Nursing Simulation: Diabetes & Homeless Veteran Scenario
advertisement
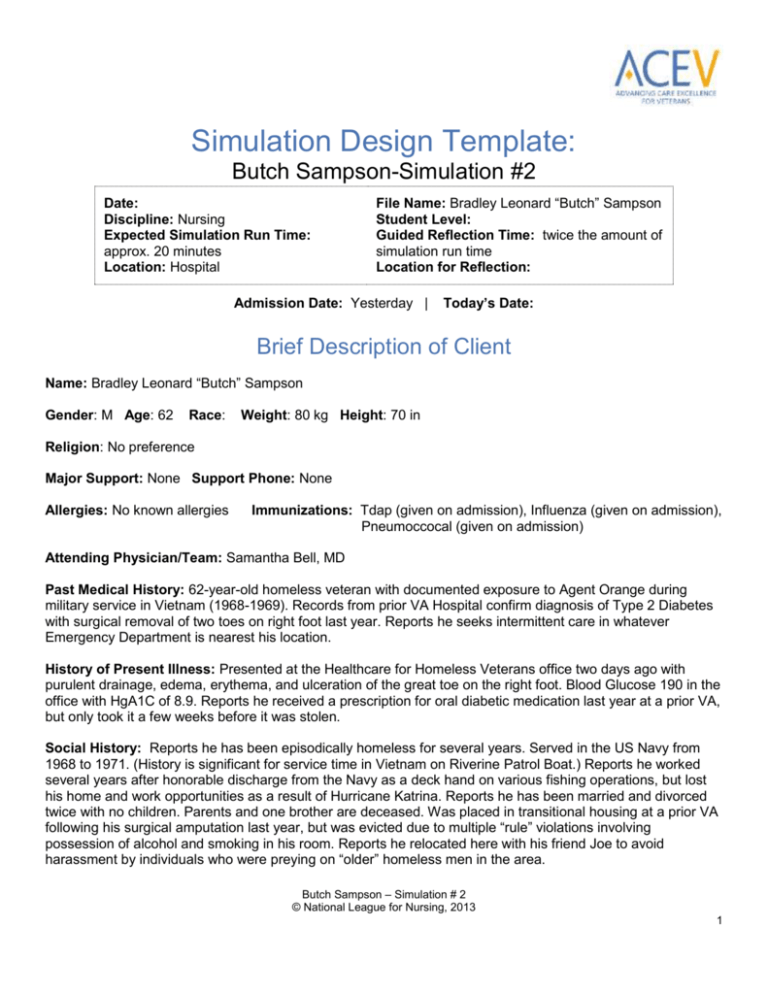
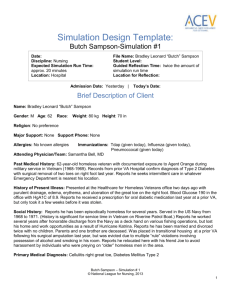
Simulation Design Template: Butch Sampson-Simulation #2 Date: Discipline: Nursing Expected Simulation Run Time: approx. 20 minutes Location: Hospital File Name: Bradley Leonard “Butch” Sampson Student Level: Guided Reflection Time: twice the amount of simulation run time Location for Reflection: Admission Date: Yesterday | Today’s Date: Brief Description of Client Name: Bradley Leonard “Butch” Sampson Gender: M Age: 62 Race: Weight: 80 kg Height: 70 in Religion: No preference Major Support: None Support Phone: None Allergies: No known allergies Immunizations: Tdap (given on admission), Influenza (given on admission), Pneumoccocal (given on admission) Attending Physician/Team: Samantha Bell, MD Past Medical History: 62-year-old homeless veteran with documented exposure to Agent Orange during military service in Vietnam (1968-1969). Records from prior VA Hospital confirm diagnosis of Type 2 Diabetes with surgical removal of two toes on right foot last year. Reports he seeks intermittent care in whatever Emergency Department is nearest his location. History of Present Illness: Presented at the Healthcare for Homeless Veterans office two days ago with purulent drainage, edema, erythema, and ulceration of the great toe on the right foot. Blood Glucose 190 in the office with HgA1C of 8.9. Reports he received a prescription for oral diabetic medication last year at a prior VA, but only took it a few weeks before it was stolen. Social History: Reports he has been episodically homeless for several years. Served in the US Navy from 1968 to 1971. (History is significant for service time in Vietnam on Riverine Patrol Boat.) Reports he worked several years after honorable discharge from the Navy as a deck hand on various fishing operations, but lost his home and work opportunities as a result of Hurricane Katrina. Reports he has been married and divorced twice with no children. Parents and one brother are deceased. Was placed in transitional housing at a prior VA following his surgical amputation last year, but was evicted due to multiple “rule” violations involving possession of alcohol and smoking in his room. Reports he relocated here with his friend Joe to avoid harassment by individuals who were preying on “older” homeless men in the area. Butch Sampson – Simulation # 2 © National League for Nursing, 2013 1 Primary Medical Diagnosis: Cellulitis right great toe, Diabetes Mellitus Type 2 Surgeries/Procedures & Dates: Surgical debridement of right great toe yesterday Nursing Diagnoses: Knowledge deficit related to self-care of affected foot, medications; alteration in health maintenance related to Diabetes Mellitus; impaired physical mobility related to surgical intervention to foot Psychomotor Skills Required Prior to Simulation Cognitive Activities Required Prior to Simulation [i.e. independent reading (R), video review (V), computer simulations (CS), lecture (L)] Review sample VA description of Transitional Housing. http://www.portland.va.gov/CRS/THousing.asp Review care of patients with Type 2 Diabetes in textbook, including diet and medications. Brehove, T., Joslyn, M., Morrison, S., Strehlow, A. J., & Wismer, B. (2007). Adapting your practice: Treatment and recommendations for homeless patients with diabetes mellitus. Nashville: Health Care for the Homeless Clinicians Network. http://www.nhchc.org/wpcontent/uploads/2011/09/DiabetesMellitus.pdf Department of Veterans Affairs. (2012). Veteran diseases associated with Agent Orange. http://www.publichealth.va.gov/exposures/agentorange/diseases.asp Swift, C. S., & Boucher, J. L. (2005). Nutrition care for hospitalized individuals with diabetes. Diabetes Spectrum, 18(1), 34-88. doi: 10.2337/diaspect.18.1.34 http://spectrum.diabetesjournals.org/content/18/1/34.full.pdf+html Simulation Learning Objectives General Objectives 1. 2. 3. 4. 5. 6. 7. 8. 9. Practice standard precautions throughout the exam. Employ effective strategies to reduce risk of harm to the client. Assume the role of team leader or member. Perform a focused physical assessment noting abnormal findings. Recognize changes in patient symptoms and/or signs of patient compromise. Perform priority nursing actions based on clinical data. Reassess/monitor patient status following nursing interventions. Perform within scope of practice. Demonstrate knowledge of legal and ethical obligations. Butch Sampson – Simulation # 2 © National League for Nursing, 2013 2 10. Communicate with client in a manner that illustrates caring for his/her overall well-being. 11. Communicate appropriately with physician and/or other healthcare team members in a timely, organized, patient-specific manner. Simulation Scenario Objectives 1. 2. 3. 4. Employ therapeutic communication. Assess knowledge of self-care for Type 2 Diabetes including diet, medications, and care of foot. Complete medication reconciliation. Provide discharge teaching. References, Evidence-Based Practice Guidelines, Protocols, or Algorithms Used for This Scenario: American Diabetes Association. (2012). Standards of medical care in diabetes-2012. Diabetes Care 35(Supp 1), s11-s63. doi: 10.2337.dc12-s011. Beaulieu, A., & Fessele, K. (2003). Agent Orange: Management of patients exposed in Vietnam. Clinical Journal of Oncology Nursing, 7(3). doi: 10.1188/03.CJON.320-323. Brehove, T., Joslyn, M., Morrison, S., Strehlow, A. J., & Wismer, B. (2007). Adapting your practice: Treatment and recommendations for homeless patients with diabetes mellitus. Nashville: Health Care for the Homeless Clinicians Network. http://www.nhchc.org/wpcontent/uploads/2011/09/DiabetesMellitus.pdf Department of Veterans Affairs. (2012). Veteran diseases associated with Agent Orange. http://www.publichealth.va.gov/exposures/agentorange/diseases.asp Fargo, J., Metraux, S., Byrne, T., Muley, E., Montgomery, A. E., Jones, H., & Culhane, D. (2012). Prevalence and risk of homelessness among US Veterans. Prevent Chronic Disease, 9, 110-112. doi: http://dx.doi.org/10.5888/pcd9.110112 Infectious Diseases Society of America. (2012). 2012 Infectious Diseases Society of America clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clinical Infectious Diseases 54. E132-e173. doi: 10.1093/cid/cis346 Nooe, R. M., & Patterson, D. A. (2010). The ecology of homelessness. Journal of Human Behavior in the Social Environment, 20 (2), 105-152. http://dx.doi.org/10.1080/10911350903269757 Butch Sampson – Simulation # 2 © National League for Nursing, 2013 3 O’Toole, T. P., Conde-Martel, A., Givvon, J. L., Hanusa, B. H., & Fine, M. J. (2003). Health care of homeless veterans. Why are some individuals falling through the safety net? Journal of General Internal Medicine, 18, 929-933. Swift, C. S., & Boucher, J. L. (2005). Nutrition care for hospitalized individuals with diabetes. Diabetes Spectrum, 18(1), 34-88. doi: 10.2337/diaspect.18.1.34 http://spectrum.diabetesjournals.org/content/18/1/34.full.pdf+html Fidelity (choose all that apply to this simulation) Setting/Environment: ER Med-Surg Peds ICU OR / PACU Women’s Center Behavioral Health Home Health Pre-Hospital Other: Medications and Fluids: IV Fluids: Oral Meds: see chart IVPB: IV Push: IM or SC: Diagnostics Available: Labs X-rays (Images) 12-Lead EKG Other: Simulator Manikin/s Needed: Standardized patient or moderate fidelity or high fidelity manikin. Props: Dressing covering right great toe. Wheelchair, cane and bag with belongings in room. Equipment Attached to Manikin: IV tubing with primary line fluids running at mL/hr Secondary IV line running at mL/hr IV pump Foley catheter mL output PCA pump running IVPB with running at mL/hr 02 Monitor attached ID band Other: Documentation Forms: Physician Orders Admit Orders Flow sheet Medication Administration Record Kardex Graphic Record Shift Assessment Triage Forms Code Record Anesthesia / PACU Record Standing (Protocol) Orders Transfer Orders Other: see chart materials Recommended Mode for Simulation: (i.e. manual, programmed, etc.) Mode will not change for this scenario. Simulator may be set manually or programmed or this Butch Sampson – Simulation # 2 © National League for Nursing, 2013 4 Equipment Available in Room: Bedpan/Urinal Foley kit Straight Catheter Kit Incentive Spirometer Fluids IV start kit IV tubing IVPB Tubing IV Pump Feeding Pump Pressure Bag 02 delivery device (type) Crash cart with airway devices and emergency medications Defibrillator/Pacer Suction Other: dressing change supplies; compression stockings simulation may be conducted with a standardized patient. Roles/Guidelines for Roles: Primary Nurse Secondary Nurse Clinical Instructor Family Member #1 Family Member #2 Observer/s Recorder Physician/Advanced Practice Nurse Respiratory Therapy Anesthesia Pharmacy Lab Imaging Social Services Clergy Unlicensed Assistive Personnel Code Team Other: Important Information Related to Roles: Student Information Needed Prior to Scenario: Has been oriented to simulator Understands guidelines /expectations for scenario Has accomplished all pre-simulation requirements All participants understand their assigned roles Has been given time frame expectations Other: Butch Sampson – Simulation # 2 © National League for Nursing, 2013 5 Report Students Will Receive Before Simulation Time: 1100 Situation: Bradley Leonard Sampson is a 62-year-old patient of Dr. Bell. He prefers to be called “Butch.” He was admitted 3 days ago for cellulitis of right great toe. He had a debridement of his right great toe and he was treated with IV antibiotics. Background: Butch has Diabetes Mellitus Type 2, but because of his chronic and episodic homelessness, he has had difficulty managing this condition. He is a Navy veteran with known Agent Orange exposure from the Vietnam War. He says after he was discharged he worked as a deck hand for several years with various fishing operations, but lost his home and job in Hurricane Katrina. He has no known relatives. He says his parents and brother are deceased and although he was married and divorced twice he has no known children. He is being discharged today to transitional housing as part of a VA program and has been assigned a case manager. Dr. Bell has also ordered home health and PT visits for follow-up care for his diabetic foot ulcer. He is a smoker - 1 pack a day x40 years and consumes alcohol regularly. These lifestyle issues have created a problem for him in the past in previous transitional housing. His fasting blood sugar today was 130. It has improved from 190 on admission with control of the infection, balanced diet and use of Metformin. Assessment: He is willing to give the transitional housing unit a try and will also consider permanent housing if it becomes available through the VA program. He’s just getting ready for discharge. His social worker, Bill, will take him to his new place. I just took his discharge vital signs and they are stable. I also re-dressed his toe this morning and the surgical wound was pink and moist with scant serous drainage. Recommendation: Go over the discharge instructions that are on his chart and see if he understands all of them. Please complete the medication reconciliation form too. Make sure he gets the surgical shoe before he leaves. Significant Lab Values: refer to chart Physician Orders: refer to chart Home Medications: refer to chart Scenario Progression Outline Timing (approx.) 0-5 min Manikin Actions Expected Interventions May Use the Following Cues Resting in wheelchair dressed in street clothes with right foot elevated on a pillow. Dressing dry and intact with no visible drainage. Role member providing cue: Butch Cue: If students Greet patient, check ID. Introduce self. Wash hands. Butch Sampson – Simulation # 2 © National League for Nursing, 2013 6 Has cane and belongings in bag. BP 120/80, Pulse 72, Resp. 16, Temp 98.6 F “You can just call me Butch. I’m ready to get out of here! My case manager said he’d give me a ride to the new place.” Establish therapeutic communication (interest and concern). Explain reason for assessments. forget to introduce themselves, Butch can say, “Who are you and what do you want with me?” Ask Butch to describe how he will take his medications. May offer other written materials about medications. Complete medication reconciliation form. Role member providing cue: Cue: Assess understanding of diet by asking Butch what he knows about food choices. Can provide additional resources about diet. Role member providing cue: Cue: Discuss reasons for elevation of leg and limitations on activity. Discuss home visits and follow up at Role member providing cue: Cue: Answers questions appropriately. If students ask personal questions about why he is homeless or specifics about his military combat patient will say, “That’s none of your business.” 5-10 min “I take that antibiotic horse pill three times a day, right? Eat something with it, too.” “I’m supposed to take that diabetes pill—Metformin—twice a day before breakfast and before supper.” 10-15 min 15-20 min “The dietician said I should try to have a half a plate with vegetables and fruit. A quarter of a plate with some kind of meat and a quarter of a plate with something like potatoes, rice, or noodles. She also gave me this sheet for keeping track.” “I know I need to take better care of myself, but being cooped up inside all day just doesn’t seem like any way to live.” “OK, I’m ready to get out of here. Need to stop downstairs and have a smoke. They say at least I can Butch Sampson – Simulation # 2 © National League for Nursing, 2013 7 smoke at this new place outside on the porch.” Healthcare for Homeless Veterans (HCVC) clinic. Debriefing/Guided Reflection Questions for This Simulation (Remember to identify important concepts or curricular threads that are specific to your program) 1. How did you feel throughout the simulation experience? 2. Describe the objectives you were able to achieve. 3. Which ones were you unable to achieve (if any)? 4. Did you have the knowledge and skills to meet objectives? 5. Were you satisfied with your ability to work through the simulation? 6. To Observer: Could the nurses have handled any aspects of the simulation differently? 7. Have you ever served in the military, or do you know someone who has? If so, how did your personal experience with these individuals influence your participation in the scenario? 8. If you were able to do this again, how could you have handled the situation differently? 9. What did the group do well? 10. What did the team feel was the primary nursing diagnosis? 11. How were physical and mental health aspects interrelated in this case? 12. What were the key assessments and interventions? 13. Is there anything else you would like to discuss? Specific Debriefing Questions for this Scenario: 1. Do you have any concerns about Butch’s ability to manage his own care? 2. What are Butch’s strengths? 3. What other members of the health care team could help to manage Butch’s care? Butch Sampson – Simulation # 2 © National League for Nursing, 2013 8