Using Haddon`s Matrix to Identify Risks and Prevention Strategies
advertisement
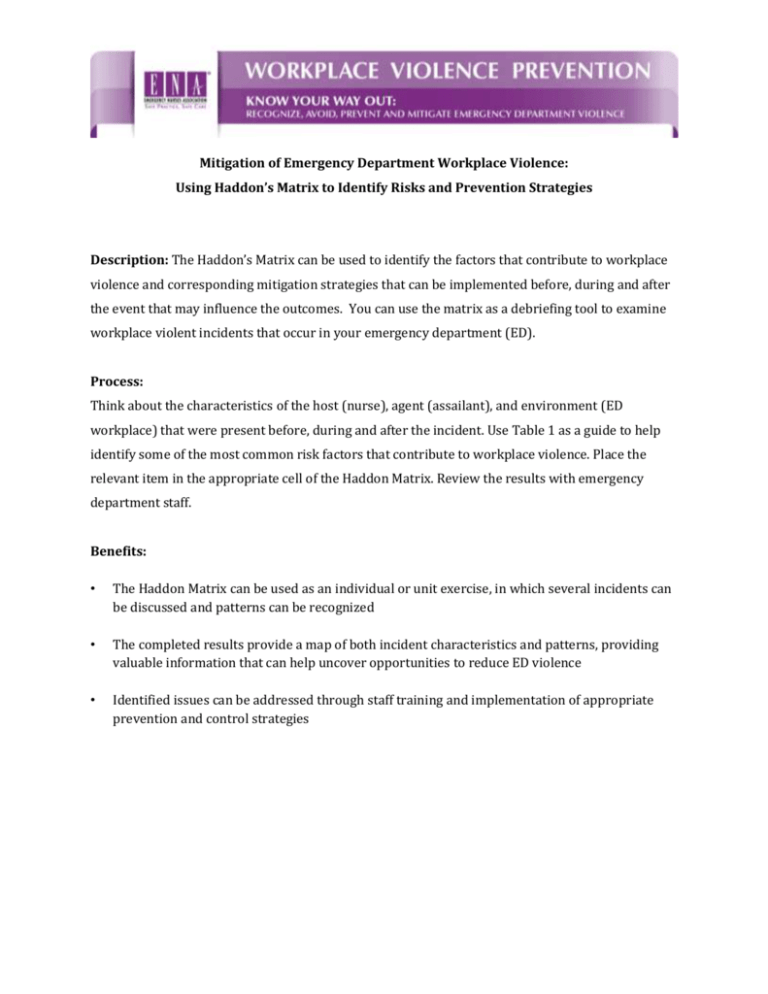
Mitigation of Emergency Department Workplace Violence: Using Haddon’s Matrix to Identify Risks and Prevention Strategies Description: The Haddon’s Matrix can be used to identify the factors that contribute to workplace violence and corresponding mitigation strategies that can be implemented before, during and after the event that may influence the outcomes. You can use the matrix as a debriefing tool to examine workplace violent incidents that occur in your emergency department (ED). Process: Think about the characteristics of the host (nurse), agent (assailant), and environment (ED workplace) that were present before, during and after the incident. Use Table 1 as a guide to help identify some of the most common risk factors that contribute to workplace violence. Place the relevant item in the appropriate cell of the Haddon Matrix. Review the results with emergency department staff. Benefits: • The Haddon Matrix can be used as an individual or unit exercise, in which several incidents can be discussed and patterns can be recognized • The completed results provide a map of both incident characteristics and patterns, providing valuable information that can help uncover opportunities to reduce ED violence • Identified issues can be addressed through staff training and implementation of appropriate prevention and control strategies Phase Host Agent/Vehicle Workplace Environment (Nurse, Security (Assailant, Weapons) (Structures, Cultural Personnel) Pre-event (e.g., preassault) Event (e.g., during assault) Post-event (e.g., postassault) Norms, and Policies) TABLE 1: RISK FACTORS FOR ED WORKPLACE VIOLENCE Host Agent/Vehicle Workplace Environment (Personal Characteristics) (Patient & Visitor Behaviors) (Physical, Social, Cultural Factors) Lack of recognition of dangerous situations/patients Limited help-seeking Little or no use of deescalation skills Lack of confidence in handling difficult patients Lingering trauma, PTSD or history of personal violence Pain or other physical symptoms; disability Loss of pay or reduced hours; absenteeism No incident report filed Fear of retribution by employer or colleagues Slow response of facility to acknowledge and respond STAMP behaviors Crowded conditions Escalating aggression Patient boarding and long wait times Difficulty accepting limitsetting requests Inadequate security Resistance to health care Inadequate safety controls Potential for poor patient outcomes Poorly lit, isolated areas History of violence Alcohol and/or drug use Threatening gestures Verbal threats Access to weapons or threatening use of weapons Emotional state of patient’s family members and visitors Unrestricted public access Small exam rooms Staffing shortages No zero tolerance or safety policies Workplace bullying Culture of tolerance Inadequate staff training Family conflict Lack of access to safety devices Lack of support from peers Prolonged wait times Attrition from nursing workforce Arrest or removal from premises Refusal from administrators to report and respond to incident Legal prosecution Reduced productivity Impact on staff retention