Case Study 4 - CANO-ACIO
advertisement

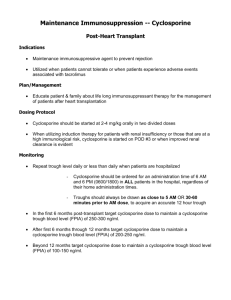
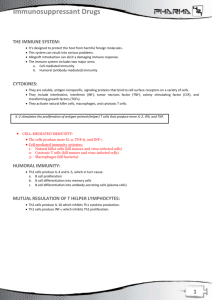
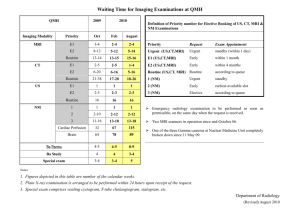
ALERT: THE PRES! HISTORY Mrs. N is a 60 year old post allogeneic hemopoeitic stem cell transplant for myelodysplastic syndrome diagnosed in 2008. In 2011 she underwent a related donor stem cell transplant from her younger sibling. Her recovery during her acute phase post transplant was fairly uncomplicated however she did take a bit longer to engraft and was left with being platelet transfusion dependent every few months. She has been doing well for the last year. Recently she developed frequent episodes of green watery diarrhea with little blood in it and abdominal pain for the past 5 days. After investigations and concerns regarding a possible GI bleed, a colonoscopy was performed. It was determined that she had a grade 1 Graft versus Host Disease (GVHD) of the gut. She is placed on steroids in addition to her Cyclosporine prophylaxis. The green watery diarrhea resolved and she was tapered off the steroids however she remained on her Cyclosporine prophylaxis. Today (4 months later) her son reports in clinic she is having periods of confusion, headache incoordination, stiff neck and visual changes. She was further incontinent of a small amount of urine this a.m. He does not take her to the ER because he knows she has an appointment with her transplant physician at 0900 this a.m. As her nurse you are quite concerned with her and get her into a bed for further assessment with her transplant physician. PHYSICAL SYSTEM General Vital Signs Skin HEENT MSK Nodes Pulmonary CV Abd Extremities Neuro PATIENT FINDINGS Fatigued, Alert and oriented with periods of confusion T-38.3, P-101bpm, RR- 18/min, BP-175/96 Pale Pupils reactive to light, only perceiving light and shadows Not able to count fingers in front of her. Small micro aneurysm in Rt eye Normal No enlarged nodes palpable Lung fields clear upon auscultation Heart sounds normal No organmegaly No bruising or petechiae Intact cranial nerves, strength and sensation equal Question #1 Reviewing her symptoms of confusion, headache, incoordination, stiff neck, visual changes, hypertension, urinary incontinence and knowing that she is platelet dependent, you are concerned she has had a (which diagnosis)? a. Gross Urinary Tract Infection b. Cerebral Hemorrhage c. Hypercalcemic Event d. Cerebral Vascular Accident LABORATORY FINDINGS CBC Test WBC MCV Hct HGB PLTS Neutrophils Eosinophils Basophils Sodium (Na++) Potassium (K+) Chloride (Cl-) Calcium (Ca++) Cyclosporine Patient Results 15.0 100 0.32 102 60 4.4 0.3 0.1 ELECTROLYTES 135 3.7 106 2.42 CYCLOSPORINE 280 CREATININE 141 Normal Values 4.0-11.0 x10E9/L 82-100fL 0.40-0.54L/L 137-180g/L 150-400 x10E9/L 2.0-8.0 x10E9/L 0.0-0.7 x10E9/L 0.0-0.2 x10E9/L 133-145 mmol/L 3.3-5.1 mmol/L 98-111 mmol/L 2.10-2.55 mmol/L 150-400 Creatinine 35-100umol/L Question #2 As Mrs. N’s nurse you receive her above laboratory results and anticipate the following medical orders? a. Type and screen followed by Transfusion of 2units of PRCS ASAP. b. Transfuse 4 units single donor platelets ASAP. c. CT and MRI of the head and Consult Neurology STAT. d. Schirmer's testing today and ophthalmology consult within 2 weeks. You are not surprised the MD would like a STAT MRI, CT of the head and some assistance from their Neurology colleagues to sort out Mrs. N’s sudden onset of confusion, headaches, incontinence, stiff neck, incoordination and visual changes. Question #3 As you are coordinating the CT and MRI with the imaging departments the neurology team completes their consult. They recommend the MRI STAT. However the imaging department is only able to take the patient immediately for her CT. Because of the difficulty obtaining the MRI STAT you: a. Send the patient for the CT. b. Verify the physician’s orders in priority sequence with him, and ensure there is MD to MD communication to ensure the priority test is arranged and completed STAT. c. Follow the advice of the Neuro consult team as that is what they are consulted for. d. Allow the patient to decide. The results of the MRI are called to the transplant physician you are working with. He tells you the MRI is definitely showing edema in Mrs. N’s cortex and parietal lobes causing her to have ocular changes and all of her neurologic symptoms. But what has caused this woman’s edema in her brain? The physician reviews the list of Mrs. N’s medications. 1. 2. 3. 4. Multivitamin One a Day (one daily) Cal Mag standard (two daily in the a.m.) Cyclosporine (100mg twice daily) Dapsone (50mg daily) 5. Senekot (2 tabs at hs) 6. Colace (2 tabs twice daily) 7. Immovane 7.5mg at hs PRN 8. Gravol (50mg every 4-6 hrs PRN) Question #4 As you review the plethora of typical post transplant medications with the physician and knowing the above lab results you anticipate the one medication which is most likely to be the causative agent of her symptoms is: a. Perhaps the steroid she was taking 4 months ago caused her some long term effects. b. Her PJP/PCP prophylaxis must not be working causing her the neurologic symptoms. c. None of them. d. The Cyclosporine is the causative agent in her neurologic symptoms. Pathophysiology Transplant patients are at high risk for developing Posterior Reversible Encephalopathy Syndrome (PRES) as they are exposed to cancer chemotherapy and/or immunosuppressant toxic agents. Cyclosporine is routinely utilized in stem cell transplant recipients as Graft versus Host Disease (GVHD) prophylaxis. It is reported in as high as 10% of patients who take the drug can experience neurotoxicity. This can occur at both elevated and therapeutic blood levels of the drug. The symptoms of neurotoxicity include confusion, visual changes, ataxia and seizures. Cyclosporine neurotoxicity is thought to be a result of endothelial damage in the brain causing edema and encephalopathy syndrome (PRES). Retrospective studies done between 1988 and 2008 indicate PRES has been reported in individuals between the ages of 4 to90 years old with the mean age ranging from 39 t 47 years. There is a marked female predominance among those studied. Posterior reversible encephalopathy syndrome is a constellation of symptoms including hypertension, headache, seizures, altered mental status, and visual disturbances (cortical blindness). Cortical blindness occurs because of damage to the visual pathways. Seizure activity is reported up to 92% of the time. The seizures are rarely isolated and they can occur continuously (status epilepticus lasting longer than 5 minutes) leading to an intensive care unit (ICU) admission. Mechanical ventilation is needed in as high as 35%-40% of patients with PRES for 3-7 days lengthening the mean hospital length of stay to approximately 20 days. Other potential symptoms occurring from PRES include brisk tendon reflexes and weakness or incoordination of the limbs. Although the exact mechanism of PRES is not known, it is thought that the cerebral edema occurs due to increased capillary pressure or failure of the blood brain barrier. The role of CT and MRI is significant in the diagnosis of PRES. MRI is reported as superior to CT as proton density and weighted images show regions of high signal indicating edema. In 1996 Hinchey et al. describe classical symptoms found on MRI as posterior white matter edema found in both hemispheres of the cerebral cortex; however other areas may be affected as well. Hinchey et al. further distinguish PRES from ischemia or infarction by potential causative factors as well as two different types of imaging (diffusion weighted imaging (DWI) and fluid attenuated inversion recovery (FLAIR). Of course encephalopathy can occur because of numerous factors including eclampsia, renal disease, acute hypertension, sepsis, and cytotoxic drugs. The cytotoxic drugs known to induce PRES include: Oxaliplatin, Bevacizumab, Sunitinib, Gemcitabine, Sirolimus and once again Cyclosporine. The syndrome generally has a higher occurrence with intravenous Cyclosporine. However given Mrs. N’s clinical picture Cyclosporine is thought to be the causative agent. Question #5 After the transplant physician educates you on PRES and toxicity that can occur with Cyclosporine you as the nurse anticipate the priority treatment: a. the patient will need a refill for her Cyclosporine b. the patient will be treated with another immunosuppressant c. The Cyclosporine will be discontinued and essential education is needed to alert the patient and family to reporting any increasing symptoms. d. A need to book a follow up MRI. Question #6 As Mrs. N’s BMT nurse you are well aware that there is another lab value that is often reviewed as you assess a cyclosporine level. Which lab value above is commonly considered important when reviewing the cyclosporine level and why? a. WBCs. Cyclosporine is an immunosuppressant that can raise the WBCs. b. Neutrophils. Cyclosporine is an immunosuppressant that attacks neutrophils. c. Calcium. Cyclosporine is a calcineurin inhibitor which can lower calcium levels. d. Creatinine. Cyclosporine is calcineurin inhibitor which can cause renal toxicity. Treatment It is important to treat the underlying cause of PRES as soon as recognized to avoid permanent damage to the affected area of the brain. The use of imaging as mentioned above (CT or MRI) can assist in diagnosis. MRI is considered superior to CT when assessing the edema in the white matter of the brain for a diagnosis of PRES. EEG’s are routinely ordered to assess for nonconvulsive status epilepticus. Lumbar punctures are generally non specific in PRES, however if symptomatology is associated with a fever, analysis of the CSF can be helpful to rule out meningitis. Anticonvulsants are utilized to stabilize status epilepticus and drug levels are monitored closely. Prompt recognition and withdrawal of the agent causing the PRES can reverse the syndrome. Priority for Mrs. N’s treatment included stopping the cyclosporine. She was admitted to hospital for 5 days for Blood pressure control, IV fluids to improve her creatinine and observation until her symptoms resolved. She did not require ICU admission and did not experience any seizures. It was also important to ensure that her platelet count was greater than 90. Although she was not found to have an intracranial hemorrhage it was critical that thrombocytopenia and bleeding did not play a role in furthering her symptoms. She was transfused with HLA matched platelets and asked to have her CBC drawn every 3 days and then to weekly to ensure her platelets remained elevated. After her cyclosporine was discontinued she was placed on an alternate immunosuppressant and a follow up MRI booking was requested to ensure her previous findings were resolving. Regular telephone follow up was provided by the clinic nurse to ensure resolution of her symptoms and that no re-emergence of symptoms occurs. Thorough patient education was provided to assist the patient to manage with the help of her family at home. Contact phone numbers were provided in the event there was an emergency or concerns arose. Question #7 Mrs N contacts you by phone two days after she is released from hospital and asks what she can do to prevent this syndrome from occurring again. You reply with your best response by saying: a. It sounds as if you are worried you did something wrong. There is nothing you did that caused this to happen to you. Your cyclosporine level was within range. Luckily you and your family reported the symptoms promptly and we were able to help you before you developed more complications. b. You did everything wrong. Next time it would be helpful if you report the symptoms earlier. c. You did everything right. We should have been checking of your cyclosporine level regularly. d. You know we cannot predict what will happen in any given situation because sometimes bad things happen to good people. Outcome Complete resolution of Mrs. N’s symptoms occurs. The repeat MRI shows resolution of all edema in the cortex, parietal and white matter of her brain. She is eventually weaned off of all her anticonvulsant medication and blood pressure medication and is monitored with regular blood work and follow-up from the transplant team. Answers 1b 2c 3b 4d 5c 6d 7a References Ezzone, S (2012). Hematopoietic stem cell transplantation: A manual for nursing practice. Oncology Nursing Society, Pittsburgh, PA. 120. Legriel, S., Pico, F., and Azoulay, E. (2011). Annual update in intensive care and emergency medicine. J.L. Vincent (ed.). Springer Science and Business Media. 631-653. Legriel, S, Schraub, O., Azoulay, E., Hantson, P., Magalhaes, E., Coquet, I., Bretonniere, C., Gilhodes, O., Anguel, N., Megarbane, B., Benayoun, L., Schnell, D., Plantefeve, G., Charpentier, J., Argud, L., Mourvillier, B., Galbois, A., Chalumeau-Lemoine, L., Rivoal, M., Durand, F., Geffroy, A., Simon, M., Stoclin, A., Pallot, J.L., Arbelot, C., Nyunga, M., Lesieur, O., Troche, G., Bruneel, F., Cordoliani, Y.S., Bedos, J.P., and Pico, F. (2012). Determinants of Recovery from Severe Posterior Reversible Encephalopathy Syndrome. PLoS ONE, 7(9), e44534, 1-11. Shah, R., Kubisz-Pudelko, A., and Reid, J. (2014). Posterior reversible encephalopathy syndrome following an inadvertent dural puncture during an emergency laparotomy for ischemic colitis-a case report. Local and Regional Anesthesia, 7, 1-4.