cortisol 16 ug/dl 30-minute stimulated cortisol: 22 ug/dl 60-minute stimulated cortisol: 26 ug/dl How do you interpret these values? Does the patient have adrenal insufficiency? What should you do now? Patient is seen by Endocrinology as outpatient and cosyntropin stim test is repeated, off prednisone. Results are as follows: Baseline cortisol: 10 ug/dl 60-minutes stimulated cortisol: 16 ug/dl Does the patient have adrenal insufficiency? How would you treat this patient now? Does this patient need fludrocortisone? Over the next 2 months, patient reports increased energy and weight gain of 3 lbs. He is seen in the Pulmonary Clinic for a follow-up of his recurrent COPD exacerbations (5 episodes in one year) and is started on Prednisone 10mg daily for his COPD. What should you do with the hydrocortisone? The patient is readmitted to the hospital 1 year later for RLL pneumonia. He is febrile, tachycardic, hypotensive, and requires 40% ventimask to maintain his oxygen saturation. The patient is diagnosed with community-acquired pneumonia and started on appropriate antibiotics. What would you do with his outpatient prednisone? When would you taper the stress dose steroids in this patient? Will the patient need steroids for life for his secondary adrenal insufficiency? MKSAP 16: Question #25: Management of adrenal insufficiency Question #39: Manage newly diagnosed adrenal insufficiency Question #48: Evaluate adrenal function during critical illness Question #55: Manage adrenal function during critical illness Question # 60: Diagnose the cause of acute adrenal insufficiency *****YOU MAY STOP HERE OR PROCEED TO NEXT CASE***** CASE A 19 yom was involved in a low speed motor vehicle accident. At the scene, he complained of neck pain. A C-collar was placed and he was transferred by ambulance to the local Emergency room. On exam, he was generally anxious, warm to touch, had mild tremor. Vitals show patient was tachycardic with heart rate of 125. Patient had tenderness over the c-spine, but no focal neurological deficits were noted. X-ray of the c-spine was ordered. Over the course of his ER stay he became progressively agitated, confused and combative. His heart rate increased to 160 and temperature rose to 40◦ C. He was visibly shaking and unable to sit still. He required sedation and restraints. He was intubated for airway protection and respiratory support and was transferred to a tertiary care center and admitted to an ICU bed. What is your differential diagnosis for his deterioration in mental status (initially anxious and mildly tremulous to agitation, confusion and combativeness) and increase in heart rate and temperature? What is your next step in the work-up and management? Patient received IV fluids with no improvement in his heart rate. His labs were all WNL, white count wnl, no toxic granulation, no left shift. Tox screen was negative. UA was negative and blood culture was drawn, thyroid panel pending. EKG showed sinus tachycardia, CXR was negative, C-spine x-ray was difficult to interpret so a C-spine CT was ordered, head CT was negative. Patient remained tachycardic at 160 and febrile to 41◦C, BP 160/90, with no obvious source of infection identified. What is the most likely diagnosis now? What are the clinical manifestations of thyroid storm? What would you look for in history if thyroid storm was suspected? What would you look for in physical exam if thyroid storm was suspected? What is the mortality rate for this condition? How would you treat this patient? Where do these pharmacologic agents work? Patient received: Propranolol 60 mg iv q 6 hours, PTU 150 mg po q 6 hours, Dexamethasone 1 mg iv q 6 hours. SSKI 6 drops po q 6 hours (started 2 hours after the first dose of PTU). The following day, his thyroid panel results were available and showed TSH was undetectable and his Free T4 was >6 mg/do. A diagnosis of thyroid storm was confirmed. Once his c-spine was cleared by CT scan, the c-collar was removed. A diffusely enlarge thyroid gland was visible on gross inspection. Three days after admission the patient’s heart rate was 92, Temp was 37.3, he was mentating normally, and was able to report a 20 pound weight loss over the preceding 3-months, insomnia and heat intolerance. What precipitated this patient into thyroid storm? What are common precipitants of thyroid storm? MKSAP 16: Question #72: Diagnose thyroid storm *****YOU MAY STOP HERE OR PROCEED TO NEXT CASE***** CASE 72 yo obese female with history of overactive thyroid gland s/p radioactive iodine therapy and hypertension is brought in to the ED by her husband for cough productive of green sputum, lethargy and confusion. Husband reports that cough started about a week ago, but patient has been really weak, unable to get out of bed much and sleeping a lot for the past month. Outpatient medications are levothyroxine and losartan, although patient has not been taking these for at least several months. Patient does not take any over the counter medications, herbs or supplements. Vitals, T 35.2, BP 80/55, HR 70, rr 9, O2 sat 80% on RA. Exam shows an obese female, arouses intermittently but falls back asleep again, unable to answer questions appropriately, appears lethargic and has dry skin and dry mucous membranes. Lungs with bibasilar diminished breath sounds and crackles most notably on R side mid-lung fields. Abdominal exam is normal. Extremities with mild bilateral edema. Neuro exam, patient unable to follow commands, moves all 4 extremities spontaneously, and has slow reflexes. Labs: WC 21, 000, 90% neutrophils, h/h 15/43, plts 230 Na 131, K 3.5, Cl 102, bicarb 25, bun 8, cr 0.7, Glucose 45 CXR shows RLL consolidation and small bilateral pleural effusions. CT head without contrast is negative. Urine toxicology is negative. Patient is admitted for SIRS/Sepsis, and started on appropriate antibiotics for the pneumonia and receives IVF to support blood pressure. Patient’s pneumonia appears to be improving over the next 24 hours as WC decreases to 9,000 and oxygenation improves to 89% on RA. You initially thought that patient’s altered mental status was due to sepsis and or delirium, and therefore expected it to improve over the next 24 hours, although it has not. Patient remains really sleepy, confused and lethargic and this is not a waxing and waning pattern. What is your differential diagnosis for her confusion, sleepiness, delayed reflexes, low BP, low respiratory rate, low sodium, and low glucose? What studies would you send to work this up? Results return as follows: TSH 155 (nl range 0.46 – 4.6) Free T4 0.2 (nl range 0.8 – 2.2) Total T3 <20 (76-101) What is your diagnosis? What precipitated this patient’s presentation? What is the most appropriate initial treatment of this patient? What is the mortality rate in treated vs untreated myxedema coma? MKSAP 16: Question #49: Treat myxedema coma Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111). 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student